Mind-Blowing Breakthrough: New Study Uncovers Unified Cause for Mental Illnesses, Revolutionizing Treatment!

An international team of scientists has made a groundbreaking discovery: a wide range of mental disorders share common genetic roots, a finding that promises to revolutionize treatment by making it simpler and more effective. Currently, mental illnesses such as bipolar disorder, depression, and anxiety are often treated as distinct conditions, necessitating multiple medications that may target different mechanisms and lead to various side effects. This new research suggests a fundamental interconnectedness.
By comprehensively mapping the entire human genome, which serves as a complete blueprint of human DNA, researchers identified 101 specific regions on human chromosomes where genetic variations contribute to an increased risk of suffering from multiple psychiatric conditions simultaneously. This shared genetic architecture enabled scientists to categorize these disorders into five distinct groups. Notably, a key region on chromosome 11 was found to be connected to eight different conditions, including schizophrenia and depression.
The five distinct groups identified are Substance Use Disorders, Internalizing Disorders, Neurodevelopmental Disorders, Compulsive Disorders, and a group encompassing Schizophrenia and Bipolar Disorder (SB group). Many patients currently navigate a complex treatment landscape, often taking multiple medications because initial drugs were ineffective or caused intolerable side effects, or due to co-occurring diagnoses.
The Substance Use Disorders cluster, which includes conditions like alcohol and opioid dependence, reveals shared genetic underpinnings. These likely influence common underlying mechanisms such as reward processing, impulse control, response to stress, and potentially the metabolic pathways involved in processing drugs.
Internalizing Disorders, comprising depression, anxiety, and post-traumatic stress disorder (PTSD), represent one of the most genetically interconnected groups identified. These three conditions exhibited the highest level of shared genetic risk, meaning that genetic factors influencing susceptibility to one disorder tend to influence the others as well. This strong overlap helps explain why individuals diagnosed with one of these conditions frequently meet the criteria for another, either concurrently or over their lifetime. Approximately 48 million Americans have experienced depression or are undergoing treatment for it, and 40 million suffer from anxiety, with these conditions often overlapping. The percentage of adults reporting a depression diagnosis has reached 29 percent, nearly 10 percentage points higher than in 2015.
Neurodevelopmental Disorders are rooted in early brain development and are primarily defined by a strong shared genetic foundation between autism spectrum disorder (ASD) and attention-deficit/hyperactivity disorder (ADHD). This significant genetic overlap suggests that a core set of genes influences early brain development, shaping connectivity, synaptic function, and the regulation of attention and social behavior. This helps to explain why autism and ADHD frequently co-occur and share symptoms like challenges with executive function and social interaction. While Tourette's Syndrome showed a weaker genetic link to this cluster, it shares some risk factors with ASD and ADHD, likely in motor control and impulse regulation, but is also driven by its own distinct genetic mechanisms.
The Compulsive Disorders cluster is characterized by a strong genetic link between anorexia and obsessive-compulsive disorder (OCD), disorders centered on intrusive thoughts and repetitive behaviors. This overlap suggests that inherited biological pathways related to cognitive control, perfectionism, behavioral rigidity, and reward processing contribute to both the ritualistic behaviors observed in OCD and the restrictive, compulsive eating patterns central to anorexia.
The Schizophrenia and Bipolar Disorder (SB) group demonstrated the most significant genetic overlap, approximately 70 percent. This substantial shared set of genetic risk factors influences fundamental brain functions and development pathways common to both bipolar disorder and schizophrenia. This explains their well-documented clinical overlap, including shared symptoms like psychosis, frequent misdiagnosis, and the occurrence of both disorders within families.
This groundbreaking understanding paves the way for a new era of personalized medicine. In the future, a simple genetic profile, potentially revealed through a blood test, could pinpoint a person's specific risk patterns, such as a high genetic tendency for depression, anxiety, or PTSD. Doctors could then utilize this information to select the most effective medication or therapy from the outset, moving beyond the current trial-and-error approach. For example, if a patient's anxiety is genetically linked to the Internalizing cluster, it would guide a doctor toward one set of preferred treatments, whereas a genetic tie to the Compulsive cluster would indicate a completely different therapeutic strategy.
Currently, pharmacogenetic tests, such as GeneSight or Genomind, are available and often offered by psychiatrists. These tests analyze how an individual's genes affect their metabolism of specific psychiatric medications, helping to predict which drugs they may tolerate better or process poorly. This reduces side effects and shortens the trial-and-error period. However, the ability to biologically subtype a disorder into specific genetic clusters, such as definitively classifying someone's depression as of the 'Internalizing' type or the 'SB' type based on genetics, is still in the early research phase.
You may also like...
NBA Bombshell: LeBron James and Ayton Out for Pacers Clash!

The Los Angeles Lakers will be severely impacted by injuries, with LeBron James, Deandre Ayton, and Maxi Kleber all side...
Man City Stays: Pep Guardiola Drops Major Hint on Future!

Pep Guardiola has hinted at staying at Manchester City, expressing confidence that his team will reach its full potentia...
HBO's New Crime Thriller Dethrones 'A Knight of the Seven Kingdoms' in Streaming Battle
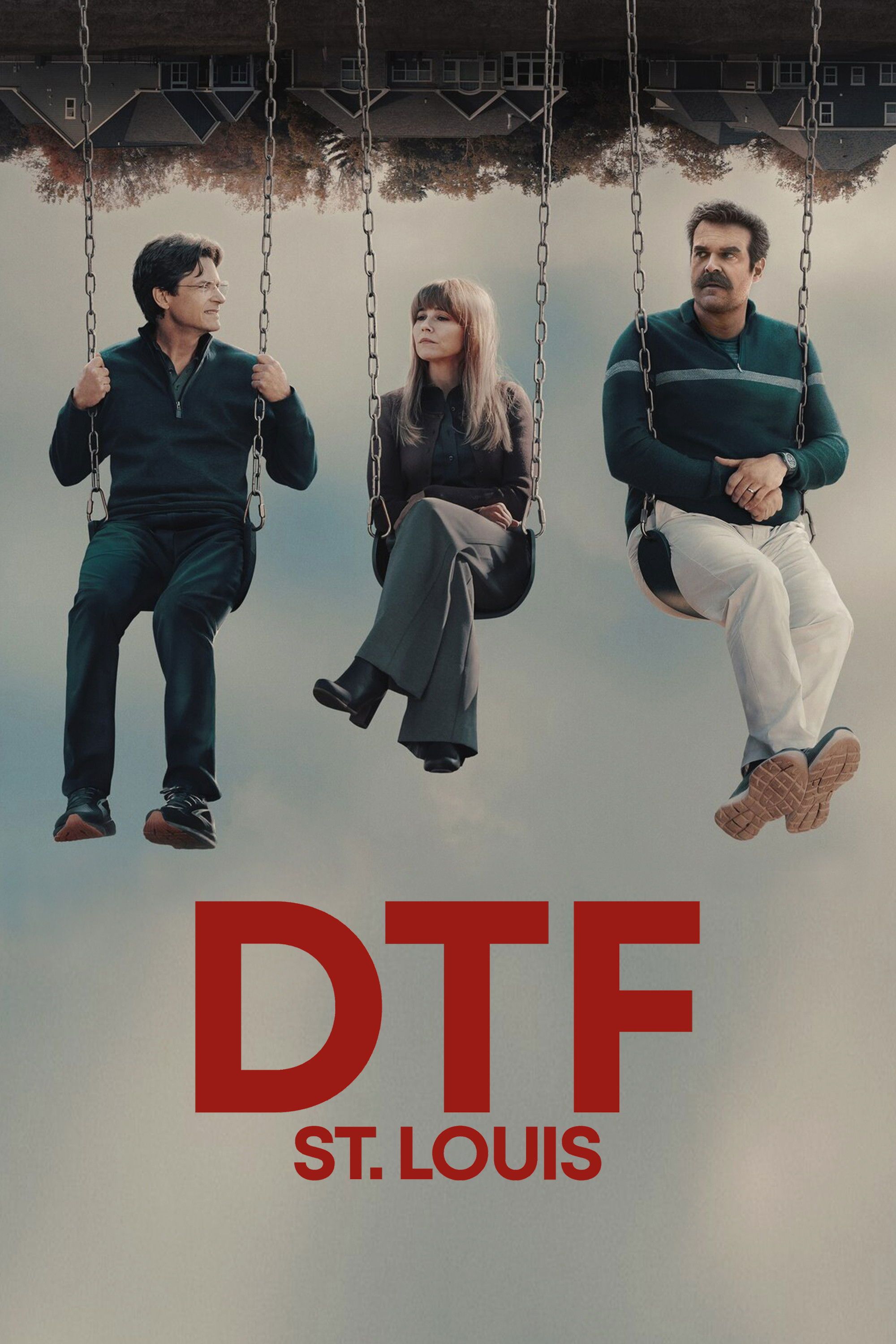
HBO Max is currently showcasing two notable series: 'DTF St. Louis,' a star-studded crime story praised for its blend of...
SZA Slams Chart Predictions, Defying Taylor Swift Comparison: 'Anything Is Possible!'

SZA's album SOS defied expectations by topping the Billboard 200 over Taylor Swift, a feat her label initially doubted. ...
Sam Asghari Demands Privacy Amid Britney Spears’ DUI Arrest After Explosive Comments

Sam Asghari has addressed Britney Spears' recent DUI arrest during a Fox News interview, calling for privacy for his ex-...
Giant Meets Miniature! World's Tallest Dog Shares Paws With the Smallest Canine Star!

The world's shortest dog, Pearl the Chihuahua, and a towering Great Dane named Reggie, had an unforgettable playdate arr...
End of an Era: Girl Scouts Announce Retirement of Two Beloved Cookie Flavors After 2025 Season!

Girl Scout cookie season is officially underway, but fans should prepare to say goodbye to Toast-Yay! and S’mores, which...
Unlock Peak Performance: Timing Magnesium for Ultimate Muscle Recovery
:max_bytes(150000):strip_icc()/Health-GettyImages-MagnesiumBeforeOrAfterWorkout-1012169458424c3791686bd6c68427e5.jpg)
Magnesium is vital for athletes, supporting muscle function, energy, and recovery, with increased demands during intense...
:max_bytes(150000):strip_icc()/HDC-GettyImages-2198830465-93292bb601a245b3a439c59d1c0e6a1c.jpg)



