Revolutionary or Risky? 'Weight Loss Jabs' Show Promise in Children as Young as Six

A recent study indicates that weight loss medications, known as GLP-1 agonists, hold significant potential for children as young as six who are struggling with obesity or type 2 diabetes. The research suggests these drugs can substantially improve blood sugar control and lead to weight reduction in youngsters, although common side effects are noted.
Researchers from the University of Florida in the United States conducted a comprehensive review of 18 trials, involving a total of 1,402 children aged between six and 17. The studies compared the efficacy of GLP-1 agonists against placebo treatments in participants diagnosed with obesity, being overweight, having pre-diabetes, or type 2 diabetes. GLP-1 agonists work by mimicking a natural hormone, which in turn reduces appetite, slows food digestion, and lowers blood sugar levels.
The analysis revealed promising outcomes for children receiving these drugs for obesity treatment, demonstrating an average weight loss of 4.72kg and a reduction in waist circumference by 3.81cm. However, the study also highlighted that 'gastrointestinal adverse events,' such as nausea, vomiting, diarrhoea, and constipation, were 'significantly more common' among those administered the drugs compared to the placebo group. The findings, published in the journal JAMA Pediatrics, affirmed that GLP-1 receptor agonists (GLP-1RAs) were effective in enhancing glycemic control, weight, and cardiometabolic outcomes in children and adolescents. Importantly, the review found no significant differences in rates of suicidal ideation, behaviours, or depression between the drug and placebo groups, though gastrointestinal side effects remain a key consideration for long-term usage. The researchers further stressed the necessity of longer follow-up periods in future trials and more real-world studies to definitively establish the long-term effects of GLP-1 RAs in younger populations.
Currently, GLP-1 agonists are available on the NHS in England for managing weight or treating type 2 diabetes, but their use is specifically recommended for adults. The trials examined in this review largely utilized older versions of these weight loss injections. Newer generations of GLP-1 agonists, such as Wegovy (containing semaglutide) and Mounjaro (tirzepatide), have demonstrated superior efficacy in adults. Previous studies have shown adults receiving semaglutide injections lost an average of 14 percent of their body weight over 72 weeks, while those on tirzepatide, often referred to as the 'king kong' of weight-loss jabs, achieved a 20 percent body weight reduction over the same duration.
The broader context of childhood obesity in England reveals that 22.1 percent of children in Year 6 (aged 10 to 11) were obese in 2023/24, a slight decrease from 22.7 percent in 2022/23. Despite this being the third consecutive year of decline, the figure remains higher than pre-pandemic levels. Furthermore, the Government’s national child measurement programme reported that approximately one in ten children entering primary school in England were obese in 2023/24, an increase from 9.2 percent in the previous year.
Commenting on these findings, Professor Naveed Sattar, a professor of cardiometabolic medicine at the University of Glasgow, observed that while obesity levels are rising fastest in younger individuals, the current meta-analysis predominantly focused on trials involving older GLP-1RAs, which are known to yield considerably less weight loss compared to newer, higher doses of semaglutide and tirzepatide. He emphasized the ongoing need for trials involving these newer, more potent agents in children with type 2 diabetes. Professor Sattar acknowledged that the reported safety profiles for older medicines in the meta-analysis are largely reassuring but called for more extensive safety assessments for newer medications, including their potential impacts on growth and puberty, and a clearer understanding of the required duration of treatment. Ultimately, he highlighted that drug-based interventions alone cannot solve childhood obesity, stressing that prevention through modifying the obesogenic environment is paramount, albeit an incredibly challenging task that no country has yet fully overcome.
You may also like...
Hidden Truths: Premier League Performances Go Deeper Than Just Results!
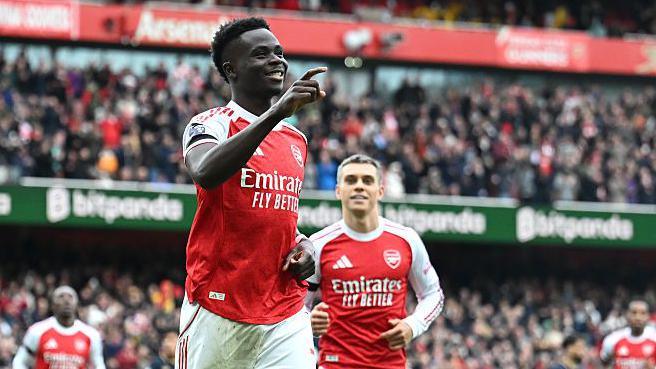
Beyond the Premier League table, Expected Goals (xG) offers a crucial metric for evaluating team performance, revealing ...
Netflix Renews 'Splinter Cell: Deathwatch' for Season 2 After Uncertain Start

Netflix has officially renewed “Splinter Cell: Deathwatch” for a second season, confirming an earlier two-season order f...
Ice Spice Shakes Up Paris Fashion Week With 'Baddie Baddie' Twerk Video

Ice Spice has unveiled her new "Baddie Baddie" music video, featuring supermodel Anok Yai and Olympic gymnast Suni Lee. ...
Selena Gomez's Raw Confession: Why She 'Sobbed' After Marrying Benny Blanco

Selena Gomez opened up at Fortune’s Most Powerful Women conference about her persistent irrational fears, despite her re...
Heartbreak After Death: Liam Payne's Secret 'Goodbye' Letter Discovered

Liam Payne's girlfriend, Kate Cassidy, recently discovered a heartfelt goodbye note from the late singer days before the...
Britney Spears Unleashes Fury: Denies Shocking Knife Allegations

Kevin Federline's forthcoming memoir contains startling allegations about Britney Spears's behavior, including claims of...
West Africa's Tech Future Unfolds: Registration Opens for NITDA Co-Create Exhibition

The NITDA Co-Create West Africa Tech Exhibition is set to showcase cutting-edge innovations and trends across diverse te...
KingsChat's Explosive Growth: Christ Embassy's Social App Surpasses 2 Million Users

KingsChat, a Nigerian social media app owned by Christ Embassy, is quietly dominating the app market with over 2 million...




