NHS 'Ghost' Scandal Unveiled: Millions Falsely Registered, Billions Wasted
An alarming investigation by the Daily Mail has revealed a significant and persistent issue within England's National Health Service (NHS) GP system: an all-time high of 4.9 million 'ghost patients' are currently registered. This discrepancy, representing a 95% increase in a decade, means an estimated £838 million annually is allocated to General Practices for patients who may have died, moved abroad, or are duplicates. This sum is more than the combined populations of Kent, Essex, and Hampshire, highlighting a systemic failure in record-keeping despite ministerial pledges a decade ago to tackle the problem.
The concept of 'ghost patients' refers to individuals who remain on GP patient lists but are no longer eligible. Surgeries in England typically receive an average of £169.74 for each patient on their books, irrespective of whether they provide active care to them. This funding, channeled from a ring-fenced 'global sum payments' budget operated by NHS England (which topped £4.6 billion this year), is primarily intended to cover practice running costs, including heating, lighting, maintenance, and staff salaries. After these outgoings, any remaining funds are shared among partners, deducting their expenses. While there is no direct suggestion that GPs are intentionally abusing the system for personal financial gain, critics argue that the substantial funds allocated to non-existent patients could otherwise be utilized to address critical shortages, such as funding the training of an additional 22,000 nurses, according to the Royal College of Nursing.
Efforts to resolve this issue have been protracted and largely ineffective. The NHS Counter Fraud Authority initiated an investigation into potential system abuses in 2019, but this work was paused due to the COVID-19 pandemic and difficulties in obtaining core data, with no immediate plans to revisit it. Outsourcing firm Capita was initially engaged in 2015 to clean up GP lists but faced budget cuts, leading to a halt in their work until 2018. Their mandate shifted to a triennial cleansing process, checking records of patients registered as over 100 years old. More recently, in September, new rules were adopted, requiring Primary Care Support England (managed by Capita) to automatically flag patients who may have moved. Surgeries now have three months, down from six, to confirm a patient's address.
Analysis based on NHS Digital statistics, conducted before the new rules were tightened, revealed a stark contrast: 63.8 million patients were registered at GP practices as of September 1, compared to the Office for National Statistics' (ONS) projection of 58.8 million for the nation's population in 2025 – a 4.9 million discrepancy. This issue is particularly acute in certain regions, with some parts of England showing up to 20 percent of registered patients potentially non-existent. Notably, North West London sub-ICB W2U3Z reported a 31.5% disparity, registering 2.9 million patients against an actual population of 2.2 million. Other regions with significant discrepancies include Humber and North Yorkshire (29.7%), Lancashire and South Cumbria (25.8%), and Greater Manchester (23.7%). North West London's sub-ICB attributed its high figures to London's significant population mobility and the registration patterns reflecting services like 'GP at Hand,' a digital-first practice.
The persistent problem has drawn sharp criticism from various stakeholders. Shimeon Lee of the TaxPayers' Alliance deemed it a 'damning indictment of the failure of the NHS bureaucracy,' advocating for drastic reforms. Sir Geoffrey Clifton-Brown MP, chair of the public accounts committee, lamented the 'failure of recordkeeping' and the 'glacial' pace of digital transformation within the NHS, accusing the Department of Health and Social Care and NHS England of complacency. Dr. Luisa Pettigrew from the Health Foundation linked the growing mismatch to delays in removing individuals, duplicate records, and high population mobility, while also noting instances of 'under coverage' where individuals are not registered or are inappropriately removed.
Conversely, medical associations and practicing GPs argue against the notion of deliberate fraud. The British Medical Association (BMA) and Royal College of GPs (RCGP) contend that 'ghost patients' are primarily a records management issue, exacerbated by high patient mobility (people moving, dying, or leaving the country) and the significant bureaucratic burden of constantly purging lists. Dr. Katie Bramall, BMA GP committee chair, stated that practices, despite their best efforts, cannot maintain 100% accurate information without a constant stream of accurate data and robust support from Primary Care Support England. Professor Kamila Hawthorne, RCGP chair, added that accurate patient registers are in a practice’s interest for achieving clinical targets and payments. Dr. Patrick Burch, a practicing GP and researcher, pointed to the high mobility of patients and the inability of under-funded and overworked GPs to consistently track patient status, warning against reducing practice funding based on inaccurate list sizes.
Beyond the financial misallocation, critics also express concern that inflated patient lists might be used politically. Unions have reportedly leveraged rising patient-to-GP ratios to demand increased funding for more staff. The BMA states the average GP is now responsible for 2,247 patients, an increase of 309 since 2015, exceeding the widely accepted safe limit of 1,800. This ongoing debate about ghost patients occurs amidst a separate row over new rules introduced on October 1, requiring GP surgeries to keep online forms open for the duration of working hours for non-urgent requests, a move that has led the BMA to hint at potential strikes due to concerns about increased workload without additional staff or adequate safeguards. Health Secretary Wes Streeting has, however, vowed not to back down on these changes, highlighting the deep-seated challenges facing England's primary care system.
You may also like...
Super Eagles Fury! Coach Eric Chelle Slammed Over Shocking $130K Salary Demand!
)
Super Eagles head coach Eric Chelle's demands for a $130,000 monthly salary and extensive benefits have ignited a major ...
Premier League Immortal! James Milner Shatters Appearance Record, Klopp Hails Legend!

Football icon James Milner has surpassed Gareth Barry's Premier League appearance record, making his 654th outing at age...
Starfleet Shockwave: Fans Missed Key Detail in 'Deep Space Nine' Icon's 'Starfleet Academy' Return!

Starfleet Academy's latest episode features the long-awaited return of Jake Sisko, honoring his legendary father, Captai...
Rhaenyra's Destiny: 'House of the Dragon' Hints at Shocking Game of Thrones Finale Twist!

The 'House of the Dragon' Season 3 teaser hints at a dark path for Rhaenyra, suggesting she may descend into madness. He...
Amidah Lateef Unveils Shocking Truth About Nigerian University Hostel Crisis!
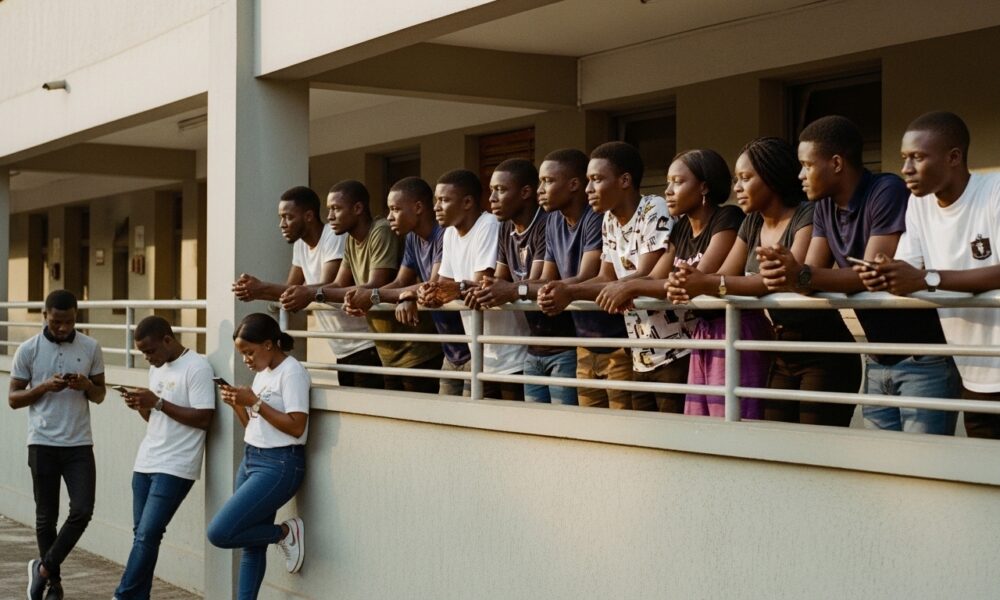
Many university students are forced to live off-campus due to limited hostel spaces, facing daily commutes, financial bu...
African Development Soars: Eswatini Hails Ethiopia's Ambitious Mega Projects

The Kingdom of Eswatini has lauded Ethiopia's significant strides in large-scale development projects, particularly high...
West African Tensions Mount: Ghana Drags Togo to Arbitration Over Maritime Borders

Ghana has initiated international arbitration under UNCLOS to settle its long-standing maritime boundary dispute with To...
Indian AI Arena Ignites: Sarvam Unleashes Indus AI Chat App in Fierce Market Battle

Sarvam, an Indian AI startup, has launched its Indus chat app, powered by its 105-billion-parameter large language model...

