Your Bones Aren’t as Solid as You Think; They’re Constantly Rebuilding Themselves
When most people picture the human skeleton, they imagine something firm and static. Bones are often described as structures built once and left unchanged. This impression is understandable because bone tissue does feel solid, and it is strong enough to withstand significant force.
However, far from being lifeless support beams, the bones are among the most dynamic tissues in the human body. This misconception makes the reality surprising: your skeleton is constantly in motion. Without your awareness, tiny sections of your bone tissue are being broken down and rebuilt every day.
What Your Bones Are Really Made Of
Bones are made up of a framework of a protein called collagen, with a mineral matrix made primarily of calcium and phosphate. These minerals form crystals that give bones their stiffness and compressive strength. Collagen is a fibrous protein, and gives bones tensile strength and a slight elasticity. This combination of rigid minerals and flexible protein makes bone tissue uniquely suited for everyday life.
Bone structure also varies depending on location and function. On the outside of most bones is compact bone, dense and tightly packed. It forms the sturdy walls of long bones and the outer layers of flat bones. Deeper inside lies spongy bone, which is not actually soft but looks more like a honeycomb, filled with small spaces. This arrangement reduces weight while maintaining strength and absorbs shocks from movement. The spaces within spongy bone also house bone marrow, where blood cells are produced. Together, these layers allow bones to be both strong and efficient, supporting the body without being overly heavy.
The Cells Behind Constant Remodeling
The dynamic behavior of bone tissue is driven by three primary types of cells that work in coordination. Osteoblasts, which are the builders. These cells produce a new bone matrix, secreting collagen and initiating the mineralization process that hardens the tissue. They line the surfaces where new bone tissue is needed. Osteocytes are the managers and communicators. They sit within small cavities inside the bone and form an interconnected network which allows them to sense stress and microscopic damage, then they reinforce or remove as necessary.
The third key cell type is the osteoclast. These cells handle the breakdown of bone tissue. They attach to bone surfaces and secrete acids and enzymes that dissolve the mineral and collagen components. This removal of old or damaged bone tissue is essential because it clears space for new tissue to be built. The actions of osteoclasts and osteoblasts are tightly coordinated because as breakdown increases, rebuilding must increase as well to maintain stability.
This cellular balance is called bone remodeling. It is a continuous process where small packets of bone tissue are resorbed by osteoclasts and then replaced by osteoblasts. This ensures that bone tissue remains strong, efficient and responsive.
The Remodeling Cycle
Bone remodeling begins in early childhood and continues throughout life. In children and adolescents, the process is especially active because the skeleton is still growing. Growth plates at the ends of long bones control lengthening, while remodeling shapes the thickness and curvature of bones to accommodate changes in size and activity.
In adulthood, growth stops, but remodeling continues. The purpose shifts from building new bones for growth to maintaining and repairing existing bones. Simple daily activities often create micro-damage in bone tissue and though the tiny cracks are too small to feel, they're enough to weaken the structure if ignored. Remodeling detects and fixes them long before they can accumulate. The rate of remodeling varies among individuals but averages around ten percent of the skeleton per year. This means that every decade, nearly the entire set of bones in the body has been renewed. As people age, the remodeling cycle becomes less balanced. Osteoclasts often remain active, breaking down bone tissue at a consistent pace, but osteoblasts may slow their building activity. This imbalance leads to gradual bone loss. Age-related remodeling also becomes less effective at repairing micro-damage, increasing the risk of fractures.
How Lifestyle Shapes Your Skeleton
The adaptability of bone tissue makes it sensitive to the choices people make and physical activity is one of the most influential factors that shape the skeleton. Bones respond to mechanical loading, meaning the force placed on them through movement and exercises stimulates remodeling. Even simple consistent movements signal to bone cells that reinforcement is necessary.

Conversely, lack of activity has significant consequences. When bones do not receive regular mechanical stimulation, remodeling shifts toward removal rather than maintenance. Hormones and nutrition also play a role in shaping bone tissue. Without adequate intake of proper nutrients, the body draws minerals from the skeleton, gradually weakening bone tissue.
Environmental and cultural factors also contribute. Diets low in calcium or high in processed foods can affect bone density over time. Certain lifestyles that limit sun exposure may reduce vitamin D synthesis, affecting bone health. Generally, the skeleton is a long-term reflection of how a person lives.
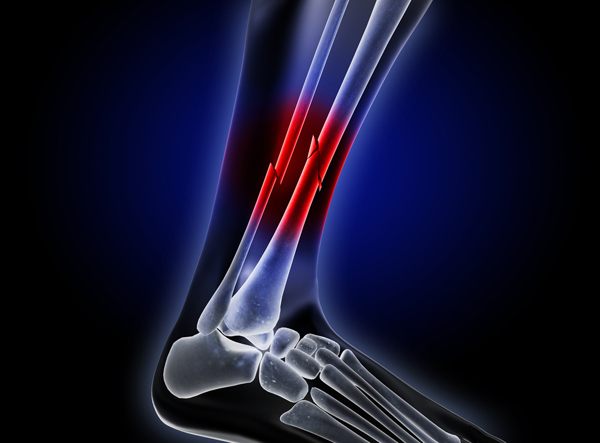
How Broken Bones Heal
Fractures occur in various ways, from sudden impacts to repeated stress. Healing begins immediately after a fracture. Blood vessels in the bone and surrounding tissue rupture, forming a clot at the site. This clot initiates an inflammatory response, which attracts cells that clear debris and signal the start of repair. Within days, a soft callus made of collagen and cartilage forms around the fracture, bridging the gap between broken ends. Over the next several weeks, the soft callus is replaced by a hard callus as minerals are deposited. Osteoblasts play a central role during this phase, building a rough form of new bone tissue. The fracture site becomes rigid and can begin to withstand movement and pressure. Although the bone is still weaker than surrounding tissue, it is functional.
The final phase is remodeling, which can last months to years. During this stage, osteoclasts and osteoblasts refine the newly formed bone tissue, restoring its original shape and internal structure. In some cases, the healed area becomes denser and stronger than before the injury because remodeling reinforces regions that experienced high stress. However, factors like age, nutrition, blood supply and underlying health conditions can influence the speed and quality of repair.
What Happens When the System Fails
Bone remodeling depends on a careful balance between breakdown and rebuilding. When this balance is disrupted, bone health can decline. Osteoporosis is one of the most common conditions resulting from remodeling failure. It occurs when bone resorption outpaces bone formation, leading to decreased density and increased fragility. People with osteoporosis are more susceptible to fractures, particularly in the spine, hip and wrist. Age is one of the strongest causes of this, as bone-building activity naturally slows over time. Hormonal changes too, especially decreased estrogen levels during menopause, affect the remodeling cycle. Genetics, physical activity levels, diet and overall health also play roles. Osteopenia, a milder form of bone loss, can precede osteoporosis and serves as a warning sign that the remodeling system is under strain.
Stress fractures represent another type of imbalance. They occur when repetitive force overwhelms the remodeling process. Instead of repairing micro-damage effectively, the system falls behind, allowing cracks to enlarge. Certain medical conditions, such as hyperparathyroidism or chronic inflammatory diseases, can also disrupt remodeling. Medications like corticosteroids may impair bone-building activity, leading to long-term density loss if used extensively.
Children and adolescents can experience growth plate injuries when the bone tissue responsible for lengthening is damaged. Inflammatory diseases, malnutrition or hormonal imbalances can affect bone development. When the natural rhythm of breakdown and rebuilding falters, the consequences reveal how dependent the skeleton is on continuous cellular activity.
A Skeleton That Never Stops Changing
Although the skeleton may appear unchanging, it is one of the busiest systems in the human body. Its ability to rebuild itself continuously allows it to support movement, protect organs and recover from injuries. The cycle of remodeling ensures that your bones remain strong throughout life, even as circumstances and demands change.
The idea that your bones are not as solid as they seem should not be alarming. Instead, it highlights the remarkable resilience of the human body. The human skeleton is a living record of how a person moves, grows and ages. Understanding its dynamic nature encourages a more informed approach to bone health and a deeper appreciation for the complexity of the body’s internal structures.
You may also like...
Super Eagles Fury! Coach Eric Chelle Slammed Over Shocking $130K Salary Demand!
)
Super Eagles head coach Eric Chelle's demands for a $130,000 monthly salary and extensive benefits have ignited a major ...
Premier League Immortal! James Milner Shatters Appearance Record, Klopp Hails Legend!

Football icon James Milner has surpassed Gareth Barry's Premier League appearance record, making his 654th outing at age...
Starfleet Shockwave: Fans Missed Key Detail in 'Deep Space Nine' Icon's 'Starfleet Academy' Return!

Starfleet Academy's latest episode features the long-awaited return of Jake Sisko, honoring his legendary father, Captai...
Rhaenyra's Destiny: 'House of the Dragon' Hints at Shocking Game of Thrones Finale Twist!

The 'House of the Dragon' Season 3 teaser hints at a dark path for Rhaenyra, suggesting she may descend into madness. He...
Amidah Lateef Unveils Shocking Truth About Nigerian University Hostel Crisis!
Many university students are forced to live off-campus due to limited hostel spaces, facing daily commutes, financial bu...
African Development Soars: Eswatini Hails Ethiopia's Ambitious Mega Projects

The Kingdom of Eswatini has lauded Ethiopia's significant strides in large-scale development projects, particularly high...
West African Tensions Mount: Ghana Drags Togo to Arbitration Over Maritime Borders

Ghana has initiated international arbitration under UNCLOS to settle its long-standing maritime boundary dispute with To...
Indian AI Arena Ignites: Sarvam Unleashes Indus AI Chat App in Fierce Market Battle

Sarvam, an Indian AI startup, has launched its Indus chat app, powered by its 105-billion-parameter large language model...


:max_bytes(150000):strip_icc()/Health-GettyImages-2081542939-b98aef06468d40a7a2ad33ca1ff25832.jpg)