Alarming Discovery: Common Blood Type Linked to Higher Risk of Deadly Liver Disease

A recent study has uncovered a significant link between an individual's blood type and their risk of developing autoimmune liver disease, a condition that can lead to severe, life-threatening damage to the liver. The research indicates that people with blood type A may face a heightened risk of autoimmune liver diseases, while those with blood type B appear to have a significantly reduced likelihood of developing primary biliary cholangitis (PBC), a specific type of liver disease that can ultimately result in organ failure.
Blood type is determined by a person's genetic makeup, specifically by the expression of A, B, or H antigens on the surface of red blood cells. Globally, people fall into one of four primary types: A, B, AB, and O, which are further categorized into positive and negative subtypes. In the UK, for instance, nearly half the population has O blood type, over a third has A, and B and AB types account for approximately 10% and 5% respectively.
The study, published in the journal Frontiers in Medicine, involved an analysis of over 1,200 patients, 114 of whom had been diagnosed with autoimmune liver disease. Researchers compared the blood types of these 114 patients with a group of 1,167 healthy individuals. Among the patients with autoimmune liver disease, 44 had autoimmune hepatitis and 70 were diagnosed with PBC. The findings revealed that blood group A was the most common among patients with both forms of chronic liver disease, followed by groups O, B, and AB.
Specifically, when compared to healthy controls, there was a significant difference in blood-type distribution among patients with PBC, although not among those with autoimmune hepatitis. The study distinctly showed that individuals with type B blood were less likely to develop PBC, whereas patients with blood type A were at a significantly higher risk. Dr. Yi Hong, an expert in transfusion medicine at Xi'an Gaoxin Hospital and lead author of the study, noted that people with blood type A were more prone to developing PBC compared to those with blood types AB and O.
Autoimmune liver diseases occur when the body's immune system mistakenly attacks the liver, leading to inflammation and damage. This can eventually cause irreversible scarring, known as cirrhosis, and ultimately liver failure. There are several types of these chronic conditions, including autoimmune hepatitis, where the immune system directly attacks liver cells, and PBC, where it targets the liver's bile ducts, causing bile to accumulate and leading to scarring, cirrhosis, and liver failure. Symptoms for these conditions can be vague or non-existent in early stages, often including fatigue, bone and joint aches, itchy skin, dry eyes and mouth, or abdominal pain, and may only be detected through routine blood tests for other reasons.
The researchers theorize that individuals with type A blood might carry more high-risk antigens for autoimmune liver disease due to a process called linkage disequilibrium. Previous studies have indicated that type A individuals are more likely to carry specific alleles, such as HLA-DRB1*03:01 and DRB1*04:01, which have been associated with autoimmune liver disease. These genes play a vital role in the immune system's ability to distinguish between the body's own cells and foreign invaders. While these mechanisms were not directly tested in the current study, they offer a plausible explanation for the observed link.
Beyond blood type, the study also identified other factors influencing susceptibility. Females were found to be more susceptible to autoimmune liver disease than males, a gender difference that could be attributed to sex hormones, fetal micro-chimerism, and genetic factors. Furthermore, the incidence of these diseases was observed to increase with age. Given these findings, the researchers concluded that their study supports the integration of blood type analysis in clinical settings as a tool to identify patients who may be at an elevated risk of autoimmune liver disease, particularly PBC.
Diagnosis of autoimmune liver disease often occurs at a stage when about a third of sufferers already have significant cirrhosis. Early symptoms like fatigue are frequently dismissed, leading to delays in seeking medical help. Current treatments include immune-system and inflammation-dampening steroids, which must be taken for life and carry side effects such as diarrhea, abdominal pain, and skin reactions. In some cases, these drugs can even worsen liver cirrhosis, potentially leading to rapid liver failure within days or weeks, with the only curative option being a liver transplant. However, the demand for liver transplants far exceeds the available supply. Experts caution that both primary biliary cholangitis and autoimmune hepatitis are on the rise, though the exact reasons remain unclear, with viral infections and environmental toxins suggested as potential triggers.
You may also like...
Super Eagles Fury! Coach Eric Chelle Slammed Over Shocking $130K Salary Demand!
)
Super Eagles head coach Eric Chelle's demands for a $130,000 monthly salary and extensive benefits have ignited a major ...
Premier League Immortal! James Milner Shatters Appearance Record, Klopp Hails Legend!

Football icon James Milner has surpassed Gareth Barry's Premier League appearance record, making his 654th outing at age...
Starfleet Shockwave: Fans Missed Key Detail in 'Deep Space Nine' Icon's 'Starfleet Academy' Return!

Starfleet Academy's latest episode features the long-awaited return of Jake Sisko, honoring his legendary father, Captai...
Rhaenyra's Destiny: 'House of the Dragon' Hints at Shocking Game of Thrones Finale Twist!

The 'House of the Dragon' Season 3 teaser hints at a dark path for Rhaenyra, suggesting she may descend into madness. He...
Amidah Lateef Unveils Shocking Truth About Nigerian University Hostel Crisis!
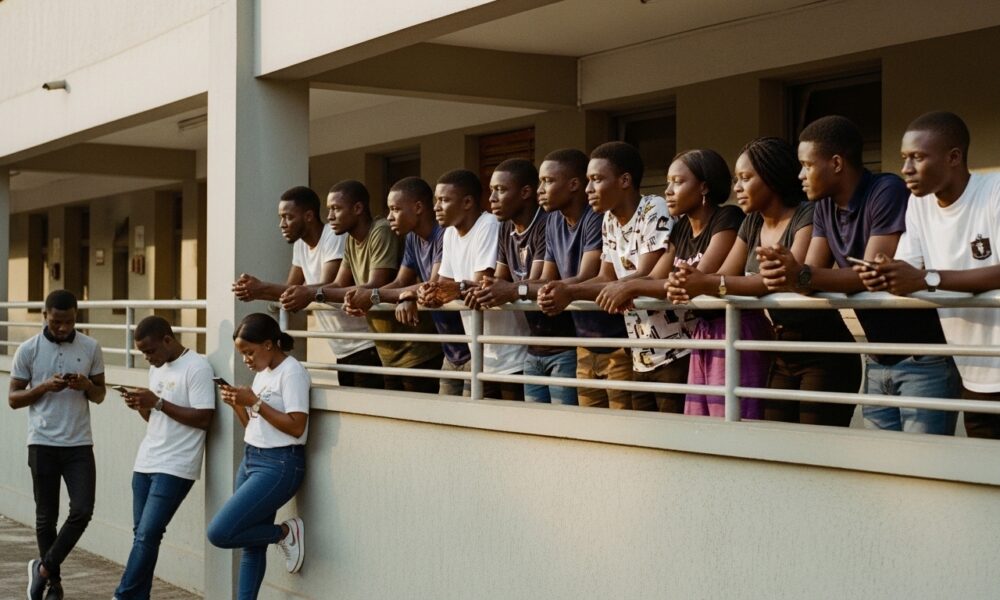
Many university students are forced to live off-campus due to limited hostel spaces, facing daily commutes, financial bu...
African Development Soars: Eswatini Hails Ethiopia's Ambitious Mega Projects

The Kingdom of Eswatini has lauded Ethiopia's significant strides in large-scale development projects, particularly high...
West African Tensions Mount: Ghana Drags Togo to Arbitration Over Maritime Borders

Ghana has initiated international arbitration under UNCLOS to settle its long-standing maritime boundary dispute with To...
Indian AI Arena Ignites: Sarvam Unleashes Indus AI Chat App in Fierce Market Battle

Sarvam, an Indian AI startup, has launched its Indus chat app, powered by its 105-billion-parameter large language model...