NHS ADHD Crisis Deepens: System in Chaos as Spending Skyrockets Amid Unregulated Clinic Boom

The National Health Service (NHS) is grappling with a significant financial challenge in its attention deficit hyperactivity disorder (ADHD) services, reportedly overspending by £164 million annually. A Guardian investigation reveals that total spending on these services is projected to more than double existing budgets, potentially reaching £314 million by April 2026 against a budget of £150 million. This substantial overspend, covering 32 of England’s 42 Integrated Care Boards (ICBs), raises concerns about potential cuts to other vital healthcare services.
A major contributing factor to this overspending is the escalating reliance on private providers for ADHD assessments and care. Data from 19 ICBs indicates that spending on private ADHD services has more than tripled in just three years, soaring from £16.3 million in 2022-23 to £58 million last year. Critics argue that this rapid increase highlights an under-regulated market where private companies are making substantial profits. Research from the Centre for Health and the Public Interest (CHPI) found one company, recently acquired by a private equity firm, reporting profit margins of 33% over the past two years, largely from NHS services.
The surge in demand for ADHD assessments has reached unprecedented levels, with over half a million people currently on NHS waiting lists. Increased awareness of the condition, coupled with stretched NHS resources, has driven many patients towards private pathways. This includes the 'right-to-choose' pathway, which allows patients to select private providers to bypass lengthy local waitlists. However, the CHPI report warns that this system is particularly attractive to business investors due to its easy accessibility; a single contract allows a company to treat patients nationwide with no cap on earnings, preventing local NHS bodies from restricting patient numbers or costs.
Concerns are mounting regarding the quality and safety of care provided by some private clinics. Many NHS adult ADHD services have ceased accepting new patients, exacerbating the reliance on private options. Experts have highlighted the unreliability of some private assessments and significant issues with continuity of care post-diagnosis. For instance, 14 companies providing NHS-funded ADHD assessments were not registered with the Care Quality Commission (CQC), and a further 19 companies offered neurodiversity services worth £1.9 million over three years without any NHS contract, undermining proper accountability.
Tragic cases underscore the risks associated with fragmented care. In one instance, a coroner issued a prevention of future deaths report following the suicide of 27-year-old Sheridan Pickett. Pickett died after receiving an online ADHD diagnosis and stimulant medication from a private clinic. Despite later hospital admission for an overdose where doctors advised against restarting ADHD drugs, this critical information was never relayed to the private provider, which continued prescribing. The coroner noted the absence of formal rules mandating information-sharing between private neurodevelopmental services and NHS teams, warning of similar future deaths without systemic change.
Clinicians working within both NHS and private sectors echo these concerns about assessment quality. One anonymous NHS clinician estimated that "around 70-80%" of private assessments do not meet required standards. Andrew Jay, founder of Divergence, a neurodiversity support platform, found that only 6% of 'right to choose' provider assessments met UK Adult ADHD Network quality standards in a recent audit. Patients often believe they are receiving an NHS-equivalent assessment but are left with inadequate documentation, sometimes having to rejoin NHS waiting lists after paying for private services.
Private clinicians themselves often face overwhelming workloads and chaotic systems. "Craig," a former clinician for a private ADHD clinic, described initial thorough training but a subsequent disconnect where administrative staff, not clinicians, wrote reports under the clinicians' names. He routinely worked double his contracted hours, dealing with a massive caseload and prescription requests, leading to physical and emotional exhaustion. Other clinicians like "Alice" and "Brian" reported similar struggles with administrative systems failing, calls going unanswered, emails piling up, and prescription delays. In extreme cases, clinicians resorted to hand-delivering vital medication to patients when delays became unsafe.
The transition of patients from private treatment to NHS shared care is another significant bottleneck. Clinicians reported promises of smooth transitions often leading to weeks or months of delays, with GPs frequently refusing to take on patients from private clinics. This leaves patients in limbo, needing medication but without clear ongoing oversight. Frontline private staff, while not intending harm, are operating within a sector overwhelmed by demand and expanding faster than its administrative and clinical structures can safely support. Many patients seeking private care are desperate, using savings or borrowing money after years on NHS waiting lists, only to potentially encounter further issues.
In response to these growing concerns, the health secretary, Wes Streeting, has announced an independent review into the diagnosis of mental health conditions, including ADHD. A Department of Health and Social Care spokesperson affirmed that "All providers, including those in the independent sector, must meet the same standards for patient safety and quality as the NHS." The NHS is also actively considering recommendations from an independent ADHD taskforce to improve care and service models, and NHS England has initiated a consultation on appropriate reimbursement for services, acknowledging the urgent need for improvements in this critical area of healthcare.
You may also like...
Splitting Bills at Birthday Parties Should Be Outlawed

Birthday dinners are meant to celebrate love and friendship, so why do they end with calculators and awkward money trans...
Smarter AI, Weaker Grid: The Energy Crisis Behind the Data Center Boom

The race to build smarter AI is colliding with a harsh reality: data centers are consuming electricity faster than power...
"Intelligence Tools Have Changed What It Means to Run a Company" — Dorsey Is Right, and That Should Terrify Us
After Jack Dorsey laid off 4,000 employees at Block Inc., his blunt admission about AI replacing roles exposes a deeper ...
Jazz Star Markkanen Sidelined with Hip Injury, Out for Weeks!

Utah Jazz forward Lauri Markkanen is set for a two-week reevaluation after an MRI confirmed hip impingement, inflammatio...
Thunder's SGA Cleared for Return, Playoff Hopes Surge!

Reigning NBA MVP Shai Gilgeous-Alexander is cleared to return for the Oklahoma City Thunder after missing nine games due...
Horror Franchise in Peril: 'Scream 7' Reviews Slammed Despite Neve Campbell's Return to Basics
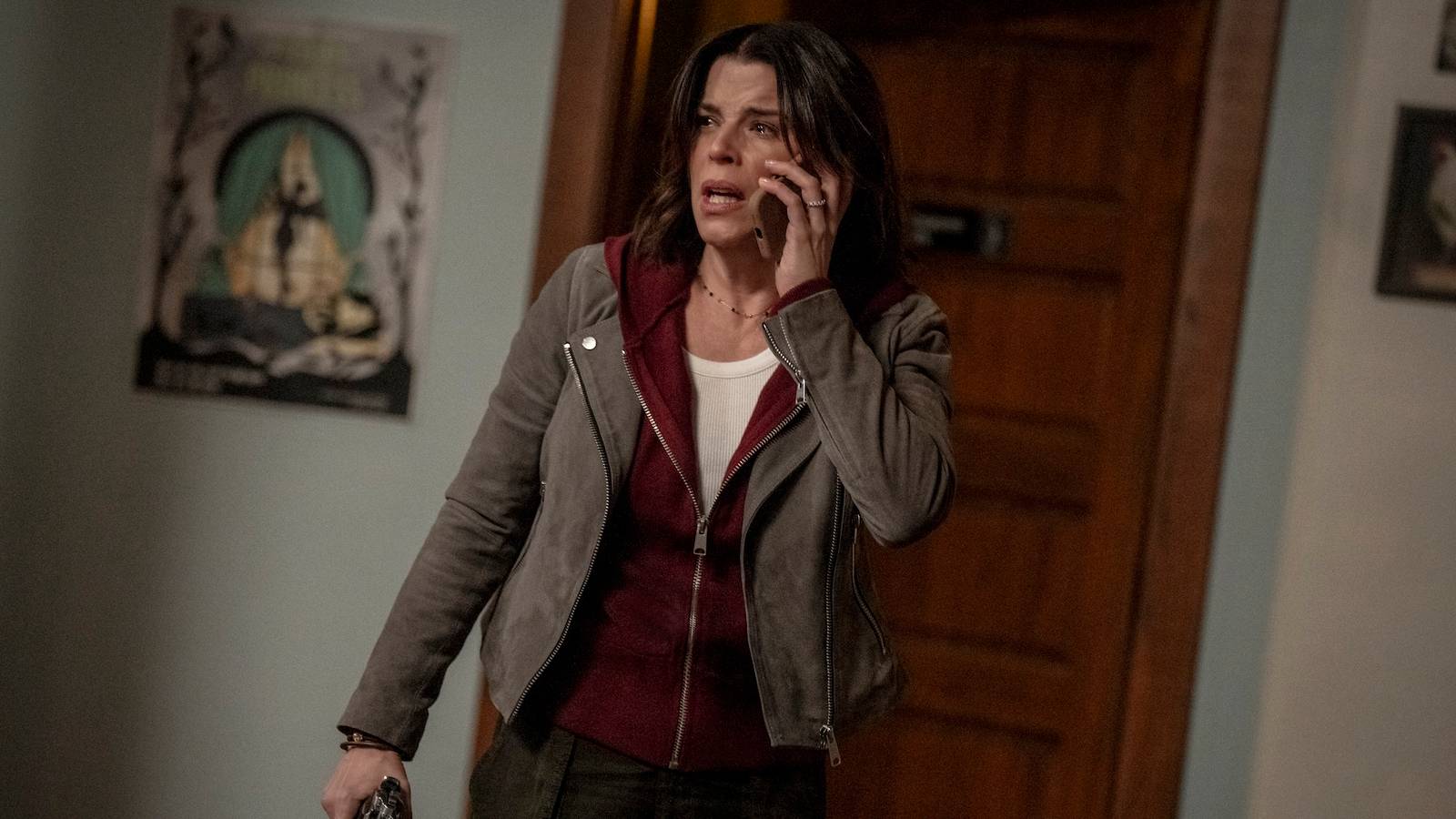
After a tumultuous production and cast exits, "Scream 7" arrives with Kevin Williamson directing and Neve Campbell retur...
Media Giant Merger: Paramount Skydance Poised to Acquire Warner Bros. Discovery, Netflix Stock Surges After Exiting Bidding War

Netflix has abruptly exited its $83 billion deal to acquire Warner Bros. Discovery, allowing Paramount Skydance to proce...
BLACKPINK Unleashes 'Deadline' Mini-Album, Lights Up South Korea’s Most-Visited Museum

Global K-pop sensation BLACKPINK has returned with their new five-track mini-album, "DEADLINE," released on Friday, Feb....


