Revolutionary Blood Test Detects Deadly Motor Neurone Disease with Flawless Accuracy

Scientists have developed a groundbreaking blood test capable of detecting motor neurone disease (MND), also known as amyotrophic lateral sclerosis (ALS), in its earliest stages with remarkable accuracy, even before the onset of symptoms. The innovative test boasts a 97 per cent accuracy rate for identifying patients with the condition and a 93 per cent accuracy rate for ruling it out in healthy individuals.
The test was developed by researchers at the US-based not-for-profit Brain Chemistry Labs. Their work involved analyzing 788 blood samples, roughly split between patients with MND/ALS and those without the illness. The scientists focused on microRNAs, tiny fragments of genetic material present in the blood that play a crucial role in regulating cell function. Patterns of these microRNAs can change in the presence of disease, making them valuable potential biomarkers for illness.
Specifically, the research team identified eight distinct microRNAs linked to motor neurone disease. The initial biomarker parameters were established using 449 individual blood samples. Subsequently, a laboratory technique called quantitative polymerase chain reaction (qPCR) was employed to rapidly analyze the remaining samples and validate the test's diagnostic precision. Dr Rachel Dunlop, a senior researcher at Brain Chemistry Labs, highlighted the profound impact of this development, stating that it 'means that patients can initiate therapy early in the disease.'
Motor neurone disease is a rare, progressive neurological condition that devastates the nerves controlling movement, rapidly leading to muscle weakness, paralysis, and ultimately death. Around 5,000 adults in the UK currently live with MND, with ALS being its most common form. While symptoms typically appear between the ages of 55 and 75, early signs can include muscle twitches, a weak grip, weakness in the leg or ankle, slurred speech, and unexplained weight loss. For most patients, life expectancy ranges from two to five years after symptom onset, though progression rates can vary significantly.
A major challenge in managing ALS has been the significant delays in diagnosis. Dr Paul Alan Cox, executive and co-founder of Brain Chemistry Labs, emphasized the urgency, stating, 'For ALS, which typically results in loss of life within 2–5 years from the appearance of symptoms, a delay of one year in receiving a diagnosis is simply unacceptable.' He underscored that 'The ALS patient population is deeply underserved,' which propelled their pursuit of this diagnostic breakthrough.
Earlier and more accurate diagnosis is critical, as it would allow patients to access specialist care, symptom-relieving treatments, and clinical trials much sooner. Though there is currently no cure for MND, these interventions can significantly improve quality of life. Following their successful findings, Dr Sandra Banack announced that the team is now seeking to transition the test beyond the laboratory, actively looking to 'identify a diagnostic firm to make this test commercially available.'
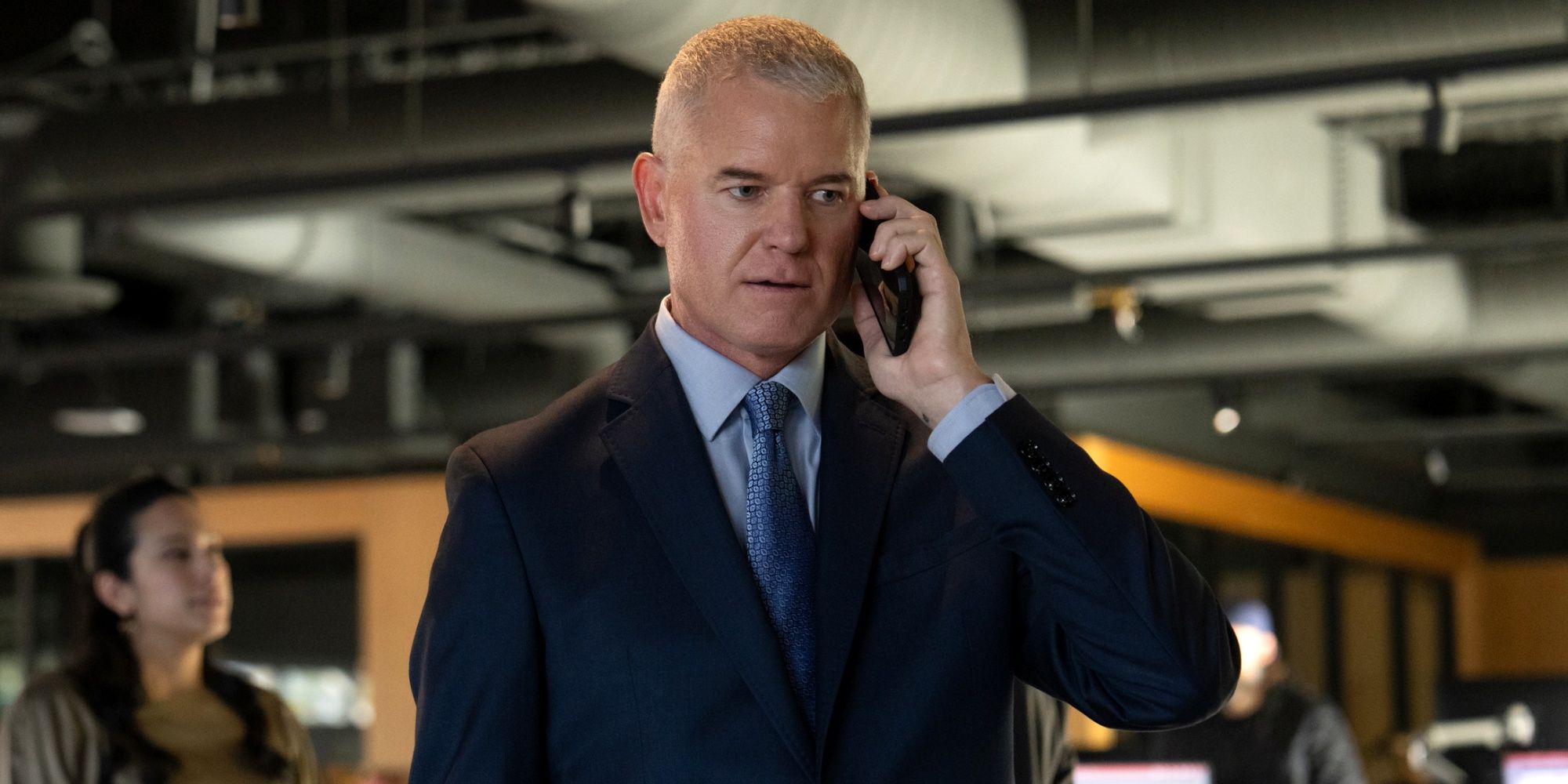
The disease has recently gained increased public attention through several high-profile cases. England rugby legend Lewis Moody revealed his diagnosis at 47 earlier this year. The illness also claimed the life of former rugby league star Rob Burrow, who was diagnosed in 2019 and became a powerful campaigner for enhanced research funding and improved patient care. Actor Eric Dane, known for his role in Grey’s Anatomy, also recently disclosed his diagnosis. Perhaps the most well-known case is that of famed physicist Professor Stephen Hawking, who defied expectations by living with MND for over 40 years after an early-20s diagnosis.
Beyond diagnostics, recent genetic discoveries are also shedding light on the disease's development and pointing towards future treatments. A study published earlier this year identified 423 ultra-rare genetic variants shared by individuals with ALS and those with another motor neurone condition, hereditary spastic paraplegia (HSP). Although these diseases progress differently, their genetic overlap suggests shared biological mechanisms. Dr Gang Wu, a statistician who led this research, noted that rare genetic variants in motor neurone diseases have often been overlooked. He explained, 'By analysing a large dataset with multiple related motor neuron disorders, we found that genes associated with HSP could also increase the risk for sporadic ALS.' These findings hold promise for helping scientists better understand who is at risk of developing ALS and, over time, supporting the development of much-needed new treatments.
You may also like...
Super Eagles Fury! Coach Eric Chelle Slammed Over Shocking $130K Salary Demand!
)
Super Eagles head coach Eric Chelle's demands for a $130,000 monthly salary and extensive benefits have ignited a major ...
Premier League Immortal! James Milner Shatters Appearance Record, Klopp Hails Legend!

Football icon James Milner has surpassed Gareth Barry's Premier League appearance record, making his 654th outing at age...
Starfleet Shockwave: Fans Missed Key Detail in 'Deep Space Nine' Icon's 'Starfleet Academy' Return!

Starfleet Academy's latest episode features the long-awaited return of Jake Sisko, honoring his legendary father, Captai...
Rhaenyra's Destiny: 'House of the Dragon' Hints at Shocking Game of Thrones Finale Twist!

The 'House of the Dragon' Season 3 teaser hints at a dark path for Rhaenyra, suggesting she may descend into madness. He...
Amidah Lateef Unveils Shocking Truth About Nigerian University Hostel Crisis!
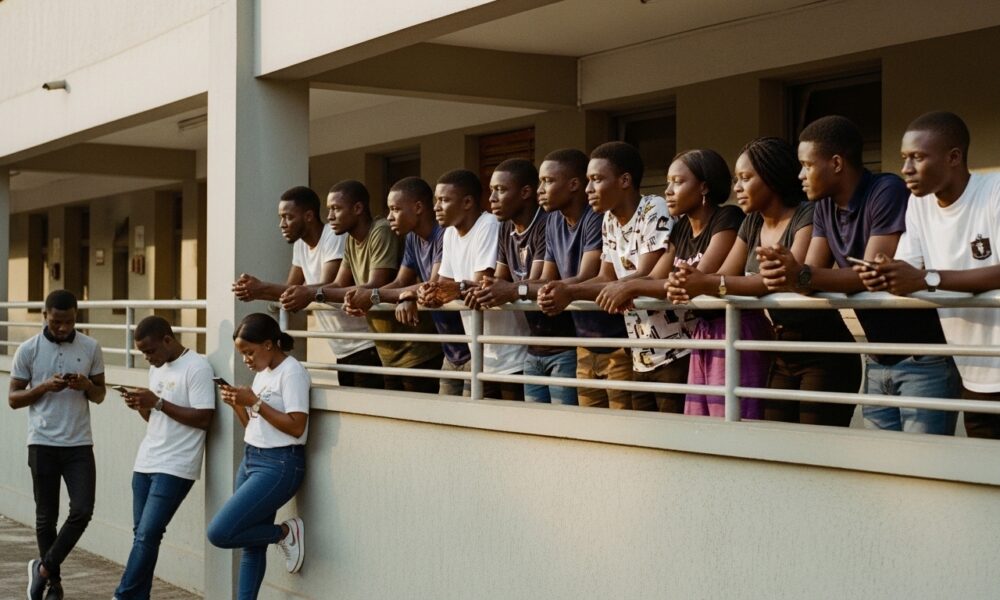
Many university students are forced to live off-campus due to limited hostel spaces, facing daily commutes, financial bu...
African Development Soars: Eswatini Hails Ethiopia's Ambitious Mega Projects

The Kingdom of Eswatini has lauded Ethiopia's significant strides in large-scale development projects, particularly high...
West African Tensions Mount: Ghana Drags Togo to Arbitration Over Maritime Borders

Ghana has initiated international arbitration under UNCLOS to settle its long-standing maritime boundary dispute with To...
Indian AI Arena Ignites: Sarvam Unleashes Indus AI Chat App in Fierce Market Battle

Sarvam, an Indian AI startup, has launched its Indus chat app, powered by its 105-billion-parameter large language model...