The Miracle That Wasn’t: Hydroxychloroquine and the Pandemic Gamble

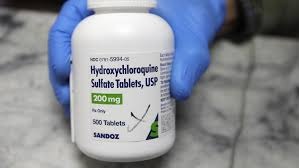
In early 2020, as COVID-19 raced across the globe, the whole came on a standstill, movement restricted, lives lost and a lot of conspiracytheory about the pandemic, it was a remarkable one that shaped the lives of individuals, institutions ad government. But amidst all of this, one drug captured headlines with dizzying promise — hydroxychloroquine (HCQ). Touted by some as a miracle cure, it was fast-tracked into clinical use, stockpiled by governments, and thrust into the heart of a political spectacle. But as months turned into years, the initial hope unraveled under the weight of rigorous science: the miracle never materialized, and the gamble came with real costs.
The Spark: From Malaria Pill to Global Hype
Hydroxychloroquine was far from new. For decades, it had been widely used to treat malaria and autoimmune conditions like lupus and rheumatoid arthritis. Its pharmacological safety at known doses made it an attractive candidate for repurposing when the coronavirus crisis hit. Early in vitro (lab) experiments suggested HCQ might inhibit SARS-CoV-2 replication in cell cultures, offering a tantalizing possibility.
By March 2020, desperate for therapeutic options, researchers began small trials and observational studies. One of the earliest high-profile reports came from France, led by Didier Raoult’s team, which claimed that HCQ, especially when combined with the antibiotic azithromycin, drastically reduced viral load in COVID patients. That report, though small and methodologically questionable, lit a global firestorm.
The media seized upon these optimistic results. In a climate of fear and uncertainty, the promise of a cheap, existing drug as a potential cure resonated. Soon, politicians joined in. In the United States, President Donald Trump publicly endorsed HCQ, calling it a “game changer,” and instructed the government to stockpile millions of doses.
In March 2020, the U.S. Food and Drug Administration (FDA) granted Emergency Use Authorization (EUA) for hydroxychloroquine in hospitalized COVID-19 patients, allowing its deployment under certain conditions despite limited evidence.
Rising Pressure: Prescriptions, Politics, and Public Faith
The enthusiasm translated into widespread prescribing. In the U.S., hydroxychloroquine prescriptions skyrocketed. Many of them came from physicians who had never prescribed the drug before, specialists outside of malaria or rheumatology fields. In March 2020 alone, non-routine prescribers issued tens of thousands of new HCQ prescriptions.
Social media played a dramatic role in amplifying the hype. Hashtags like #HCQ, #miracledrug, and #COVIDcure circulated heavily. Analysts later documented how polarized debates over HCQ’s efficacy dominated Twitter discourse. Many users, desperate for hope, accepted early claims without scrutinizing the science.

At the same time, other scientists warned that reports were preliminary and flawed. But their caution was drowned out in the roar of optimism and political endorsement.
Cracks in the Foundation: Doubts and Early Red Flags
As use expanded, so did skepticism. One of the first major challenges came in April 2020, when analyses noted serious methodological flaws in the French study: small sample sizes, lack of randomization, missing controls, and selective reporting.
Further, safety concerns began to emerge. HCQ is known to carry cardiac risk — particularly arrhythmias, especially when used in higher or off-label doses. Combined with azithromycin, that risk increased. The FDA issued a safety warning on April 24, 2020, cautioning that HCQ use for COVID-19 could lead to serious heart rhythm problems.
Meanwhile, real-world observational studies began reporting mixed or negative results. A high-profile observational cohort in New York (Geleris et al.) found no clear association between HCQ use and improved outcomes in hospitalized patients.
In the background, the WHO’s large Solidarity trial, and the U.K.’s RECOVERY trial, incorporated HCQ among their treatment arms to test it rigorously in large populations. The stakes were rising.
Collapse: Clinical Trials, Revoked Authorizations, and Failures
By mid-2020, results from large, controlled trials began to land and they were stark.
In June 2020, the RECOVERY trial announced that hydroxychloroquine provided no clinical benefit in hospitalized COVID-19 patients. It failed to reduce mortality, improve recovery, or shorten hospital stays.
Around the same time, the FDA officially rescinded its Emergency Use Authorization for HCQ, declaring that “based on new information … it is no longer reasonable to believe that oral formulations … may be effective” and that known and potential risks outweigh benefits.
Globally, other trials and meta-analyses echoed the verdict: HCQ conferred little or no benefit on mortality or other clinical outcomes, but increased adverse events, especially cardiac.
Complicating matters, some early foundational studies used to justify HCQ’s adoption were later found to be deeply flawed. In December 2024, a key French study from 2020 was formally retracted due to methodological and ethical concerns. It has been one of the most cited studies promoting HCQ.
By late 2020 and early 2021, most national health agencies and clinical guidelines recommended against HCQ for COVID-19, except in clinical trials. The global promise had crumbled.
Fallout: Lives, Trust, and Lessons
The hydroxychloroquine saga leaves a complicated legacy, not just scientific, but social, political, and human.
Missed Opportunity Costs & Health Risks
Millions took HCQ early in the pandemic, often outside of strict trial settings. Some suffered serious side effects: cardiac arrhythmias, complications from drug interactions, and more. Retrospective analyses have even estimated “excess mortality” in some settings tied to HCQ use, though these estimates remain controversial and uncertain.
The resources and public attention devoted to HCQ may also have diverted focus from more promising therapeutic pathways and trials. That “miracle” detour consumed time, money, and public confidence.
Erosion of Trust in Science & Institutions
The speed at which HCQ was democratized into public discourse, amplified by celebrities, politicians, and social media, blurred the lines between scientific caution and overreach. When the drug failed to deliver, trust in medical institutions, public health agencies, and even peer review took a hit.
Some scientists argue that HCQ’s trajectory offered a cautionary tale: that in moments of crisis, the rigor of science must not be sacrificed for speed. Rapid publication, data sharing, and open debate are crucial, but they must be paired with skepticism and transparency.
Future Implications for Pandemic Response
Several lessons emerge:
Avoid excessive reliance on preliminary results.Single small studies should be treated as hypothesis-generating, not definitive.
Guard scientific integrity. Retractions of influential studies erode credibility.
Keep politics at bay. The political framing of HCQ intensified pressure on scientists and regulators, complicating objective evaluation.
Structure strong, adaptive trials. The existence of large adaptive trials like RECOVERY and Solidarity was critical to debunking the HCQ myth demonstrating that well-designed trials are feasible, even in crisis.
Retrospective: Why the Miracle Never Was
Looking back, why did hydroxychloroquine’s initial promise fail so spectacularly? The answer lies in several intersecting failures:
Overinterpretation of lab findings. What works in petri dishes often fails in complex human physiology.
Small, biased trials. Early studies lacked rigor, no randomization, no masking, small sample sizes, yet they were globally amplified.
Safety under-considered. Known risks, especially cardiac, were not weighed sufficiently in the rush to repurpose.
Political and social turbocharging. External pressure and media hype outpaced cautious scientific process.
Sluggish correction. Even after negative trials emerged, some advocates refused to concede, prolonging confusion.
The “miracle” turned out to be more of a cautionary tale — a potent reminder that in medicine, miracles are rare, and careful proof matters more than hope.
You may also like...
When Sacred Calendars Align: What a Rare Religious Overlap Can Teach Us

As Lent, Ramadan, and the Lunar calendar converge in February 2026, this short piece explores religious tolerance, commu...
Arsenal Under Fire: Arteta Defiantly Rejects 'Bottlers' Label Amid Title Race Nerves!

Mikel Arteta vehemently denies accusations of Arsenal being "bottlers" following a stumble against Wolves, which handed ...
Sensational Transfer Buzz: Casemiro Linked with Messi or Ronaldo Reunion Post-Man Utd Exit!

The latest transfer window sees major shifts as Manchester United's Casemiro draws interest from Inter Miami and Al Nass...
WBD Deal Heats Up: Netflix Co-CEO Fights for Takeover Amid DOJ Approval Claims!

Netflix co-CEO Ted Sarandos is vigorously advocating for the company's $83 billion acquisition of Warner Bros. Discovery...
KPop Demon Hunters' Stars and Songwriters Celebrate Lunar New Year Success!

Brooks Brothers and Gold House celebrated Lunar New Year with a celebrity-filled dinner in Beverly Hills, featuring rema...
Life-Saving Breakthrough: New US-Backed HIV Injection to Reach Thousands in Zimbabwe

The United States is backing a new twice-yearly HIV prevention injection, lenacapavir (LEN), for 271,000 people in Zimba...
OpenAI's Moral Crossroads: Nearly Tipped Off Police About School Shooter Threat Months Ago
ChatGPT-maker OpenAI disclosed it had identified Jesse Van Rootselaar's account for violent activities last year, prior ...
MTN Nigeria's Market Soars: Stock Hits Record High Post $6.2B Deal

MTN Nigeria's shares surged to a record high following MTN Group's $6.2 billion acquisition of IHS Towers. This strategi...