Revolutionary Hope for Knee Pain Sufferers: Side-Effect Free Treatments on the Horizon!

For millions globally, persistent knee pain signals the insidious onset of osteoarthritis, a debilitating degenerative joint condition that severely impacts movement, making even simple acts like walking, climbing stairs, or standing agonizing. This pervasive disease affects nearly 10 million Britons and is projected to afflict a staggering one billion people worldwide by 2050. Despite its widespread scale and increasing burden, current treatment options remain notably limited, with no approved drugs capable of preventing the disease's progression. Alarmingly, up to 40 percent of patients with the most severe forms of osteoarthritis experience inadequate pain relief from commonly prescribed medications, contributing to over 100,000 individuals annually awaiting knee or hip replacement surgery on the NHS.
Osteoarthritis develops when the protective cartilage at the ends of bones gradually erodes over time. This breakdown leads to chronic pain, swelling, and increasing difficulty in joint movement as bone begins to rub directly against bone. In the absence of effective pharmaceutical interventions, many sufferers resort to lifestyle modifications such as exercise and weight loss to manage their symptoms. However, evidence suggests these approaches often fall short; a 2020 study in Arthritis Care and Research revealed that as many as 60 percent of knee osteoarthritis patients found little relief from non-pharmaceutical interventions.
Experts agree that there is a critical need for new treatment options. The past year has seen several promising developments, leading specialists to express quiet confidence that 2026 could mark a pivotal turning point in arthritis care. Professor Philip Conaghan, a specialist in arthritis and director of the Biomedical Research Centre at the University of Leeds, noted that while early-stage trials have offered hope, arthritis studies have historically struggled to deliver positive results in the crucial phase three trials required for widespread adoption. However, he highlights a couple of recent developments that genuinely appear to be viable new treatment options in the near future.
One such promising avenue is a new class of drugs known as neurotrophin inhibitors, which aim to target the biological drivers of knee pain itself, offering a distinct approach from traditional painkillers. Last year, a trial of an experimental drug called LEVI-04 in patients with symptomatic knee osteoarthritis yielded remarkable results, with participants reporting a 50 percent reduction in pain, alongside significant improvements in stiffness and physical function. This phase three study focused specifically on knee pain caused by osteoarthritis, the most common form of the disease and a leading cause of knee joint failure. Results from this critical final stage trial are anticipated this year.
Unlike conventional painkillers that merely mask symptoms, LEVI-04 is designed to switch off pain closer to its source. The drug specifically targets neurotrophin-3 (NT-3), a nerve-growth protein that becomes overactive in damaged knee joints. In osteoarthritis, elevated NT-3 levels encourage pain-sensing nerves to grow and become hypersensitive, causing everyday movements like walking or standing to trigger severe pain. LEVI-04 works by blocking NT-3, thereby effectively reducing pain signals originating directly from the knee joint, rather than just masking pain in the brain. The drug is administered via direct injection into the affected knee, allowing it to act locally and circumventing systemic side effects such as nausea or addiction. Researchers also suggest that, beyond pain reduction, LEVI-04 may help protect joint structure and slow further cartilage deterioration, although this aspect is still under investigation. Early evidence indicates that LEVI-04 does not share the same safety concerns that led to the shelving of previous neurotrophin-targeting drugs. Professor Conaghan, lead investigator on the LEVI-04 study, lauded the results as 'truly exceptional,' stating the drug could 'offer a vital new treatment option to millions of patients in huge need' and potentially represent a major breakthrough for osteoarthritis treatment if phase three trials replicate these findings.
Beyond pain management, researchers are also exploring whether new slimming jabs, specifically GLP-1 injections, could play a role in treating osteoarthritis, particularly in the knee. These drugs, already recognized for their benefits in liver disease, heart attack risk reduction, and slowing chronic kidney disease, may also offer 'real hope' for arthritis. A 2025 Taiwanese study involving nearly 1,000 knee osteoarthritis patients found that those receiving weight-loss injections were significantly less likely to require joint replacement surgery. This finding aligns with established evidence linking excess weight to osteoarthritis; one study found that for every five-point increase in BMI, the likelihood of developing the disease rises by 35 percent. While part of the explanation is mechanical, as extra weight places added strain on weight-bearing joints like the knees, accelerating cartilage wear, experts believe GLP-1 drugs may offer benefits beyond mere weight loss. Pharmaceutical companies, such as 4Moving Biotech, are investigating whether the effects of these drugs could be enhanced by direct injection into the affected joint. Professor Conaghan suggested there might also be an anti-inflammatory effect from GLP-1 drugs, adding, 'There is real potential that these medicines could have a significant impact on osteoarthritis care, and that is now getting closer.' However, it is important to note that arthritis is not yet included in prescribing guidelines for weight-loss injections.
Another groundbreaking development comes from the University of Cambridge, where researchers unveiled a 'revolutionary' form of artificial cartilage earlier this year. This soft, gel-like material is designed to sense subtle changes within the joint, such as those indicative of an arthritis flare-up, and precisely release medication when and where it is needed. Loaded with anti-inflammatory drugs, the material responds to small shifts in pH levels associated with inflammation. By mimicking the properties of natural cartilage while also serving as a targeted drug delivery system, researchers hope this gel could alleviate pain, reduce side effects, and provide more continuous treatment for arthritis patients, including those with knee disease. Nevertheless, experts, including Professor Conaghan, stress that significant questions remain, particularly regarding the specific drugs that would ultimately be incorporated into this innovative delivery system.
In a parallel development, French researchers recently reported promising early results from an immunotherapy drug – a treatment more commonly used in cancer care – in a small group of patients with knee osteoarthritis. This experimental vaccine targets interleukin-6, an inflammatory protein known to drive cartilage breakdown and joint inflammation, which often sees elevated levels during inflammatory flare-ups lasting weeks or months. By reducing these excess levels, the treatment aims to soothe symptoms and potentially limit further joint damage. In a study at the University of Paris Descartes, 18 of 24 knee osteoarthritis patients received three vaccine doses over 16 weeks, while six received placebo injections. After 42 weeks, vaccinated patients exhibited significantly lower levels of interleukin-6. While researchers described this as 'an encouraging first step,' experts like Professor Conaghan urge caution, citing past phase II trials of similar drugs that failed to deliver positive results. He emphasized that such treatments are likely to be effective only in a subset of patients, if at all, and there is currently no reliable method to identify these specific individuals.
Finally, the truth about a Brazilian herbal treatment has also garnered attention. Last year, a study in mice suggested that an ancient Brazilian herb, Alternanthera littoralis (commonly known as Joseph's Coat), could help ease knee pain linked to osteoarthritis. The research indicated that this native species, found in Brazil's coastal regions and traditionally used for bacterial, fungal, and parasitic infections, reduced swelling, inflammation, pain, and stiffness in affected joints. Compounds within the plant produced effects similar to some current pain-relief drugs for osteoarthritis. Scientists at the Federal University of Grande Dourados, writing in the Journal of Ethnopharmacology, noted its 'significant anti-inflammatory, analgesic and anti-arthritic effects,' reinforcing its traditional use and highlighting its potential as a therapeutic candidate. However, this research is at a very early stage, based solely on animal experiments, with further studies required before any human trials. Professor Conaghan cautioned, 'It is simply too early to say whether this will prove effective in patients.'
You may also like...
Super Eagles Fury! Coach Eric Chelle Slammed Over Shocking $130K Salary Demand!
)
Super Eagles head coach Eric Chelle's demands for a $130,000 monthly salary and extensive benefits have ignited a major ...
Premier League Immortal! James Milner Shatters Appearance Record, Klopp Hails Legend!

Football icon James Milner has surpassed Gareth Barry's Premier League appearance record, making his 654th outing at age...
Starfleet Shockwave: Fans Missed Key Detail in 'Deep Space Nine' Icon's 'Starfleet Academy' Return!

Starfleet Academy's latest episode features the long-awaited return of Jake Sisko, honoring his legendary father, Captai...
Rhaenyra's Destiny: 'House of the Dragon' Hints at Shocking Game of Thrones Finale Twist!

The 'House of the Dragon' Season 3 teaser hints at a dark path for Rhaenyra, suggesting she may descend into madness. He...
Amidah Lateef Unveils Shocking Truth About Nigerian University Hostel Crisis!
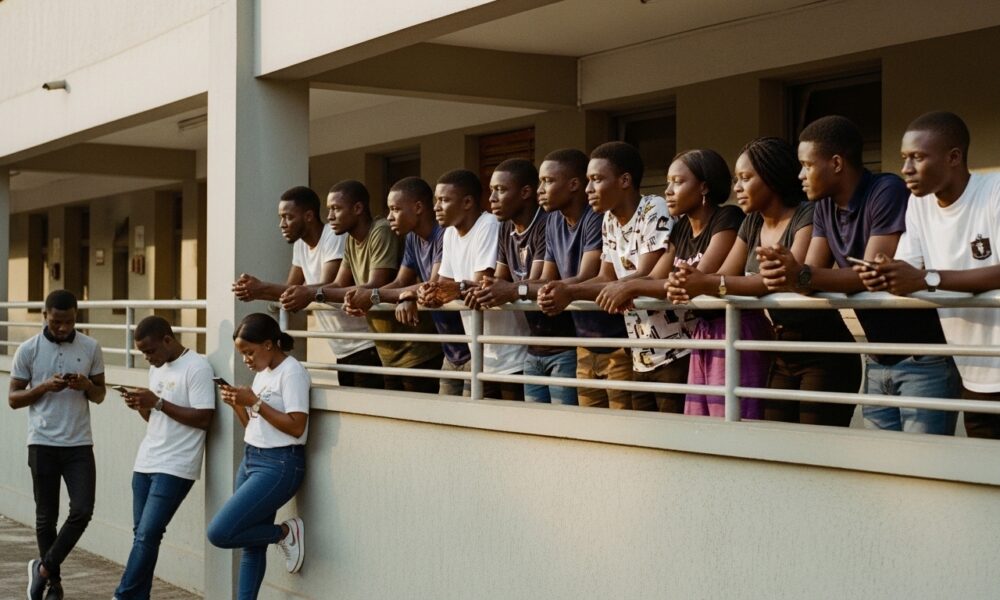
Many university students are forced to live off-campus due to limited hostel spaces, facing daily commutes, financial bu...
African Development Soars: Eswatini Hails Ethiopia's Ambitious Mega Projects

The Kingdom of Eswatini has lauded Ethiopia's significant strides in large-scale development projects, particularly high...
West African Tensions Mount: Ghana Drags Togo to Arbitration Over Maritime Borders

Ghana has initiated international arbitration under UNCLOS to settle its long-standing maritime boundary dispute with To...
Indian AI Arena Ignites: Sarvam Unleashes Indus AI Chat App in Fierce Market Battle

Sarvam, an Indian AI startup, has launched its Indus chat app, powered by its 105-billion-parameter large language model...