A New Dawn for Global Mental Health: Innovations Breaking Through the Crisis

Technological innovations are at the forefront of this revolution, directly addressing some of the most significant barriers to care, particularly the shortage of qualified professionals and the lack of accessible services in remote areas.
SOURCE: Google
Telemedicine and teletherapy platforms have made mental health support available on-demand, allowing individuals to connect with licensed therapists via video, phone, or text, regardless of their location.
This has proven particularly impactful in rural and underserved regions, where access to in-person clinics is often non-existent, and a study by the American Psychological Associationfound that telehealth services are just as effective as traditional therapy for many conditions.
Beyond simple connectivity, AI-driven diagnostics and digital phenotyping are revolutionizing early detection.
AI can analyze data from a person's smartphone use, like their speech patterns, tone of voice, or social media activity, to identify subtle behavioral markers of depression and anxiety with impressive accuracy, often before a person is even aware of their symptoms, as noted in research published in Nature Medicine.
This capability supports early intervention, allowing for timely treatment that can prevent conditions from escalating.
Furthermore, VR (Virtual Reality) therapies are being used for exposure therapy in a controlled environment, helping patients with phobias and PTSD to confront their fears safely and effectively.
The gamification of treatment, seen in products like EndeavorRX for ADHD, is also making therapy more engaging and accessible for younger people, as highlighted by a report from the Pew Research Center.
The Power of Destigmatization and Public Awareness
SOURCE: Google
Global destigmatization campaigns and increased public awareness are having a measurable impact on help-seeking behaviors.
As mental health conversations become more normalized in media, workplaces, and daily life, the shame and fear associated with seeking help are diminishing.
Data from a study by the National Alliance on Mental Illness (NAMI) shows that improved public attitudes towards help-seeking have led to a greater willingness to seek professional care, especially among younger generations.
These campaigns often employ strategies like sharing personal stories, which helps to humanize mental illness and foster empathy and understanding.
This shift has created a virtuous cycle: as more people feel comfortable discussing their mental health, the issue gains more visibility, which in turn encourages more support and resources.
This public dialogue is also a key driver of policy change, as governments and corporations recognize the widespread nature of the problem and the economic imperative of addressing it.
A 2022World Health Organization (WHO) report noted that public awareness campaigns are a critical first step in shifting mental health from a private struggle into a collective public health priority, as they directly lead to increased political will and funding.
Policy and Funding as Drivers of Change
Policy reforms, increased funding, and international guidance from organizations like the WHO are driving the integration of mental health into primary care systems.
Historically, mental and physical health have been treated as separate entities, leading to fragmented and incomplete care.
The WHO's Comprehensive Mental Health Action Plan 2013–2030 and its mhGAP program are championing a new model where mental health services are provided at the community level by trained non-specialist health workers.
This "task-shifting" approach is critical for addressing the severe shortage of mental health professionals globally, a problem detailed in a recent Lancet Commission report.
Furthermore, governments are beginning to legislate for parity between physical and mental healthcare, ensuring that mental health conditions are covered equally by insurance and public health programs.
This financial commitment is key to creating a sustainable and equitable system. The move towards holistic, person-centered care models acknowledges the interconnectedness of physical and mental well-being, promoting a more comprehensive approach to health that treats the whole person, not just their symptoms.
In the United Kingdom, for example, the NHS Long Term Plan has committed significant new funding to expand mental health services and integrate them more closely with physical healthcare, demonstrating a clear policy shift.
Community-Led and Culturally Sensitive Interventions
In many underserved regions, community-led and culturally sensitive interventions are proving to be the most effective way to bridge treatment gaps.
SOURCE: Google
These programs leverage existing local resources and social structures, such as community leaders, barbers, or faith-based organizations, to deliver mental health support in a way that is trusted and culturally resonant.
For example, the Confess Project in the US trains barbers as mental health advocates, providing support in a non-traditional, comfortable setting.
A study on mental health services in Sub-Saharan Africa found that community-based approaches are far more effective at reaching rural populations than centralized, clinic-based models.
These interventions are powerful because they bypass the systemic barriers of traditional healthcare, including stigma and geographical inaccessibility.
By adapting psychotherapies to reflect local cultural norms and values, they enhance patient engagement and improve outcomes, as noted in a review published in the Journal of Community Psychology.
This approach empowers communities to take ownership of their well-being, proving that effective mental healthcare doesn't always require a clinic.
The United Nations has also highlighted the importance of incorporating indigenous healing practices and traditional knowledge into modern mental health frameworks to better serve diverse populations.
Accelerating Progress Through Public-Private Partnerships
Public-private partnerships and new investment models are accelerating the development and scaling of accessible mental health solutions.
Governments are collaborating with private tech companies, non-profits, and venture capital firms to create innovative platforms and services that would be difficult for the public sector to develop alone.
The private sector brings efficiency, innovation, and capital, while the public sector provides regulatory oversight, public health expertise, and reach.
These partnerships can lead to scalable solutions, such as digital platforms for remote therapy, that can be implemented rapidly and widely.
They also allow for the sharing of risk and resources, ensuring that promising innovations can move from research to reality much faster.
The surge in Venture Capital (VC) investment in mental health technology—with billions invested annually—underscores the market's recognition of the urgent need for new solutions.
This collaborative approach is essential to tackling a crisis of this magnitude, as no single sector has the capacity to solve it alone.
The World Bank has also begun investing in mental health initiatives in low-income countries, recognizing its critical role in economic development.
Challenges and Ethical Considerations on the Horizon
Despite this progress, significant challenges and ethical considerations remain. A key challenge is ensuring equitable access to technology.
The "digital divide" means that many low-resource communities lack the reliable internet access and devices needed to use digital mental health solutions.
This risks creating a new form of inequality where only those with resources can benefit from the innovations.
This is a problem a Brookings Institution report has identified as a major obstacle to global health equity.
There are also pressing ethical concerns related to data privacy and algorithmic bias in AI-driven diagnostics.
The personal nature of mental health data requires stringent security protocols to protect patient information from misuse. Furthermore, if AI models are trained on biased data sets, they could disproportionately misdiagnose or mismanage care for marginalized communities.
This issue has been raised by organizations like Human Rights Watch. To ensure sustainable progress, the mental health community must address these issues head-on, prioritizing transparency, accountability, and a commitment to ensuring that a brighter future for mental health is a reality for everyone, not just a privileged few.
You may also like...
From Etisalat to 9mobile to T2: The Rise, Retreat, and Reinvention of Nigeria’s Fourth Operator
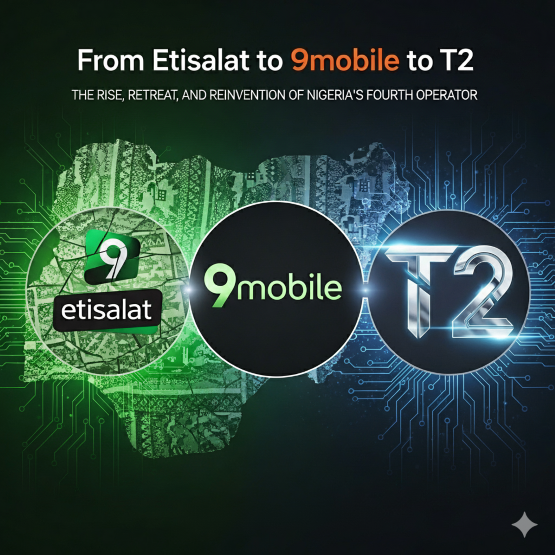
From a meteoric rise to a challenging retreat, Etisalat Nigeria’s evolution into T2 tells a story of resilience, wins, a...
Boxing Blockbuster: Jake Paul and Gervonta Davis Set for November Showdown

In a surprising announcement, Jake Paul is set to face WBA lightweight champion Gervonta "Tank" Davis in an exhibition b...
Carabao Cup Shocker: Grimsby Stuns Man Utd in Penalty Thriller

Manchester United suffered a shocking Carabao Cup exit after losing 12-11 on penalties to League Two side Grimsby Town. ...
Venice Stunner: Paolo Sorrentino's 'La Grazia' Captivates Critics with Record-Breaking Ovation!

Paolo Sorrentino's new film “La Grazia” opened the Venice Film Festival to critical acclaim, presenting a nuanced portra...
The Hunt for 007: Frontrunners Out, Legends Back, New Details Emerge in Bond Saga!

The search for the next James Bond intensifies as actors like Taron Egerton and Glen Powell rule themselves out, while M...
Reading and Leeds Festival Plunged Into Chaos by Secret Set Leaks and Star's Last-Minute Snub

Reading and Leeds Festival 2025 is buzzing with fan speculation about secret sets from The Foo Fighters and Chase & Stat...
Naira Marley Breaks Silence on Mohbad's Death Amid Mounting Controversy

Musician Naira Marley has publicly addressed the controversial death of his former signee, Mohbad, sharing his side of t...
Pete Davidson's Paternal Bliss: Comedian's Dream of Fatherhood Comes True with Elsie Hewitt

Comedian Pete Davidson and model Elsie Hewitt are expecting their first child, announced via Instagram by Hewitt. Davids...