Africa's Silent Killer: Unmasking the Looming Non-Communicable Disease Crisis
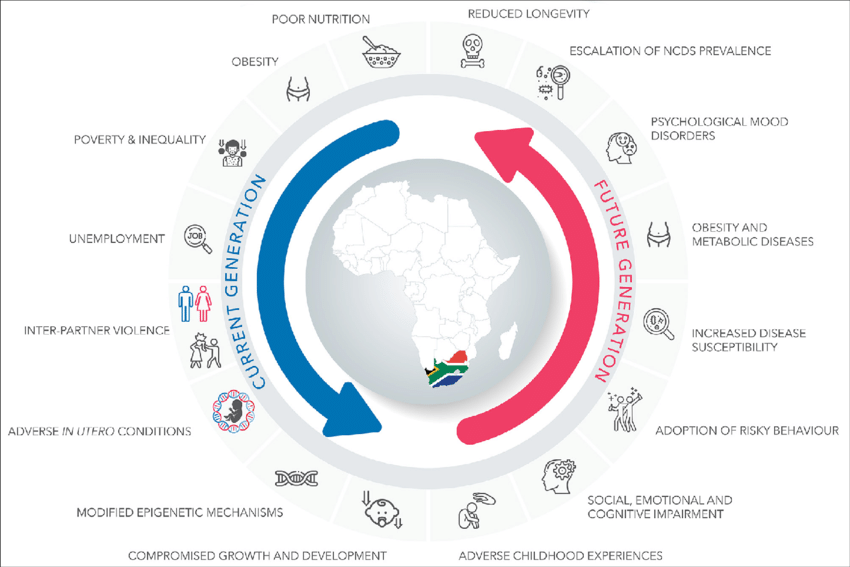
While the world often associates Africa's health challenges primarily with infectious diseases like malaria, HIV, or tuberculosis, a far more insidious and rapidly escalating threat is taking hold: Non-Communicable Diseases (NCDs) such as hypertension, diabetes, cancer, and chronic respiratory illnesses.
SOURCE: Google
This article will expose how changing lifestyles, rapid urbanization, shifts in diet, and increasing longevity are fueling an NCD epidemic that is quietly overwhelming healthcare systems and imposing immense economic burdens on families and nations.
We'll delve into the social determinants of these diseases, the unique challenges of prevention and treatment in resource-limited settings, and the urgent need for a paradigm shift in public health approaches.
The Rising Tide: Drivers of Africa's NCD Surge
The rapid increase in NCDs across various African countries is driven by a confluence of socio-economic changes, rapid urbanization, and profound lifestyle shifts, creating a perfect storm for this silent epidemic.
Rapid urbanization is a primary catalyst. As millions migrate from rural areas to burgeoning cities in search of economic opportunities, they often encounter environments conducive to NCDs.
Urban centers typically involve more sedentary occupations, increased exposure to processed foods, and higher levels of air pollution.
The shift from active, agrarian lifestyles to more passive, urban ones directly contributes to a rise in obesity and physical inactivity, key risk factors for diabetes and cardiovascular diseases.
Reports from theWorld Health Organization (WHO) highlight that NCDs are projected to become the leading cause of death in Africa by 2030, partly due to these demographic shifts.
Changing dietary patterns play a significant role. Traditional African diets, often rich in whole grains, fruits, and vegetables, are increasingly being replaced by Westernized diets characterized by high consumption of processed foods, sugary drinks, refined carbohydrates, and unhealthy fats.
These readily available, often cheaper, and aggressively marketed convenience foods contribute to a rise in hypertension, type 2 diabetes, and obesity. For instance, countries like South Africa have seen a dramatic increase in fast-food consumption, directly correlating with a rise in diet-related NCDs.
Lifestyle shifts beyond diet and physical activity also contribute. There's an alarming increase in tobacco use, especially among young people, and harmful alcohol consumption across many African nations.
Both are major risk factors for various cancers, chronic respiratory diseases, and cardiovascular conditions. Furthermore, longer life expectancies, a positive indicator of development, mean more people are living into ages where NCDs typically manifest, increasing the overall burden on the population.
The "double burden of disease," where countries grapple with both persistent infectious diseases and a burgeoning NCD crisis, is a defining feature of Africa's current health landscape.
Strained Systems: Healthcare's NCD Challenge
Africa's already strained healthcare systems are struggling immensely to adapt to the long-term management and specialized care required for NCDs, often prioritizing acute infectious diseases due to historical funding and training biases.
SOURCE: Google
A significant challenge is the lack of infrastructure and specialized personnel. NCDs require continuous care, regular monitoring, and often specialized equipment.
Many public health facilities in Africa, particularly in rural and even peri-urban areas, lack these essential resources.
There's also a severe shortage of trained specialists – cardiologists, endocrinologists, oncologists, and mental health professionals – compounding the difficulty of providing adequate NCD care.
Patients often have to travel long distances to access limited specialized centers, incurring significant travel and accommodation costs, or simply go without care.
Prioritization of infectious diseases has historically shaped healthcare funding and training.
For decades, global health initiatives and domestic budgets rightly focused on combating prevalent infectious diseases like HIV/AIDS, malaria, and tuberculosis. While crucial, this has inadvertently led to an underinvestment in NCD prevention and management.
Healthcare workers are often trained more extensively in acute care and infectious disease protocols, leaving them ill-equipped for the chronic, multi-faceted nature of NCDs, which require patient education, lifestyle counseling, and long-term follow-up.
The financial burden on patients and systems is immense. NCDs require lifelong medication, frequent doctor visits, and sometimes costly procedures. In health systems where out-of-pocket payments are common, this leads to catastrophic health expenditures, pushing families into poverty.
Even for those with health insurance, coverage might be limited. Governments, already managing competing health priorities, find it difficult to allocate sufficient budgets for expensive NCD medications and long-term care programs, exacerbating the problem.
The World Health Organization estimates that NCDs could cost African countries billions of dollars in lost GDP due to premature deaths and disability.
This financial strain impacts not just individual families but also national productivity and economic development.
Innovation and Intervention: A Path Forward
Despite the immense challenges, innovative, community-based, and policy-level interventions are showing promise in preventing, detecting, and managing NCDs in the African context, but urgent steps are needed to scale them effectively.
SOURCE: Forbes
Community-based screening and awareness programs are crucial. Leveraging existing community health worker (CHW) networks can dramatically improve early detection of NCDs like hypertension and diabetes.
CHWs, trained to measure blood pressure, conduct basic glucose tests, and provide health education, can reach populations in remote areas who have limited access to formal healthcare.
Initiatives like the "Healthy Heart Africa" program have demonstrated success in training healthcare workers and raising public awareness about hypertension and diabetes across several African countries.
Integrating NCD screening into routine visits for other health services, such as antenatal care or HIV clinics, also offers a cost-effective way to reach more people.
Low-cost digital health solutions (mHealth) are also proving effective. Mobile phone-based interventions can support NCD management through medication reminders, health education messages, appointment alerts, and even remote consultations. SMS programs can encourage adherence to treatment and healthy lifestyles.
For instance, in Ghana, mobile health applications have been used to support diabetes management, improving patient engagement and self-care.
Telemedicine can connect patients in remote areas with specialists in urban centers, bridging geographical gaps in expertise.
At the policy level, robust interventions are urgently needed.
This includes implementing "sin taxes" on tobacco, alcohol, and sugary drinks to discourage consumption and generate revenue for NCD programs. Strict regulations on food labeling and marketing, especially to children, can promote healthier dietary choices.
Governments must also invest in creating environments that encourage physical activity, such as safe walking paths and public green spaces in urban areas.
Strengthening primary healthcare systems to manage NCDs at the foundational level, rather than relying solely on specialized hospitals, is paramount.
This includes training general practitioners and nurses in NCD management, ensuring consistent supplies of essential NCD medicines, and developing robust referral systems.
Ultimately, scaling these interventions requires a paradigm shift in funding and political will. International donors and national governments must recognize NCDs as a top public health priority, allocating dedicated resources for prevention, early detection, and long-term care.
Investing in health promotion, strengthening primary care, and leveraging community assets are urgent steps needed to transform Africa's health trajectory, turning the tide against this silent, yet devastating, NCD crisis.
You may also like...
When Sacred Calendars Align: What a Rare Religious Overlap Can Teach Us

As Lent, Ramadan, and the Lunar calendar converge in February 2026, this short piece explores religious tolerance, commu...
Arsenal Under Fire: Arteta Defiantly Rejects 'Bottlers' Label Amid Title Race Nerves!

Mikel Arteta vehemently denies accusations of Arsenal being "bottlers" following a stumble against Wolves, which handed ...
Sensational Transfer Buzz: Casemiro Linked with Messi or Ronaldo Reunion Post-Man Utd Exit!

The latest transfer window sees major shifts as Manchester United's Casemiro draws interest from Inter Miami and Al Nass...
WBD Deal Heats Up: Netflix Co-CEO Fights for Takeover Amid DOJ Approval Claims!

Netflix co-CEO Ted Sarandos is vigorously advocating for the company's $83 billion acquisition of Warner Bros. Discovery...
KPop Demon Hunters' Stars and Songwriters Celebrate Lunar New Year Success!

Brooks Brothers and Gold House celebrated Lunar New Year with a celebrity-filled dinner in Beverly Hills, featuring rema...
Life-Saving Breakthrough: New US-Backed HIV Injection to Reach Thousands in Zimbabwe

The United States is backing a new twice-yearly HIV prevention injection, lenacapavir (LEN), for 271,000 people in Zimba...
OpenAI's Moral Crossroads: Nearly Tipped Off Police About School Shooter Threat Months Ago
ChatGPT-maker OpenAI disclosed it had identified Jesse Van Rootselaar's account for violent activities last year, prior ...
MTN Nigeria's Market Soars: Stock Hits Record High Post $6.2B Deal

MTN Nigeria's shares surged to a record high following MTN Group's $6.2 billion acquisition of IHS Towers. This strategi...

