BMC Public Health volume 25, Article number: 1829 (2025) Cite this article
Aortic aneurysm is one of the causes of cardiovascular disease-related death, posing a significant challenge to global healthcare. Understanding the burden of aortic aneurysm is crucial for formulating effective public health intervention policies and allocating resources. The study aims to assess the global, regional, and national burden, trend, and inequalities of aortic aneurysm.
Aortic aneurysm-associated mortality, disability-adjusted life-years (DALYs), age-standardized mortality rate (ASMR), age-standardized disability-adjusted life-years (ASDR), and their average annual percentage change (AAPC) were estimated based on a population-based study, the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2021. The global, regional, and national burden of aortic aneurysm was analyzed across 204 countries and territories from 1990 to 2021, stratified by sex, sociodemographic index (SDI), and further predicted to 2045.
The ASMR decreased from 2.54 per 100,000 population in 1990 to 1.86 per 100,000 population in 2021, with an AAPC of -0.99%. The ASDR declined from 48.79 per 100,000 population in 1990 to 36.54 per 100,000 population in 2021, with an AAPC of -0.90%. The most significant decline in ASDR was observed among males (-1.14% vs. -0.68% per year). ASMR increased considerably, especially in countries with a low-middle SDI (1.29% per year), while it dropped particularly in countries with a high SDI (-1.65% per year). Notably, though the number of mortality and DALYs was predicted to continue rising, the ASMR and ASDR for aortic aneurysm were projected to decrease annually from, with predicted values of 1.92 per 100,000 population and 40.38 per 100,000 population in 2045, respectively.
The global relative burden of individuals with aortic aneurysm decreased since 1990, along with a prominent decrease in related ASMR and ASDR. Aortic aneurysm-related mortality and DALYs were higher in males and those living in regions with a high SDI.
Aortic aneurysm is a balloon-like dilation of the aorta, occurring in either thoracic or abdominal segments of the aorta. The incidence of aortic aneurysm is approximately 54 cases per 100,000 person-years, as reported by a population-based study involving 420,292 participants in the United Kingdom [1]. It causes a weakness of the aortic wall and significantly increases the risk of a tear, leading to aortic dissection [2]. The probability of adverse aortic events, comprising of aortic dissection, aortic rupture, and sudden death, increases significantly with the maximal aortic diameter of the aneurysm, reaching 62.5% when the diameter exceeds 70 mm, as revealed by a prospective cohort study of 3,247 patients in the United States with aortic aneurysm [3]. However, these studies have predominantly focused on developed countries, with limited attention given to the diverse burden in developing countries.
The Global Burden of Disease (GBD) study offers comprehensive systematic epidemic data for evaluating injuries and diseases across various regions, territories, and populations [4,5,6,7,8]. A systematic analysis of the 2017 Global Burden of Diseases, Injuries, and Risk Factors Study (GBD 2017) described the global, regional, and national burden of aortic aneurysm between 1990 and 2017 [9, 10]. Although recognition of aortic aneurysm as a life-threatening health issue has increased, current updated data on the global burden of aortic aneurysm remain limited. In addition, the projections of future burden trends for aortic aneurysm have yet to be investigated. The GBD 2021 update provides new estimates of the global burden of various diseases [11]. Understanding the current and future global burden of aortic aneurysm using the latest data is critical for public health planning and targeted management.
Thus, this study aims to assess aortic aneurysm-related mortality, disability-adjusted life-years (DALYs), age-standardized mortality rate (ASMR), age-standardized DALYs (ASDR), and their average annual percentage change (AAPC), at global, regional, and national levels, from 1990 to 2021, stratified by sex and sociodemographic index (SDI), and to further project its trend to 2045.
The GBD study, initiated and performed by the Institute for Health Metrics and Evaluation (IHME) at the University of Washington, provides a comprehensive and systematic picture of global health challenges. The GBD 2021 evaluates the global impact of 288 causes of death, 371 diseases and injuries, and 88 risk factors, including aortic aneurysm, across 204 countries and territories over periods from 1990 to 2021 [12]. The GBD 2021 relies on a wealth of health and disease data, drawn from public health databases, hospital records, census data, and other health surveys, which are authorized or provided by the appropriate public health authority. The data from GBD 2021 is aggregated, anonymized, and does not involve personally identifiable information.
We conducted a secondary analysis of the GBD 2021 data without direct access to all individuals. The GBD dataset was accessed through the GBD Results Tool (https://vizhub.healthdata.org/gbd-results/). Extraction parameters were specified to include “mortality” and “disability-adjusted life-years (DALYs)” with corresponding 95% uncertainty intervals (UIs), targeting “aortic aneurysm” across global regions, all age groups, and both sexes from 1990 to 2021. Patients were not involved in formulating the research question, determining the outcome measures, or participating in the design and implementation of the study.
GBD 2021 is based on the 9th and 10th editions of the International Classification of Diseases (ICD). In the GBD 2021, aortic aneurysm is defined as a doctor-diagnosed disease identified through an aortic aneurysm registry or hospital records with ICD-9 codes 441-441.9 and ICD-10 codes I71.1-I71.9. The temporal and regional trends in ASMR and ASDR for aortic aneurysm on global, regional, and national scales were assessed. SDI, a composite indicator combining education (mean years of schooling among individuals older than 15 years), income (per capita lag-distributed income), and fertility rates (total fertility rate among females under 25 years), was calculated to assess social and economic development. Each component was normalized to a 0–1 scale. SDI, defined by the geometric mean of these three normalized values, was multiplied by 100 for reporting purposes. It ranges from 0 to 1, with higher values indicating better socioeconomic and health status [13]. Countries in the study were classified into five categories based on SDI quintiles: low SDI, low-middle SDI, middle SDI, high-middle SDI, and high SDI.
The burden of aortic aneurysm was evaluated based on mortality (per 10,000 population), DALYs (per 100,000 population), ASMR (per 100,000 population), ASDR (per 100,000 population), and AAPC of ASMR and ASDR across sex, regions, and countries on global, regional, and national scales.
DALYs are a metric assessing the overall burden of diseases, injuries, or health problems, combining the loss of quality of life from death and illness to describe the health status of a group at a given time. DALYs are calculated using the formula: years of life lost (YLL) + years lived with disability (YLD) [14, 15]. Specifically, YLL refers to the years lost due to premature death, calculated as: number of estimated deaths × (standard life expectancy - actual age at death). YLD indicates the years lost due to disease, injury, or disability, computed as the prevalence of sequela × disability weights for the health state.
Age standardization was performed using the standard world population of GBD 2021. ASMR is used to compare mortality differences among populations in different countries, regions, or periods. By adjusting for differences in age distribution across populations, ASMR ensures comparability of mortality among groups with different age structures [16]. Direct comparison of mortality rates may lead to unfair conclusions, as the age structure of different populations can vary significantly. ASMR eliminates the impact of age structure differences on mortality, facilitating comparison of mortality rates across populations, regions, or time. ASDR, combining death and disability burden, eliminates the effect of age structure differences when comparing DALYs across populations or regions, allowing fair comparison of health burden between different populations [17]. To describe and analyze the trend of ASMR and ASDR of aortic aneurysm over time, the joinpoint regression model splits the data into different trend segments by identifying and quantifying joinpoints [18].
AAPC is a measure of the average annual rate of change in an indicator over a specific period, often used to compare health trends across time periods, especially when data shows year-to-year fluctuations or changes. AAPC provides a standardized measure of change that overcomes the limitations of using annual changes alone, making cross-year, cross-group, and cross-regional data analysis more objective and comparable. For the study, AAPC was derived from the weighted average of the slope coefficients in each segment of the joinpoint regression model over a specific period. AAPC clearly shows whether the change is increasing, decreasing or stable. If AAPC and corresponding 95% confidence intervals (CIs) are > 0, <0, or = 0, it indicates an average annual increase, decline, or stable during the study period, respectively [19].
The age-period-cohort model was applied to analyze the changing trends of ASMR and ASDR, considering three temporal factors into account: age, period, and cohort [20]. Changes associated with biological (such as physiological structure and function) and social (such as social experience and role) processes of aging are considered age effect, denoted by varying rates of aortic aneurysm (per 100,000 population) across 17 age groups: 15–19 years, 20–24 years, 25–29 years, 30–34 years, 35–39 years, 40–44 years, 45–49 years, 50–54 years, 55–59 years, 60–64 years, 65–69 years, 70–74 years, 75–79 years, 80–84 years, 85–89 years, 90–94 years, and ≥ 95 years. External factors affecting different age groups at specific times, such as war, famine and epidemic, as well as technologic advances in diagnosis, screening, early detection, and treatment, lead to period effect, expressed by the rate ratio of aortic aneurysm across 6 period groups: 1992–1996, 1997–2001, 2002–2006, 2007–2011, 2012–2016, and 2017–2021. Variations caused by specific exposures within a birth cohort form cohort effect, represented by the risk ratio of aortic aneurysm across 22 birth cohorts: 1892–1901, 1897–1906, 1902–1911, 1907–1916, 1912–1921, 1917–1926, 1922–1931, 1927–1936, 1932–1941, 1937–1946, 1942–1951, 1947–1956, 1952–1961, 1957–1966, 1962–1971, 1967–1976, 1972–1981, 1977–1986, 1982–1991, 1987–1996, 1992–2001, and 1997–2006. A Bayesian age-period-cohort model was used to predict the future burden of aortic aneurysm, including the number of deaths, DALYs, ASMR, and ASDR.
Cross-country inequality analysis was used to assess differences in the burden of aortic aneurysm, particularly DALYs, across countries or regions. Frontier analysis was applied to evaluate the gap between countries and identify which countries achieve the best health performance with limited resources, serving as a “benchmark” for others by comparing a country’s actual performance with that of frontier countries.
The joinpoint regression program (version 5.0.2), R (version 4.2.3), and STATA (version 18) were used for statistical analyses.
The global mortality and DALYs of aortic aneurysm from 1990 to 2021 are shown in Table 1. Globally, the mortality rate of aortic aneurysm significantly increased by 74.22%, from 8.84 (95% UI 8.31 to 9.35) per 10,000 population in 1990 to 15.39 (95% UI 13.84 to 16.57) per 10,000 population in 2021. The ASMR of aortic aneurysm decreased from 2.54 (95% UI 2.35 to 2.69) per 100,000 population in 1990 to 1.86 (95% UI 1.67 to 2.00) per 100,000 population in 2021, with an average annual trend of -0.99% (95% CI -1.06% to -0.91%).
The DALYs of aortic aneurysm have shown an upward trend during the same period, rising from 18.84 (95% UI 17.84 to 20.07) per 100,000 population in 1990 to 31.08 (95% UI 28.57 to 33.54) per 100,000 population in 2021. The ASDR of aortic aneurysm declined from 48.79 (95% UI 46.01 to 51.80) per 100,000 population in 1990 to 36.54 (95% UI 33.52 to 39.46) per 100,000 population in 2021, with an average annual trend of -0.90% (95% CI -0.98% to -0.83%).
From 1990 to 2021, the global mortality rate of aortic aneurysm increased for both males and females (males: from 5.76 per 10,000 population to 9.39 per 10,000 population; females: from 3.08 per 10,000 population to 6.01 per 10,000 population). During the same period, the ASMR for aortic aneurysm decreased for both males and females worldwide (males: from 3.87 per 100,000 population to 2.57 per 100,000 population; females: from 1.58 per 100,000 population to 1.28 per 100,000 population). The decrease in the average annual trend of aortic aneurysm mortality was more rapid in males than in females (AAPC: -1.31% vs. -0.64%) (Table 1).
From 1990 to 2021, the global DALYs for aortic aneurysm rised for both males and females (males: from 12.89 per 100,000 population to 20.50 per 100,000 population; females: from 5.95 per 100,000 population to 10.58 per 100,000 population). During the same period, the ASDR for aortic aneurysm decreased for both males and females (males: from 74.09 per 100,000 population to 51.78 per 100,000 population; females: from 28.52 per 100,000 population to 23.01 per 100,000 population), although the reduction was less pronounced in females (AAPC: -0.68% vs. -1.14%) (Table 1).
Supplementary Fig. 1 demonstrates the results of joinpoint regression analysis on the ASMR and ASDR for aortic aneurysm by sex. The local trends across different joinpoints were inconsistent, although both ASMR and ASDR generally showed dramatic declines. After experiencing a slight rise in 1990–1994 (AAPC: 0.80%), the global trend of ASMR continuously fell in 1994–1999 (AAPC:-0.67%), 1999–2012 (AAPC: -1.84%), and 2012–2021 (AAPC: -0.71%). Despite a gradual growth in 1990–1995 (AAPC: 0.41%), the ASMR of males plummeted in 1995–2003 (AAPC: -1.65%), 2003–2013 (AAPC: -2.29%) and 2013–2021 (AAPC: -0.82%). As for females, the global trend of ASMR underwent a slight increase in 1990–1994 (AAPC: 0.88%), a considerable drop in 1999–2011 (AAPC: -1.52%), and a gradual decline in 2011–2021 (AAPC: -0.46%), while it leveled off in 1994–1999 (AAPC: -0.11%).
The global trend of ASDR exhibited three joinpoints of a significant rise in 1990–1994 (AAPC: 1.14%), and three spiral declines in 1994–1999 (AAPC: -1.00%), 1999–2013 (AAPC: -1.71%), and 2013–2021 (AAPC: -0.44%). The ASDR of males also showed three joinpoints, with a gradual increase in 1990–1995 (AAPC: 0.60%), followed by dramatic declines in 1995–2003 (AAPC: -1.69%) and 2003–2013 (AAPC: -2.00%), and a slight dip in 2013–2021 (AAPC: -0.60%). As for females, the ASDR initially increased in 1990–1994 (AAPC: 1.09%), followed by a period of stability in 1994–1999 (AAPC: -0.46%). After that, it plunged in 1999–2011 (AAPC: -1.56%), followed by a slight decline in 2011–2021 (AAPC: -0.44%).
Figure 1 illustrates the age-period-cohort analysis of ASMR and ASDR for aortic aneurysm stratified by sex. The average annual trend of ASMR and ASDR fluctuated considerably across different age groups. The most significant decrease in both ASMR and ASDR was observed in both males and females aged 75 to 79 years (Fig. 1A and B). After controlling for the effects of period and birth cohort, the impact of age on the risk of aortic aneurysm (ASMR and ASDR) was evident, with a dramatic surge for females in all age groups and a sharp rise for males under 95 years followed by a gradual fall after age 95 (Fig. 1C and D). After controlling for the effects of age and birth cohort, the rate ratio, a metric quantifying the effect of period on ASMR and ASDR, fell dramatically in both males and females from 1992 to 2021 (Fig. 1E and F). After controlling for the effects of age and period, the risk ratio of ASMR and ASDR in earlier birth cohorts was higher than in later birth cohorts. Additionally, the ASMR and ASDR in males exhibited a higher risk ratio than females across all birth cohorts (Fig. 1G and H).
Age-period-cohort analysis of ASMR and ASDR for aortic aneurysm. A and B. Drift and local drifts for ASMR and ASDR, respectively; C and D. Age effects on ASMR and ASDR, respectively; E and F. Period effects on ASMR and ASDR, respectively; G and H. Birth cohort effects on ASMR and ASDR, respectively. Abbreviations: ASDR: age-standardized disability-adjusted life-years rate; ASMR: age-standardized mortality rate
Aortic aneurysm-related mortality increased across all SDI subgroups during 1990–2021, especially in low-middle SDI countries, which rose by 264.76% from 0.46 (95% UI 0.37 to 0.63) per 10,000 population in 1990 to 1.68 (95% UI 1.40 to 2.25) per 10,000 population in 2021. In 2021, the highest mortality from aortic aneurysm was in countries with a high SDI (6.72 per 10,000 population), more than 10 times the mortality in countries with a low SDI (0.64 per 10,000 population). The ASMR of aortic aneurysm underwent an upward trend in countries with low, low-middle, and middle SDI, while it showed a downward trend in countries with high-middle and high SDI. The largest increase was observed in countries with a low-middle SDI (AAPC: 1.29%), which was 4.61 times faster than in countries with a low SDI (AAPC: 0.28%). The largest decrease was investigated in countries with a high SDI (AAPC: -1.65%), which was 4.71 times faster than in countries with a high-middle SDI (AAPC: -0.35%) (Supplementary Table 1). Results of joinpoint regression analysis revealed that the ASMR of aortic aneurysm in countries with a low-middle SDI climbed considerably during the same period, with four joinpoints: 1990–1996 (AAPC: 1.97%), 1996–2006 (AAPC: 0.86%), 2006–2012 (AAPC: 1.31%), 2012–2019 (AAPC: 1.90%), and 2019–2021 (AAPC: -0.76%). In contrast, the ASMR in countries with a high SDI experienced a continuous drop, especially in 2002–2013 (AAPC: -2.87%) (Supplementary Fig. 2).
The DALYs from aortic aneurysm increased across all SDI subgroups during 1990–2021, especially in low-middle SDI countries, which rose by 241.13%, from 1.17 (95% UI 0.93 to 1.60) per 100,000 population in 1990 to 3.98 (95% UI 3.34 to 5.30) per 100,000 population in 2021. In 2021, the highest DALYs from aortic aneurysm were observed in countries with a high SDI (11.20 per 100,000 population), which was 6.87 times higher than in countries with a low SDI (1.63 per 100,000 population). The ASDR of aortic aneurysm decreased in countries with high-middle and high SDI, while it increased in countries with low, low-middle, and middle SDI. The largest decrease occurred in countries with a high SDI, which was more than 6 times faster than in countries with a high-middle SDI (AAPC: -1.69% vs. -0.27%). The largest increase was seen in countries with a low-middle SDI, which was more than 5 times faster than in countries with a low SDI (AAPC: 1.24% vs. 0.23%). (Supplementary Table 1). There was a significant rise in the ASDR of aortic aneurysm in countries with a low-middle SDI during the same period, with three joinpoints: 1990–1996 (AAPC: 1.85%), 1996–2012 (AAPC: 0.95%), 2012–2019 (AAPC: 1.82%), and 2019–2021 (AAPC: -0.29%). Conversely, a sharp drop was observed for the ASDR of countries with a high SDI, especially during the period 2002–2013 (AAPC: -2.93%) (Supplementary Fig. 2).
Figure 2 displays the cross-country inequality analysis of aortic aneurysm. It is evident that the distribution of the burden was imbalanced among countries with different SDI levels. Countries with high sociodemographic development levels bore a disproportionate concentration of DALYs. The frontier analysis showed that the top 15 countries with the most potential for improvement were Armenia, Montenegro, Nauru, Russian Federation, Japan, Belarus, Monaco, Brunei Darussalam, Uruguay, Brazil, Grenada, Saint Lucia, Serbia, Zimbabwe, and Greece, with the largest effective differences ranging from 190.96 to 81.03. Frontier countries with low SDI (< 0.5) and low effective difference included Somalia, Niger, Afghanistan, Yemen, and Timor-Leste. Countries with a high SDI (> 0.85) but substantial room for improvement included Japan, Monaco, Norway, Denmark, and Lithuania (Fig. 2A, Supplementary Table 2). There was a significant decline in the concentration index, a measure of relative gradient inequality, which ranged from 0.34 (95% CI 0.27 to 0.40) in 1990 to 0.08 (95% CI 0.02 to 0.13) in 2021 (Fig. 2B). The trend of DALYs relative to SDI from 1990 to 2021 was shown by the frontier analysis of aortic aneurysm (Fig. 2C), indicating significant space for improvement in the burden of aortic aneurysm relative to national sociodemographic development levels. However, the slope index of inequality, a measure of absolute gradient inequalities, edged up from 70 DALYs per 100,000 population in 1990 to 83 DALYs per 100,000 population in 2021 between countries with the highest and lowest SDI (Fig. 2D).
Cross-country inequality analysis of aortic aneurysm. (A) Frontier analysis based on ASDR for aortic aneurysm and SDI in 2021, with the frontier in solid black and countries as dots. The top 15 countries with the largest effective difference were labeled in black. Frontier countries with low SDI (< 0.5) and low effective difference were labeled in blue, while those with high SDI (> 0.85) and relatively high effective difference were labeled in red. Blue dots signified a rise in ASDR, while red dots indicated a decline in ASDR during 1990–2021; (B) Concentration index for DALYs of aortic aneurysm worldwide in 1990 and 2021, with points representing countries sized by population; (C) Frontier analysis based on ASDR for aortic aneurysm and SDI from 1990 to 2021, where the color scale represents the years (dark blue for 1990, light blue for 2021), and the frontier is delineated in solid black; (D) Inequality slop index for DALYs of aortic aneurysm worldwide in 1990 to 2021, with points representing countries sized by population. Data in 1990 was visualized in blue, while data in 2021 was visualized in red. Abbreviations: ASDR: age-standardized disability-adjusted life-years rate; DALYs: disability-adjusted life-years; SDI: sociodemographic index
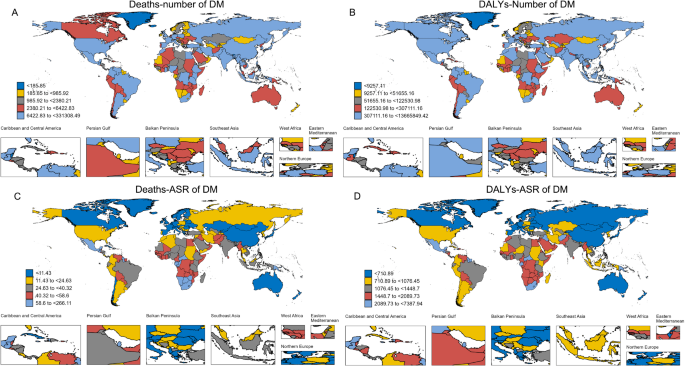
At the national level, Armenia had the highest ASMR and ASDR of aortic aneurysm in 2021 (ASMR: 9.16 per 100,000 population; ASDR: 192.82 per 100,000 population), followed by Montenegro (ASMR: 8.65 per 100,000 population; ASDR: 178.94 per 100,000 population) and Nauru (ASMR: 6.01 per 100,000 population; ASDR: 114.52 per 100,000 population). Saudi Arabia had the lowest ASMR and ASDR of aortic aneurysm in 2021 (ASMR: 0.21 per 100,000 population; ASDR: 5.08 per 100,000 population) (Supplementary Table 3, Fig. 3).
From 1990 to 2021, Uzbekistan experienced the highest increase in ASMR and ASDR, with an average annual trend of 5.04% and 4.87% respectively, followed by Georgia (AAPC of ASMR: 4.93%; AAPC of ASDR: 4.74%) and Kyrgyzstan (AAPC of ASMR: 4.32%; AAPC of ASDR: 3.92%). Over the same period, Guam showed the most substantial decline in ASMR (AAPC: -4.46%), followed by Australia (AAPC: -3.77%) and Canada (AAPC: -3.42%). The country with the greatest decrease in ASDR for people with aortic aneurysm was Australia (AAPC: -3.90%), followed by Bermuda (AAPC: -3.78%) and Guam (AAPC: -3.42%) (Supplementary Table 4, Supplementary Fig. 3).
ASMR and ASDR for aortic aneurysm in 2021. (A) ASMR; (B) ASDR. Abbreviations: ASDR: age-standardized disability-adjusted life-years rate; ASMR: age-standardized mortality rate
The globally predicted case numbers for mortality, DALYs, ASMR, and ASDR for aortic aneurysm to 2045 in both males and females are illustrated in Fig. 4, Supplementary Tables 5, and Supplementary Table 6. Based on the Bayesian age-period-cohort model, the total number of deaths from aortic aneurysm is expected to increase by 96.43%, from 16.24 per 10,000 population in 2022 to 31.90 per 10,000 population in 2045, with the steepest rise projected for males at 98%. The number of DALYs from aortic aneurysm is anticipated to undergo a steady upward trend by 82.87%, from 3.27 per 1,000,000 population in 2022 to 5.98 per 1,000,000 population in 2045, with the steepest rise projected for females at 90.83% (Supplementary Table 5). Both females and males are expected to dip gradually in ASMR for aortic aneurysm by 10.16% and 4.26% within the next decades, respectively. Concurrently, a slight decrease of 4.71% in ASDR for aortic aneurysm is expected for females, and a minimal decrease of 0.23% is anticipated for males (Supplementary Table 6).
Bayesian age-period-cohort predicted number of mortality, DALYs, ASMR and ASDR for aortic aneurysm by sex from 1990 to 2045 at a global level. (A) The number of mortality and ASMR; (B) The number of DALYs and ASDR. Abbreviations: ASDR: age-standardized disability-adjusted life-years rate; ASMR: age-standardized mortality rate; ASR: age-standardized rate; DALYs: disability-adjusted life-years
This study provided the mortality, DALYs, ASMR and ASDR of aortic aneurysm at global, regional, and national levels from 1990 to 2021 using the most updated GBD 2021 data, and further forecasted its burden trend to 2045. Although the overall burden of aortic aneurysm has increased in absolute terms (mortality and DALYs), its relative burden (ASMR and ASDR) has decreased, with the sharpest drop occurring during the first decade of the 21st century. This may be attributed to better prevention measures, improved treatment levels, and other social health interventions. The cross-country inequality analysis showed that SDI-related relative inequality decreased, while absolute inequality exacerbated over time. It is worth noting that despite the anticipated decline in the ASMR and ASDR from 2022 to 2045, the number of deaths and DALYs is predicted to keep elevating, indicating a significant challenge in the future control and management of aortic aneurysm.
The global burden of aortic aneurysm varies by sex. Compared to females, the mortality, DALYs, ASMR, and ASDR of aortic aneurysm were higher in males, owing to high-risk behaviors such as cigarette smoking and cocaine use in males [21,22,23]. Additionally, approximately 20% of patients with aortic aneurysm have evidence of a family history or genetic conditions, such as Ehlers–Danlos syndrome, Loeys–Dietz syndrome, and Marfan syndrome, which predominantly affect males [24, 25]. In patients with Marfan syndrome, aortic root dilatation, aortic regurgitation and aortic surgery are more likely to occur in males than in females [26]. Males with single gene disorders are more likely to develop aortic disease. In patients with fibrillin-1 (FBN1) mutations, males are at higher risk of developing ascending aortic dilatation and aortic events (all P < 0.01) [27]. The above evidence suggests more severe manifestations of aortic disease in males.
It is also obvious that the decline in ASMR and ASDR was pronounced in both males and females, especially during the first decade of the 21st century, because of advances in medical technology, such as early screening and treatment of aortic aneurysms, and public health interventions, such as smoking control, and blood pressure management [28, 29]. While females experienced slower improvement in the burden of aortic aneurysm than males, this may be attributed to the protective effect of estrogen and cultural differences. Firstly, estrogen plays a protective role in cardiovascular diseases, such as atherosclerosis, coronary heart disease, and hypertension [30,31,32], which are well-documented risk factors for aortic aneurysm. Secondly, in some regions and socio-cultural contexts, females have less access to healthcare and experience poorer healthcare outcomes due to a patriarchal worldview [33,34,35,36].
The burden of aortic aneurysm significantly differs among countries with different SDI. The ASMR and ASDR of aortic aneurysm decreased in countries with high-middle and high SDI, while increased in countries with low, low-middle, and middle SDI. Specially, Armenia, Montenegro, and Nauru led the world in aortic aneurysmal-related ASMR and ASDR in 2021, while Saudi Arabia had the lowest ASMR and ASDR. Uzbekistan, Georgia, and Kyrgyzstan had the largest annual increases in ASMR and ASDR from 1990 to 2021, while Guam, Australia, and Canada showed significant reductions. Inadequate healthcare infrastructure, public health services, health education, and disease prevention and treatment hinder healthcare improvement in developing countries. In contrast, developed countries often have better healthcare systems and disease prevention measures and place greater emphasis on public health policies and interventions, such as early screening and surgical treatment, leading to significant declines in ASMR and ASDR. It has been reported that the number of adult and pediatric cardiac surgeons in high-income countries are 179 and 136 times greater than in low-income countries (7.5 per million population vs. 0.04 per million population; 9.51 per million population vs. 0.07 per million population), respectively [37, 38]. In Africa, the number of cardiac centers is 1 per 33 million population, dramatically lower in North America (1 center per 120,000 population), Europe and Oceania (1 center per million population), and Asia (1 per 16 million population) [38, 39].
The ASMR and ASDR of aortic aneurysm are expected to decline slightly due to advances in medical technology and early intervention. Nevertheless, the absolute global burden of aortic aneurysms is expected to continue to increase due to the growing aging population, especially in terms of mortality and DALYs. This indicates significant challenges in the management and early screening of aortic aneurysm in the elderly population. Older populations tend to have higher rates of aortic aneurysm-related risk factors, such as hypertension and atherosclerosis [40]. Universal screening in aging populations is not cost-effective. In addition, a greater increase of DALYs in females compared to males was observed. Although males face a higher risk of death due to unhealthy lifestyles, females tend to live longer after developing the disease and may experience more complications and dysfunction in old age. Accordingly, females will bear a greater long-term health burden from aortic aneurysm. Therefore, policymakers should prioritize early risk-stratified screening, risk factor control, and healthcare system preparedness to provide stronger support for the high-risk elderly population.
The decline in ASMR and ASDR is encouraging, especially for individuals with aortic aneurysm and their families in countries with a high SDI. However, the increasing number of mortality and DALYs pose a huge challenge for policymakers, particularly in countries with a low-middle SDI. In clinical practice, males are encouraged to improve their lifestyles, self-management skills, and health education. Effective care and treatment training for females is also necessary for doctors and caregivers.
Several limitations exist in the study. Firstly, the epidemiological data were extracted from the GBD database, which may be biased due to variations in health systems and reporting mechanisms, especially in countries with low SDI [41]. Secondly, differences in health systems, policies, practices, and education may influence the burden of aortic aneurysm. Whether the interpretation of the results in this study applies to the real world remains to be validated by further high-quality evidence. Thirdly, because of the complexity of data reporting, collection, processing, and integration, as well as the application of model predictions and multi-source data, there is a time lag for the GBD data.
Although the number of mortality and DALYs for aortic aneurysm increased significantly from 1990 to 2021, the ASMR and ASDR declined remarkably, with the highest levels remaining in males and in people living in countries with a high SDI.
All data used in the study are available in the Global Health Data Exchange (http://ghdx.healthdata.org/gbd-results-tool).
The Overseas Exchange and Cooperation Program for Graduate Students at Shantou University Medical College, China (No. 002-18124704), Funding for Guangdong Medical Leading Talent, the First Affiliated Hospital of Shantou University Medical College, China (No. 2019–2022), and Special Fund from the Central Government for Guiding Local Scientific and Technological Development in 2024 (No. STKJ2024068) supported this research.
Not applicable.
Not applicable.
The authors declare no competing interests.
Patients and/or the public were not involved in the design, conduct, reporting, or dissemination plans of this research.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Tian, C., Zhang, X., Tang, H. et al. Disease burden of aortic aneurysm from 1990 to 2021 with a forecast to 2045: insights from the global burden of disease 2021. BMC Public Health 25, 1829 (2025). https://doi.org/10.1186/s12889-025-23067-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-025-23067-7