BMC Public Health volume 25, Article number: 1248 (2025) Cite this article
Viral hepatitis, recognized as a significant global public health threat by the World Health Organization (WHO), has spurred efforts to establish elimination goals by 2030. In Republic of Korea (Korea), the prevalence of Hepatitis C virus (HCV) infection exhibits significant regional disparities, necessitating tailored infection control measures at the regional level. This study aimed to analyze the HCV prevalence trend by area (region/town) in Korea, from 2005 to 2022, and identify the areas requiring priority management.
A comprehensive analysis of HCV prevalence trends across different geographical regions and towns from 2005 to 2022 was conducted. Using data from the National Health Insurance Service, individuals diagnosed with acute or chronic HCV during this period were included in the analysis. HCV prevalence was adjusted by area, year, sex, and age. Additionally, trends in annual percent changes (APC) and average APC (AAPC) in HCV prevalence were examined using Joinpoint regression analysis.
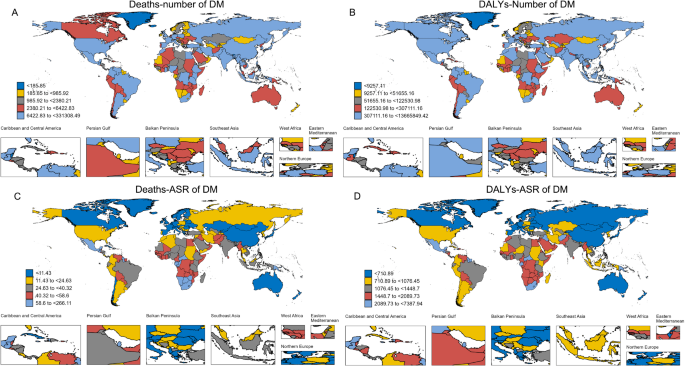
Age, sex, and region adjusted HCV prevalence per 100,000 people declined from 151 in 2005 to 98 in 2022. During the 18 years, the highest HCV prevalence was recorded in the southern regions of Korea (Busan, Jeonnam, and Gyeongnam) and in the towns of Namhae-gun of Gyeongnam, Boeun-gun of Chungbuk, and Sunchang-gun of Jeonbuk. The age-, sex-, and region-adjusted annual HCV prevalence decreased significantly at an APC of -2.5% (95% confidence interval [CI]: -3.5, -1.4) and AAPC of -2.7% (95%CI: -4.3, -1.0). By town, the prevalence decreased the most in Boeun-gun of Chungbuk (AAPC: -23.7%; 95%CI: -30.2, -16.5) and increased the most in Gunwi-gun of Gyeongbuk (AAPC: 3.0%; 95%CI: 1.1, 4.9).
Over 18 years, a notable decline in HCV prevalence was observed in Korea, although this trend exhibited regional disparities. To effectively achieve the WHO hepatitis elimination goals by 2030, targeted interventions should prioritize areas with persistent or emerging prevalence.
Hepatitis C virus (HCV) infection, alongside hepatitis B virus (HBV) infection, poses a significant risk factor for liver cirrhosis and liver cancer. As of 2019, the World Health Organization (WHO) reported a global prevalence of HCV at 0.8% (range, 0.6–1%), affecting approximately 58 million individuals worldwide with chronic HCV infection [1]. In 2020, the highest prevalence rates were observed in Eastern Europe (2.9%) and Central Asia (2.6%), with China (9.48 million), Pakistan (7.39 million), and India (6.13 million) ranking as the top three countries with the highest disease burden [2].
The prevalence of HCV exhibits significant variation among countries. In Republic of Korea (hereinafter Korea), the HCV prevalence is relatively low, ranging from 0.6 to 0.78% [3,4,5,6]. Mongolia has a notably high prevalence of 11.2% [7], while Japan records the lowest prevalence at 0.13% [8]. In terms of HCV-related mortality in 2019, Mongolia recorded 54.80 deaths per 100,000 population, Japan 7.98, China 4.04, and Korea 3.87. Notably, Mongolia’s HCV-related mortality has increased by 53% since 1990 [9]. These trends underscore the critical need for effective policy interventions in HCV management.
Globally, over a million deaths attributed to liver cirrhosis and hepatocellular carcinoma due to chronic viral hepatitis were recorded in 2019 [10], with projections indicating an increase until 2040 [11, 12]. In response, the WHO has identified viral hepatitis as a pressing global public health concern, setting forth elimination goals by 2030, with target annual incidence and mortality rates for HCV infection [13]. Similarly, Korea is formulating a specific roadmap towards achieving these goals. However, unlike that of HBV infection, the prevalence of HCV infection exhibits significant regional disparities, necessitating tailored infection control measures at the regional level.
In Taiwan, the prevalence of HCV infection, as indicated by anti-HCV positivity rates, varied considerably across regions, ranging from 0.3 to 7.6%. In response, the Taiwanese government categorized regions into seven potential risk grades and implemented priority screening and treatment programs in areas with higher prevalence rates, aligning with its HCV elimination strategy [14]. Similarly, in Korea, regions such as Busan, Jeonnam, and Gyeongnam exhibited HCV prevalence rates approximately five times higher than the global average [14].
Consequently, prioritizing the management of HCV in high-risk regions is paramount to achieving HCV elimination goals by 2030, underscoring the need for comprehensive regional epidemiological studies. Prior research in Korea, spanning 2005 to 2012 [15], lacked the inclusion of data reflecting the impact of direct-acting antivirals covered by health insurance since August 1, 2015. Additionally, previous studies predominantly focused on 17 regions, potentially overlooking high-prevalence towns. In this study, we aimed to analyze age- and sex-adjusted HCV prevalence trends over an 18-year period (2005–2022) across 17 regions and 257 towns, identifying areas warranting priority management.
We utilized data from National Health Insurance Service (NHIS) spanning 2002 to December 31, 2022. The NHIS dataset in Korea represents extensive big data encompassing the utilization of healthcare infrastructure by NHIS subscribers, a system that was expanded to encompass the entire Korean population in 1989. This data contains comprehensive information, including patients’ demographic details (such as age, sex, and area of residence), income levels (including type of health insurance), specifics of healthcare services (such as diagnosis code, surgeries, procedures, and prescribed medications), and date of death [16].
While one limitation of the data is the absence of information on non-reimbursable healthcare services, diagnostic tests and treatment drugs for HCV are covered by the National Health Insurance system [17]. Therefore, our data comprehensively captures HCV-related healthcare services. Additionally, this data covers a vast population, with 51.41 million out of 52.93 million individuals (representing 97.1% of the population) benefiting from health insurance as of December 2021 [18].
Patients diagnosed with acute or chronic HCV as indicated by the International Classification of Disease, 10th Revision (ICD-10th ) codes B17.1 and B18.2, either as a primary or secondary diagnosis, between 2005 and 2022 were included in the study. Each patient receiving multiple healthcare services within a single year was considered a single prevalent case.
To ensure accurate identification of incident cases, we excluded patients with any HCV diagnostic records prior to 2005. Incident cases were then defined as patients who received their first diagnosis of acute or chronic HCV infection between 2005 and 2022.
The date of death was used to identify deaths among final prevalent cases, and the all-cause mortality was calculated.
The prevalence of HCV was estimated by year, sex, and age for each area (region, town). The year-end resident registration population of the corresponding year served as the reference population (denominator), while the 2020 year-end resident registration population was utilized as the standard population for age-, sex-, and area-adjusted prevalence and incidence rates [19].
To identify significant changes in the temporal trend of HCV prevalence over 18 years and to objectively analyze the optimal inflection points, we utilized Joinpoint Regression Program version 4.9.1. This analytical method possesses the capability to identify statistically significant changes in trend data over time, making it particularly suitable for analyzing long-term patterns of HCV prevalence. The analysis employed two primary metrics: Annual Percent Change (APC) and Average Annual Percent Change (AAPC). APC represents the exponential slope calculated from the linear trend of log-transformed annual prevalence, allowing for the detection of significant changes in trend patterns at specific points in time [20]. AAPC was derived by applying a weighted average of the APC values from 2005 to 2022 to assess the overall trend throughout the study period.
Age- and sex-adjusted annual prevalence of HCV was visualized on town maps using R Studio version 4.3.0. All statistical analyses were conducted using SAS Enterprise Guide 7.1 (SAS Institute, Cary, NC, USA), with a significance level set at P < 0.05. The study was approved by the Institutional Review Board of the National Cancer Center (NCC2023-0026).
From 2005 to 2022, the annual number of HCV prevalent cases ranged from 52,756 to 79,787, with a mean age of 56.8 years (55.1 in men, 58.5 in women). Age-, sex-, and region-adjusted annual HCV prevalence peaked at 185 per 100,000 in 2007, fluctuating in subsequent years and eventually declining to 98 per 100,000 in 2022. Sex- and region-adjusted prevalence increased with age, with the highest prevalence observed in the 70–79-year-old group, while age- and region-adjusted prevalence did not significantly differ between sexes (Table 1; Fig. 1). The age- and sex-adjusted incidence rate per 100,000 steadily decreased over the 18-year period, from 78.3 in 2005 to 16.3 in 2022. Conversely, the all-cause mortality rate increased from 1.1% in 2005 to 1.6% in 2022 (Additional file 1).
From 2005 to 2022, Busan consistently exhibited the highest HCV prevalence among regions, while Chungbuk consistently had the lowest prevalence, except for the period between 2006 and 2008. Throughout this period, HCV prevalence in Busan, Jeonnam, Gyeongnam, and Jeju consistently surpassed the national average. Daegu initially had a prevalence below the national average, but from 2014 to 2022, its prevalence exceeded the national average, as did that of Incheon from 2017 onwards, remaining similar until 2022. (Table 1; Additional file 2).
In 2022, the age- and sex-adjusted HCV prevalence per 100,000 was highest in Busan at 210, followed by Gyeongnam at 131 and Jeonnam at 127. Conversely, Chungbuk had the lowest prevalence at 40, followed by Gangwon at 57 and Sejong at 58 (Table 1).
The towns with the highest age- and sex-adjusted prevalence of HCV varied over time, including Namhae-gun of Gyeongnam (2005), Boeun-gun of Chungbuk (2006–2008), Sunchang-gun of Jeonbuk (2009–2015, 2018–2019), Jindo-gun of Jeonnam (2016–2017, 2020), and Seo-gu of Busan (2021–2022). Notably, high HCV prevalence was not limited to previously identified high-prevalence towns, but it was extended to neighboring towns, such as Jung-gu of Busan, Shinan-gun and Mokpo-si of Jeonnam, and Sacheon-si of Gyeongnam. Additionally, Sunchang-gun of Jeonbuk, Boeun-gun of Chungbuk, Geumsan-gun, and Yesan-gun of Chungnam were identified as towns with high HCV prevalence rates despite their distance from the traditionally high-prevalence southern regions (Table 2; Fig. 2).
While a significant disparity in HCV prevalence existed between high-prevalence and other towns in 2005, this gap narrowed over time. In recent years, HCV prevalence has gradually increased in towns neighboring high-prevalence areas, such as Seo-gu and Jung-gu of Busan, indicating a spread of HCV infections from high-prevalence towns to adjacent areas (Fig. 2).
Between 2005 and 2022, the age-, sex-, and area-adjusted prevalence of HCV significantly decreased, demonstrating an APC of -2.5% (95% confidence interval [CI]: -3.5, -1.4). Delving deeper into the analysis, joinpoint regression revealed notable fluctuations in HCV prevalence over the years. Specifically, the APC results indicated an initial increase of 8.8% per year between 2005 and 2007 (95% CI: -1.8, 24.3), followed by a significant decrease of 1.7% per year between 2007 and 2018 (95% CI: -2.6, -0.7), and a subsequent substantial decline of 10.4% per year between 2018 and 2022 (95% CI: -14.2, -6.4). The AAPC for the entire period was − 2.7%, reflecting a consistent annual decrease of 2.7% (95% CI: -4.3, -1.0) (Table 3).
Examining regional trends, Jeonnam demonstrated the most substantial decrease in age- and sex-adjusted HCV prevalence over the 18-year period (AAPC: -4.4%; 95% CI: -5.3, -3.4), while Incheon exhibited the smallest reduction (AAPC: -0.7%; 95% CI: -2.2, 0.9) (Table 3). Notably, Daegu, Incheon, Chungbuk, and Jeju displayed the most frequent changes in HCV prevalence, with four joinpoint alterations observed over the study duration (Table 3).
Further analysis at the town level revealed significant variations in prevalence trends. Boeun-gun of Chungbuk exhibited the most substantial decrease in prevalence, plummeting from 361 per 100,000 in 2005 to 34 per 100,000 in 2022 (AAPC: -23.7%; 95% CI: -30.2, -16.5). Conversely, Gunwi-gun of Gyeongbuk experienced the highest increase, rising from 64 per 100,000 in 2005 to 87 per 100,000 in 2022 (AAPC: 3.0%; 95% CI: 1.1, 4.9), followed by Yecheon-gun of Gyeongbuk and Goseong-gun of Gangwon (Table 4).
The aim of this study was to identify areas requiring priority management of HCV infection by analyzing prevalence changes across different demographic and geographic parameters from 2005 to 2022. Notably, we observed a fluctuating pattern in HCV prevalence over the years, with an overall decline from 2005 to 2022, emphasizing the dynamic nature of HCV prevalence trends and the need for tailored intervention strategies.
Our findings revealed that, while there was a peak in age-, sex-, and area-adjusted HCV prevalence per 100,000 in 2007, subsequent years saw a continuous decline, reaching 97 per 100,000 in 2022. The APC indicated a significant overall decrease of -2.5% over the study period, with the AAPC including joinpoints further confirming a downward trend (-2.7% per year). Additionally, the incidence rate of HCV showed a notable downtrend from 78.3 per 100,000 in 2005 to 16.3 per 100,000 in 2022. However, there was an increase in all-cause mortality rate from 1.1% in 2005 to 1.6% in 2022, suggesting the need for continued vigilance in managing HCV-related complications.
The observed decline in HCV prevalence in this study can be explained by several key factors. Compared to 2005, the overall incidence rate in 2022 decreased by 79.2%, while all-cause mortality increased by 45.3%. Treatment rates also showed significant improvement, rising from 13.9% [21] during the interferon-based antiviral therapeutics (2009–2013) to an average of 56.8% [22] following the introduction of Direct-acting Antivirals (DAA) in 2018–2020. These factors are believed to have collectively contributed to the reduction in HCV prevalence in the study region.
Regarding regional prevalence, Busan, Jeonnam, and Gyeongnam consistently exhibited higher prevalence rates compared with the national average throughout the study period. Similarly, specific towns such as Seo-gu and Jung-gu of Busan and Jindo-gun of Jeonnam consistently showed high prevalence rates. Notably, Jeonnam demonstrated the most significant decrease in prevalence among regions, while Incheon exhibited the smallest reduction, indicating varied regional dynamics in HCV prevalence trends.
Comparison with previous studies revealed discrepancies in prevalence estimates, likely due to differences in study methodologies and population samples. The Korea National Health and Nutrition Examination Survey reported a prevalence of anti-HCV positivity among individuals aged 10 years or older of 0.75% in 2012 and 0.74% in 2021 [23]. Additionally, the 5-year prevalence of anti-HCV positivity (2012–2016) was reported as 0.66% (with a range of 0.56–0.78%) [3]. Furthermore, the age-, sex-, and area-adjusted prevalence of anti-HCV positivity among adults undergoing routine health check-ups at tertiary hospitals decreased from 0.78% in 2009 to 0.55% in 2015 [4, 6]. Notably, our study focused on diagnosed HCV patients, while other studies reported anti-HCV positivity in the general population, leading to variations in prevalence estimates.
Analysis at the town level highlighted several high-prevalence areas, with Boeun-gun of Chungbuk and Sunchang-gun of Jeonbuk showing particularly elevated prevalence rates, compared with previously identified high-prevalence towns. In Sunchang-gun of Jeonbuk, the Korea Disease Control and Prevention Agency initiated an epidemiological investigation into a specific clinic in March 2016 due to suspicions of a mass HCV outbreak. However, this suspected outbreak was not ultimately confirmed [24]. Factors contributing to these trends include access to healthcare services, population demographics, and regional healthcare infrastructure.
High-prevalence areas are characterized by significant outflows of the younger population and minimal inflows, leading to a faster rate of aging compared to other regions. Further research is needed on various factors such as socio-economic status, healthcare accessibility, and demographic characteristics that may influence HCV transmission in these regions.
Public awareness efforts regarding HCV infection are fundamentally necessary regardless of regional prevalence rates. A recent economic evaluation study demonstrated that biennial HCV screening could achieve elimination targets within 18 years [25], supporting the effectiveness of screening programs. While nationwide screening tests would be resource-intensive, implementing priority screening in regions with high prevalence or increasing trends would be a more practical and cost-effective approach for early detection and treatment. This targeted screening strategy could serve as a pilot program before considering nationwide expansion. Conversely, regions with low prevalence rates should maintain their status through continuous HCV education and prevention programs.
This study has several limitations. First, the prevalence may be underestimated due to insufficient data on undiagnosed and asymptomatic HCV cases. Our study, which used NHIS dataset, only includes information from patients who received diagnosis and treatment at medical institutions, potentially excluding HCV patients who did not seek treatment. These limitations may have been mitigated over time as awareness and diagnostic rates improved. Indeed, statistics show that public awareness of HCV among the general population increased from 10.4% in 2013 [26] to 34.0% in 2019 [27]. Second, while the joinpoint regression analysis used in this study is a useful tool for identifying trends and significant inflection points in HCV prevalence from past to present, it has limitations in predicting future prevalence patterns. Further research is needed to forecast future changes in HCV prevalence based on the trends identified in this study.
Our study provides valuable insights into the changing landscape of HCV prevalence in Korea, highlighting the need for continued surveillance and targeted interventions to achieve the WHO’s hepatitis elimination goals by 2030. Robust policies focusing on early screening and treatment in high-prevalence areas are essential to curb the spread of HCV and mitigate its associated health burden.
The data of this study can be accessed through the National Health Insurance System. However, it’s important to note that these data are subject to restrictions regarding their availability, as they were utilized under license specifically for this study and are therefore not accessible to the public. Nevertheless, Data are available from the authors upon reasonable request and with permission of Korea National Health Insurance. Further details can be found at the following link: https://nhiss.nhis.or.kr.
- AAPC:
-
Average annual percent change
- APC:
-
Annual percent change
- CI:
-
Confidence interval
- HBV:
-
Hepatitis B virus
- HCV:
-
Hepatitis C virus
- NHIS:
-
National Health Insurance Service
- WHO:
-
World Health Organization
This study used NHIS claims data (NHIS-2023-1-809) from the National Health Insurance Service.
This study was supported by a grant from the National Cancer Center, Republic of Korea (grant number: NCC-2310710).
The study was approved by the Institutional Review Board of the National Cancer Center (NCC2023-0026).
Since this study used secondary data that is open only to researchers meeting specific conditions, it was exempted from requiring informed consent according to regulations.
The Institutional Review Board of the National Cancer Center determined that informed consent was unnecessary due to the nature of the data.
Not Applicable.
The authors declare no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Choi, H., Ki, M. Temporal and geospatial patterns of hepatitis C virus prevalence: a longitudinal examination using national health insurance service data in the Republic of Korea (2005–2022). BMC Public Health 25, 1248 (2025). https://doi.org/10.1186/s12889-025-21777-6