5 Most Dangerous Medical Trials in History

Most people meet medicine at its polished end point. A pill that works, a vaccine that saves lives, or a treatment that feels like a routine. What we rarely see is the brutal learning curve behind it.
Every breakthrough has a backstory. Some are careful and ethical. Others are dark enough that they permanently changed the rules of science. The dark uncomfortable truth many are unaware of is that medicine only learned to protect patients after failing them.
Before we talk about the worst trials in history, one question matters.
Why Do Medical Trials Exist?
Medical trials are not carried out to experiment on people for curiosity’s sake. They exist because the human body refuses to behave like a spreadsheet.
A drug can look perfect in a lab and still harm real people. Animal testing can pass, and humans can still react violently. Trials exist to answer four non-negotiable questions: Is it safe? Does it work? For whom? And at what cost?
They are meant to prevent harm before it becomes widespread. They determine dosage, uncover side effects, expose long-term risks, and stop ineffective treatments from entering hospitals.
Every cancer drug, vaccine, and surgical technique used today passed through this system.
The problem has never been medical trials themselves. The problem has been how power, race, poverty, and urgency distort who gets protected and who gets sacrificed.
That distortion is where history gets ugly.
5 Most Dangerous Medical Trials in History
Modern medicine saves lives every day, but its progress is stained by experiments that cause irreversible harm. Some trials were built on deception.
Others ignored consent entirely. Many exploited people who had little power to refuse.
These are not exaggerated stories or internet myths. They are documented events that forced the world to rethink how medical research should work.
This was not a scientific mistake, it was a moral failure.
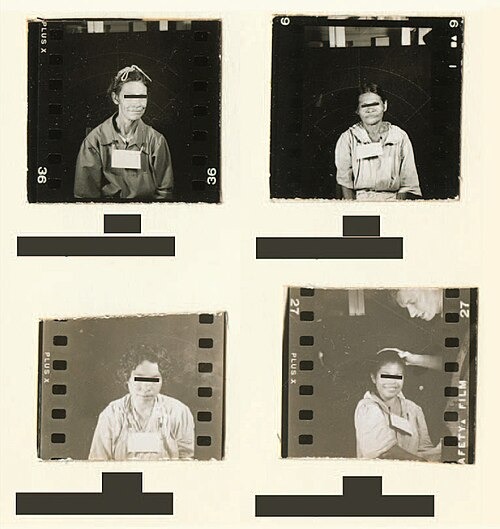
From 1932 to 1972, hundreds of Black men in Alabama were enrolled in what they were told was free healthcare. In reality, doctors were observing untreated syphilis. The men were never told they were sick. When penicillin became the proven cure, it was deliberately withheld.

Men died from preventable complications, their partners were infected, and children were born with congenital syphilis. The study ran for forty years and ended only after a whistleblower exposed it.
Tuskegee didn’t just harm bodies,it broke trust. Decades later, its shadow still affects how Black communities interact with healthcare systems.
If Tuskegee was neglected, this was an intentional infection.
In the 1940s, U.S. researchers deliberately infected prisoners, psychiatric patients, and soldiers in Guatemala with syphilis and gonorrhea. Consent was never obtained. Many participants had no idea they were part of an experiment.
Some were treated, many were not, while several died.
The truth stayed buried until 2010. A formal apology followed. Justice never really did.
In 1996, a meningitis outbreak hit Kano, Nigeria. During the crisis, children were given an experimental antibiotic called Trovan.
History
Rewind the Stories that Made Africa, Africa
A Journey Through Time, Narrated with Insight.
Parents later said they were not properly informed that the drug was experimental or that established treatments were available. Several children died. Others were left with lifelong disabilities.
The case triggered lawsuits, global outrage, and a settlement years later. It also exposed a pattern that still exists today: high-risk trials are more likely to happen where poverty limits resistance.
This trial proved that even modern medicine can spiral out of control.
In 2006, six healthy volunteers in the UK received a new immune system drug during an early-stage trial. Within an hour, all six suffered extreme immune reactions. Their organs began to fail. Intensive care became a race against death.
Some survived with permanent damage, including amputations. The drug had passed animal testing. Human biology responded differently.
The incident forced regulators worldwide to rethink how first-in-human trials are designed.
Thalidomide was marketed in the late 1950s as a safe cure for morning sickness. It was prescribed to pregnant women across Europe, Australia, and parts of Africa.
The outcome was catastrophic.
RECOMMENDED READ: The Rookie FDA Doctor Who Saved Hundreds of America’s Babies From Birth Defect Catastrophe

More than 10,000 babies were born with missing limbs, malformed organs, and severe disabilities. The drug had never been adequately tested for pregnancy risks.
This tragedy directly shaped modern drug approval laws and mandatory clinical trial systems.
Conclusion
History
Rewind the Stories that Made Africa, Africa
A Journey Through Time, Narrated with Insight.
These cases are not ancient history. They explain why medicine now insists on informed consent, ethics boards, phased testing, and transparency. Every safety rule exists because someone was harmed before it did.
Medical trials are necessary. Ethical trials are non-negotiable. And history proves what happens when that line is crossed.
You may also like...
Osimhen Unleashes Fury & Victory: The Galatasaray-Juventus Saga Unpacked!

Victor Osimhen's decisive goal led Galatasaray to a dramatic 7-5 aggregate victory over Juventus, securing their spot in...
Netflix Sensation 'Bridgerton' Season 4 Part 2 Sparks Debate with Bold Moves and Familiar Flaws

Bridgerton Season 4 Part 2 delves deeper into the forbidden romance of Benedict and Sophie, alongside a myriad of family...
Berlin Film Festival Rocked: Staff Rally Behind Chief Tricia Tuttle Amid Future Uncertainty

Berlin Film Festival director Tricia Tuttle faces an uncertain future as its governing body failed to decide on her cont...
Director Jafar Panahi Unveils The Secret Behind His Oscar-Nominated Film's Haunting End

Jafar Panahi's latest clandestine film, "It Was Just an Accident," explores the moral dilemmas of former political priso...
The 'Scrubs' Crew Spills Why Revival Needed a 'Resetting'

The beloved medical comedy <i>Scrubs</i> returns with a 30-minute revival, reuniting Zach Braff and Donald Faison as J.D...
Art World Cheers: Ken Nwadiogbu Crowned 2026 Young Generation Art Award Winner in Berlin
Nigerian-born, London-based artist Ken Nwadiogbu has been honored with the 2026 Young Generation Art Award, triumphing o...
Damson Idris Revs Up! British-Nigerian Actor Becomes Formula 1 Global Ambassador

British-Nigerian actor Damson Idris has been named Formula 1’s Global Brand Ambassador, a role that recognizes his deep ...
Cross-Border Rail Roars Back: TAZARA Link Between Tanzania and Zambia Resumes After Eight-Month Halt

TAZARA has resumed its cross-border passenger train services between Tanzania and Zambia after an eight-month suspension...