Skin's Secret Warnings: Unlocking Early Clues to Devastating Health Crises

New research suggests that common skin conditions such as rashes or eczema could serve as significant indicators of a heightened risk for suicidal thoughts and depression, particularly in individuals who have experienced an episode of psychosis. This intriguing connection is rooted in the shared embryonic origin of the skin and brain, both developing from the same cellular layer in the womb known as the ectoderm. This common developmental pathway prompted scientists at the Gregorio Marañón Institute of Health Research in Spain to investigate a potential link between dermatological complaints and mental health conditions.
The Spanish research team conducted a study involving 481 patients who had recently experienced a first episode of psychosis, characterized by symptoms such as a loss of contact with reality, hallucinations, and delusions. Upon initial testing, 14.5 percent of these patients were found to exhibit dermatological symptoms, including rashes, itching, and photosensitivity. This trend was notably more prevalent among female patients, with 24 percent affected, compared to 10 percent of male patients.
All study participants received a four-week course of antipsychotic treatment. Following this period, their mental health parameters were re-evaluated. The findings revealed a critical distinction: patients who had experienced psychosis and were also suffering from co-occurring skin conditions displayed higher levels of depression and a significantly elevated risk of suicide compared to those without dermatological issues. Specifically, 25 percent of patients with skin conditions reported having suicidal thoughts or attempts, a stark contrast to just seven percent of patients who did not have skin conditions.
Lead researcher, Dr. Joaquín Galvañ, emphasized the profound implications of these findings, stating that "This discovery suggests that the presence of skin conditions indicates that these patients are more at risk for worse outcomes than patients who do not have skin conditions after a first episode of psychosis." He further noted that, if corroborated by subsequent studies, this finding has the potential to act as an invaluable "advance marker" for mental health risk. Similar to how a blood test can indicate a greater risk for cancer or heart disease, dermatological symptoms could pinpoint a subgroup of psychosis patients with a poorer clinical prognosis who might greatly benefit from early, tailored therapeutic interventions.
While it was previously established that between 30 to 60 percent of individuals with skin conditions also present with psychiatric symptoms, this study approached the relationship from the inverse perspective: investigating whether people with mental health problems also exhibit skin conditions, and what useful information this might provide. The precise reason for this connection remains to be fully elucidated, but the researchers' working hypothesis continues to be the common developmental origins of the skin and neurological systems. The findings of this groundbreaking study were presented at the European College of Neuropsychopharmacology (ECNP) meeting in Amsterdam.
Dr. Galvañ underscored the need for further research, stating, "As far as we know this is the first study to show this link in patients with psychosis, so we need follow-up studies to confirm the finding." He also called for investigations into whether this link extends to other psychiatric conditions, such as bipolar disorder, ADHD, anxiety, or general depression. This research builds upon existing knowledge, including the American Psychiatric Association's acknowledgment of the "many complex connections between skin conditions and mental health conditions," noting that over one-third of dermatological patients have psychological concerns. Psoriasis, atopic dermatitis, and eczema are among the skin diseases most commonly associated with co-occurring mental health conditions.
Further supporting this intricate relationship, a separate 2015 study conducted across 13 European countries found that 10 percent of dermatological patients suffered from depression, compared with 4.3 percent of control subjects. Anxiety was reported in 17.2 percent of these patients, and suicidal ideations were noted in 12.7 percent. Psoriasis, atopic dermatitis, eczema, and leg ulcers were identified as among the diseases most strongly associated with these psychiatric comorbidities, reinforcing the significance of the skin-brain axis in mental well-being.
You may also like...
Super Eagles Fury! Coach Eric Chelle Slammed Over Shocking $130K Salary Demand!
)
Super Eagles head coach Eric Chelle's demands for a $130,000 monthly salary and extensive benefits have ignited a major ...
Premier League Immortal! James Milner Shatters Appearance Record, Klopp Hails Legend!

Football icon James Milner has surpassed Gareth Barry's Premier League appearance record, making his 654th outing at age...
Starfleet Shockwave: Fans Missed Key Detail in 'Deep Space Nine' Icon's 'Starfleet Academy' Return!

Starfleet Academy's latest episode features the long-awaited return of Jake Sisko, honoring his legendary father, Captai...
Rhaenyra's Destiny: 'House of the Dragon' Hints at Shocking Game of Thrones Finale Twist!

The 'House of the Dragon' Season 3 teaser hints at a dark path for Rhaenyra, suggesting she may descend into madness. He...
Amidah Lateef Unveils Shocking Truth About Nigerian University Hostel Crisis!
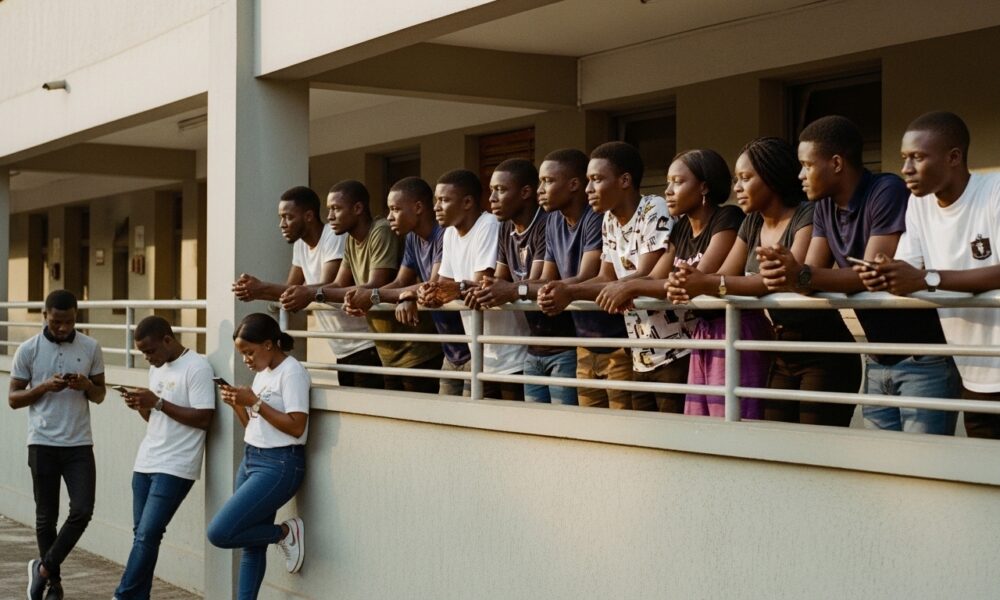
Many university students are forced to live off-campus due to limited hostel spaces, facing daily commutes, financial bu...
African Development Soars: Eswatini Hails Ethiopia's Ambitious Mega Projects

The Kingdom of Eswatini has lauded Ethiopia's significant strides in large-scale development projects, particularly high...
West African Tensions Mount: Ghana Drags Togo to Arbitration Over Maritime Borders

Ghana has initiated international arbitration under UNCLOS to settle its long-standing maritime boundary dispute with To...
Indian AI Arena Ignites: Sarvam Unleashes Indus AI Chat App in Fierce Market Battle

Sarvam, an Indian AI startup, has launched its Indus chat app, powered by its 105-billion-parameter large language model...


