Reliability and validity of the short quality of life scale among bank employees in Guangxi, China
The World Health Organization defines quality of life as an individual’s subjective evaluation of their position in the cultural and value system, as well as their relationships with their goals, expectations, standards, and concerns (WHOQOL, 1993). Within various demographic groups and across diverse cultural milieus, the quality of life plays a significant role in shaping suicidal ideation and behaviors have been reported by researches (He et al., 2020). Health-related quality of life is affected by psychological issues such as depression and suicidal ideation which has been shown significantly in stroke patients in the United States (Chen et al., 2024). In Nigeria, suicidal behavior among HIV-infected individuals is strongly associated with a diminished quality of life (Oladeji et al., 2017). Similarly, a clear link between decreased quality of life and suicidal ideation have been identified by the study in a Australian general community (Goldney et al., 2001). These findings underscore the close relationship between quality of life and suicidal ideation. Therefore, this study groups participants based on the presence or absence of suicidal ideation to more accurately assess quality of life across different psychological states. Assessing quality of life provides a comprehensive understanding of an individual’s physical, psychological, and social well-being, which are closely linked to suicidal ideation (Ki et al., 2024). The quality of life scale serves as an effective tool for identifying individuals experiencing a diminished quality of life, who may be at risk for mental health issues and potentially suicidal ideation or behaviors (Chen et al., 2024). This allows for early detection and targeted intervention to address underlying issues such as depression, loneliness, and hopelessness, thereby reducing the likelihood of suicidal behavior.
The Guangxi region in China, situated in the multi-ethnic and less developed western part of the country. In recent years, banking professionals have been experiencing significant psychological stress because of the pressures associated with digital transformation and other factors (Li, 2022). A study reported that the prevalence of suicidal ideation among bank employees in Guangxi was 7.5%, with major depression, hopelessness, and negative coping styles identified as significant risk factors (He et al., 2020).
The quality of life of Chinese bank employees is influenced by multiple factors and exhibits significant regional disparities. Work-life imbalance is a critical factor contributing to the decline in their quality of life. Long hours in confined environments and strict performance evaluations, which are typical of the banking profession, severely disrupt the work-life balance of bank employees. Research has demonstrated a significant positive correlation between work-life balance and job satisfaction in the Shanghai region (Xue et al., 2024). Due to factors such as fewer bank branches, employees in county and rural areas are more susceptible to work-life imbalance, leading to a decline in their quality of life (Li and Liu, 2021). Environmental factors, particularly the work environment, have a substantial impact on the quality of life of bank employees (Gür et al., 2016). Furthermore, grassroots bank employees in different altitude regions show varying probabilities of abnormal results in physical examinations, which further affect their quality of life (Wang and Zhao, 2008). These disparities suggest that improving the quality of life of Chinese bank employees requires tailored strategies and a comprehensive consideration of various factors. Nonetheless, research on the quality of life of bank employees remains limited, especially regarding the validation of relevant assessment tools.
Various measurement tools provide quantitative bases for assessing the quality of life of bank employees. WRQoL scale focuses on work-related aspects of life quality, accurately capturing employees’ quality of life within their work environment (Geçkil, 2021). The Quality of Work Life Scale measures multiple dimensions, including job satisfaction, overall well-being, and work stress (Tentama and Suwandi, 2020). The scale was evaluated using structural equation modeling, which demonstrated that its dimensions and indicators effectively captured the construction of work life quality with high validity. In the empirical analysis of bank employees’ quality of life, Cronbach’s α was employed to assess the reliability of the model, and the results indicated a satisfactory level of reliability. Although various quality of life scales, including QOLS (Burckhardt and Anderson, 2003), WHOQOL-BREF (Makovski et al., 2019), CASP-11-SG (Tan et al., 2023), CQ-11D (Zhou et al., 2024) and ProQOL (Galiana et al., 2020), each has certain limitations. The WHOQOL-BREF demonstrates strong cross-cultural validity but requires lengthy administration time, while the QOLS, CASP-11-SG and CQ-11D face challenges in cultural adaptation within Chinese contexts. ProQOL, while effective in assessing professional burnout, has a narrower focus. Given these limitations, we selected the QOLS-6 scale and conducted targeted validation to better suit the specific population of this study.
This study used the 6-item short form Quality of Life Scale (QOLS-6) developed by Phillips (Phillips et al., 2002). The QOLS-6 was showed good reliability and validity in a psychological analysis of the general Chinese population in 2002. The scale focuses on six dimensions of quality of life over the preceding 30 days, including physical well-being, psychological health, economic status, occupational satisfaction, family relationships, and social interactions. The QOLS-6 has been validated in a study of psychological autopsy of elderly individuals who died by suicide in rural China, demonstrating its reliability and effectiveness within this population (He et al., 2021). Currently, the QOLS-6 has demonstrated strong psychometric properties primarily among rural elderly populations in China, highlighting its potential for broader applicability. The scale features a concise structure with only six items, enhancing its practicality for large-scale assessments.
To the best of our knowledge, QOLS-6 was used for the first time in research among the bank employees. This study evaluates the applicability of the QOLS-6 within bank employees in Guangxi, providing a foundation for future research to validate its generalizability across diverse occupational and regional groups. By demonstrating its reliability and validity, the study proposes the QOLS-6 as a practical tool for assessing quality of life in mental health research contexts. The following research hypotheses are proposed:
H1: Based on the theoretical framework of quality of life and the design of the scale’s content, three latent factors can be extracted from the quality of life scale in the bank employee population.
H2: The quality of life scale demonstrates good reliability in the bank employee population.
H3: The quality of life scale demonstrates good validity in the bank employee population.
In this study, a cross-sectional survey and cluster sampling method were adopted to conduct an online questionnaire survey among 5,000 employees of a bank in Guangxi from November to December 2019. Guangxi is an underdeveloped region in western China. The research sample covers several prefecture-level cities such as Nanning, Liuzhou, Guilin and Guigang. The work institutions involved include first and second-level branches and first and second-level sub-branches of banks, and the work institution levels involved cover both the front desk and middle and back offices of banks. The researchers sent each respondent a survey link via an electronic questionnaire and briefly introduced the study. The participants signed informed consent, and their identities remained anonymous prior to the commencement of the study. To prevent data loss and redundant responses, it was necessary for each respondent to complete all questions and submitted their response only once. Meanwhile, the survey included an automated logic verification feature to guarantee the integrity of responses. After the survey was completed, the data was double-checked, cleaned, and reviewed, resulting in the collection of 3,974 valid questionnaires, including 298 employees in the suicidal ideation group and 3,676 employees in the non-suicidal ideation group. This study was approved by the Medical Ethics Committee of Guangxi Medical University (Ethical Application Ref: KY20240151).
Demographics
The collected demographic data includes sex, age, educational level (Associate Degree or below, Bachelor’s Degree, Master’s Degree or above), marital status (Single, Married, or Other), and years of working experience (≤3 years, 4–12 years, over 12 years). “Other” marital statuses include separation, divorce, and widowhood. The age grouping is based on the sample’s median age of 35 years. Work experience groups are defined according to the requirement in China for new employees to sign a labor contract of at least three years at the beginning of their employment, combined with the division of career stages into early, mid, and late phases.
Quality of life scale (QOLS-6)
The QOLS-6 developed by Phillips (Phillips et al., 2002) assesses the respondent’s quality of life in six dimensions over the preceding month: physical, psychological, economic, occupational, familial relationships, and social interactions. Participants rated each item on a 5-point Likert scale (1 = very poor, 5 = excellent), with total scores ranging from 6 to 30. A higher total score indicates a better quality of life.
Suicidal ideation and self-harming actions
The presence of suicidal ideation within the past year is assessed by asking the question “Have you seriously considered ending your own life within the past year?” (Wang, 2019). In addition, self-harming actions were evaluated with the question: “At any point in the past, have you taken any self-harming actions?” Participants responded with either “Yes” or “No.”
Maslach burnout inventory-general survey (MBI-GS)
The scale measures three dimensions of emotional exhaustion, depersonalization, and diminished professional accomplishment. This is a self-report questionnaire with 15 items, rating on a 7-point scale (0 = never to 6 = each day). The higher the total score on the scale, the higher the level of job burnout (Li and Shi, 2003). The scale demonstrated good internal consistency, with a Cronbach’s α coefficient of 0.884.
Job satisfaction scale
The scale consists of six items, including satisfaction with promotion opportunities, colleagues, superiors, the job itself, income, and overall satisfaction. The answers can be given using a 5-point Likert Scale (1 = very dissatisfied to 5 = very satisfied). The higher the total score of the scale, the more satisfied the job (Schriesheim and Tsui, 1980). The Cronbach’s α for the scale was 0.865, indicating satisfactory reliability.
Patient health questionnaire (PHQ-9)
PHQ-9 consists of nine depressive symptoms items that evaluate the state of the past two weeks, including both emotional (Items 1, 2, 4, 6, 8, 9) and physical (Items 3, 5, 7) dimensions. The specific items include “Over the past two weeks, how often have you felt little interest or pleasure in doing things?,” etc. The answers can be given using a 4-point Likert Scale ranging from none to every day. The total score of the scale is 27 points, The higher total score indicating more severe depressive symptoms (Spitzer et al., 1999). In the study, the Cronbach’s α for the scale was 0.918.
Chinese revision of short-form of the UCLA loneliness scale (ULSA-6)
Consisting of 6 items, it uses a 4-point Likert Scale (1 = never, 5 = always). The specific items include “Lack of company from others,” “No one to turn to for help,” “I feel neglected,” etc. The total score of the scale ranges from 6 to 24 points, with higher scores indicating a stronger sense of loneliness (Zhou et al., 2012). The Cronbach’s α for the scale was 0.913.
Beck hopeless scale (BHS)
The BHS evaluates an individual’s mental state over the previous week, comprising four items rated on a 5-point Likert Scale from completely agree to completely disagreement. The specific items include, “I hope that in the future I can do the most important things well.,” “My future is dark.,” “I’m just unlucky and I’ll always be.” and “I am full of confidence about the future.” The total score ranges from 4 to 20, with higher scores indicating a greater sense of hopelessness (Beck et al., 1974). The Cronbach’s α for the scale was 0.797.
Affection and resolve scale (family APGAR)
The study utilized the Family APGAR Questionnaire developed by Smilkstein (1978), which evaluates family functionality across five dimensions: Adaptation, Partnership, Growth, Affection, and Resolve. The questionnaire employs a 3-point reverse scoring system, with responses of “often,” “sometimes,” and “rarely” scored as 2, 1, and 0 points, respectively. The total score ranges from 0 to 10, with higher scores indicating better family functionality. The Cronbach’s α for the scale was 0.874.
Categorical variables were expressed as count and percentage, while continuous variables were expressed as mean ± standard deviation (Means ± SD). Descriptive analysis, chi-square test, independent sample t-test and Mann–Whitney test were employed to compare demographic characteristics between the groups.
Reliability was assessed using Cronbach’s α coefficient, where values between 0.70 and 0.79 were deemed acceptable, 0.80 to 0.89 as good, and ≥ 0.90 as excellent (van Krugten et al., 2022). Corrected item-total score correlations were also calculated, with coefficients≥0.40 considered indicative of acceptable item consistency within the overall scale.
To ensure the robustness of the factor structure, the non-suicidal ideation group (N = 3,676) was randomly split into two subsamples: Subsample A (n = 1,838) for EFA and Subsample B (n = 1,838) for CFA. The structural validity of QOLS-6 was assessed through exploratory factor analysis (EFA). The suitability of EFA was confirmed by the Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy and Bartlett’s test of sphericity, where KMO values >0.600 and p < 0.05 indicated adequacy (Ma et al., 2020). EFA was conducted using principal components extraction and varimax rotation, with factors identified based on eigenvalues >1 and the scree plot. A factor loading cut-off of ≥0.40 was applied to retain items contributing significantly to the factor structure. To ensure the accuracy of the results, a parallel analysis using Monte Carlo simulation was conducted, generating a series of data sets that simulate the experimental data. If the eigenvalues of the factors from the experimental data set are larger than those for the simulated data set, then it can be concluded that the respective factors are present in the data set (Sanatkar and Rubin, 2023). Confirmatory factor analysis (CFA) was used to evaluate the construct validity. Using chi-square test, root mean square error of approximation (RMSEA; values<0.08 are acceptable, ≤0.05 are ideal), standardized root mean square residual (SRMR; values ≤0.05 suggest a good fit), Bentler Comparative Fit Index (CFI), and Bentler Bonett normed fit index (NFI) (CFI and NFI values >0.90 suggest adequate fit) (Sun et al., 2019). For concurrent validity, Spearman correlation was used, with correlation coefficients below 0.2 considered absent, 0.2 to <0.35 as weak, 0.35 to <0.50 as moderate, and ≥ 0.50 as very strong (Haspels et al., 2023). Statistical analyses were performed using SPSS 27.0, Amos 26.0 and Mplus 8.3 software, and a two-tailed p-value of <0.05 was considered statistically significant.
Demographics
Among the 3,974 survey participants, there were 1,195 males (30.1%) and 2,779 females (69.9%). Among them, 298 (7.5%) reported suicidal ideation, as a suicidal ideation group, 3,676 (92.5%) of non-suicidal ideation workers as a non-suicidal ideation group. As shown in Table 1, it is evident that the prevalence of suicidal ideation is significantly higher among individuals aged ≤35 years (p = 0.001), and with 4–12 years of work experience (p = 0.038). The prevalence of self-harming actions was found to be higher among participants with suicidal ideation (p < 0.001). The scores of depression, hopelessness, loneliness, and job burnout in the group with suicidal ideation were significantly higher than those in the non-suicidal ideation group (p < 0.001), while their scores of job satisfaction and family function were significantly lower than those in the non-suicidal ideation group (p < 0.001).
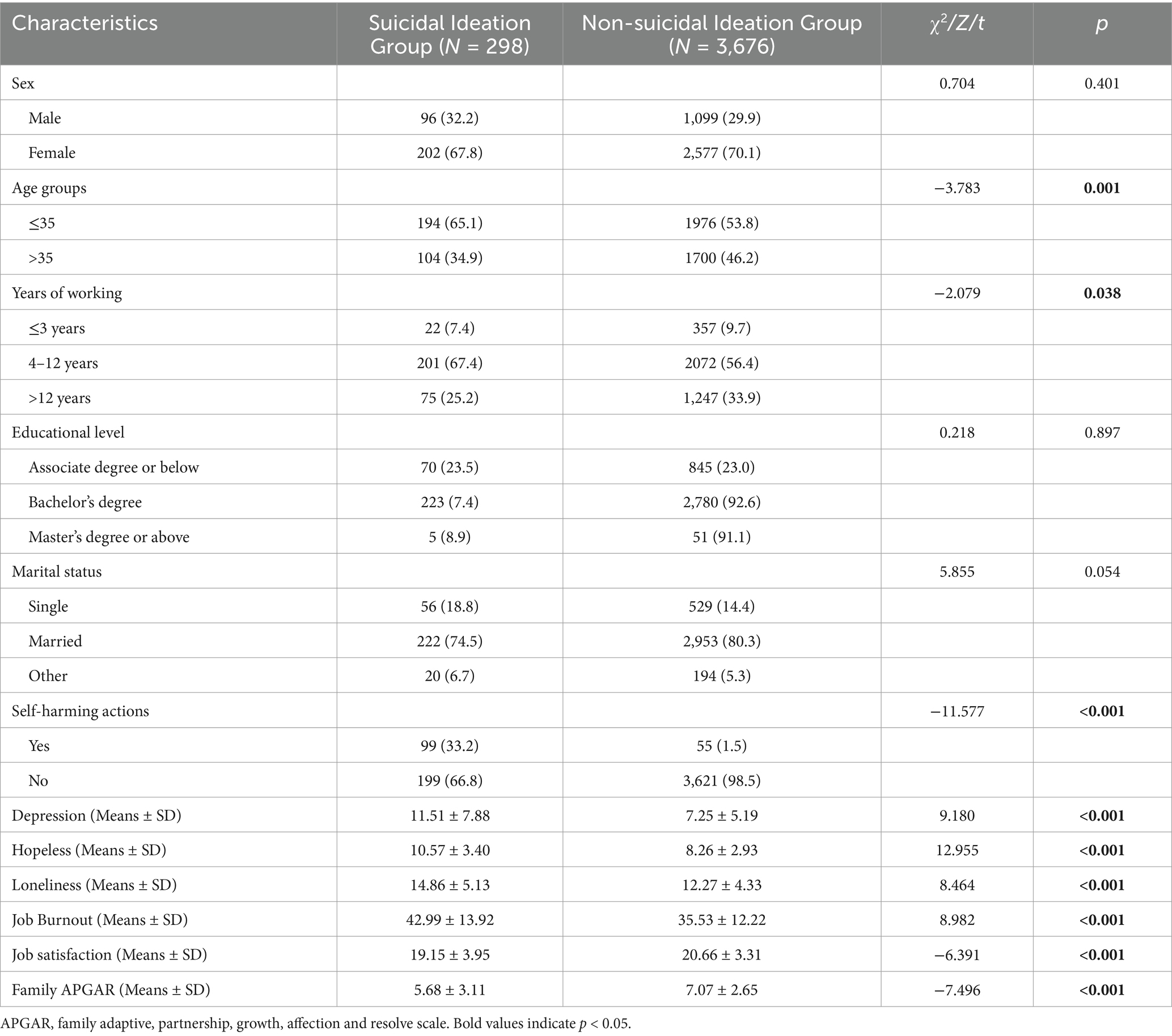
Table 1. Comparison of different characteristics between the suicidal ideation group and non-suicidal ideation group.
Score of each item in quality of life scale
As shown in Table 2, total scores of quality of life in the suicide ideation group and the non-suicide ideation group were 18.59 ± 5.23 and 20.44 ± 3.80, respectively. Compared with the non-suicidal ideation group, the suicide ideation group had lower quality of life scores, indicating that the quality of life of the suicide ideation group was worse than that of the non-suicidal ideation group (p < 0.001).
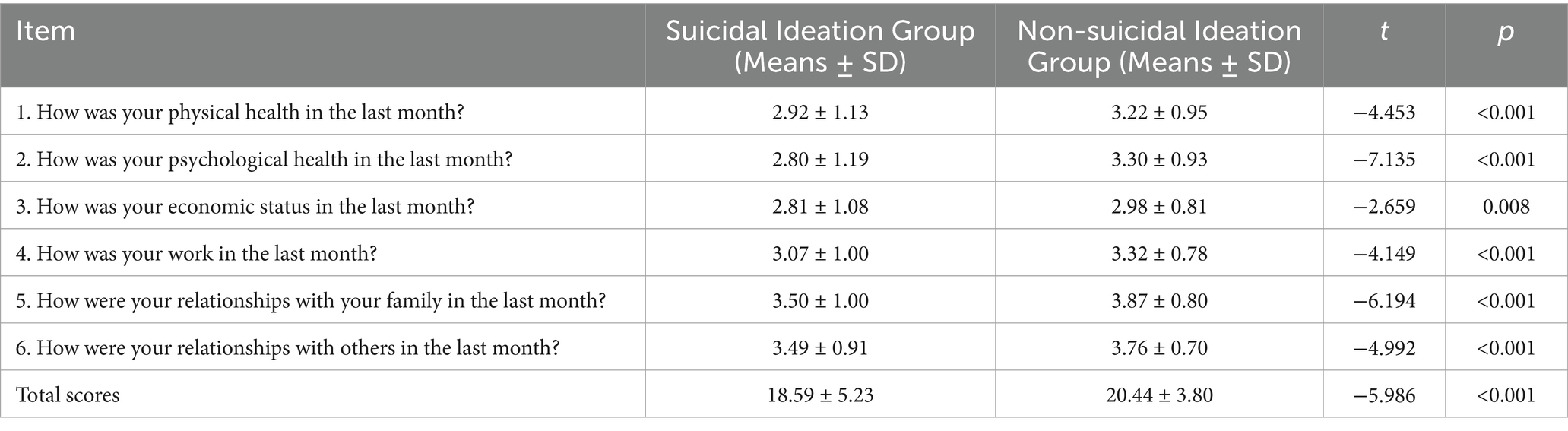
Table 2. The score of each item for suicidal ideation group and non-suicidal ideation group in QOLS-6.
Internal consistency reliability
The Cronbach’s α coefficient of the QOLS-6 scale was 0.865. For the suicidal ideation group and the non-suicidal ideation group, the Cronbach’s α coefficients were 0.908 and 0.857, respectively. This indicates good internal consistency reliability.
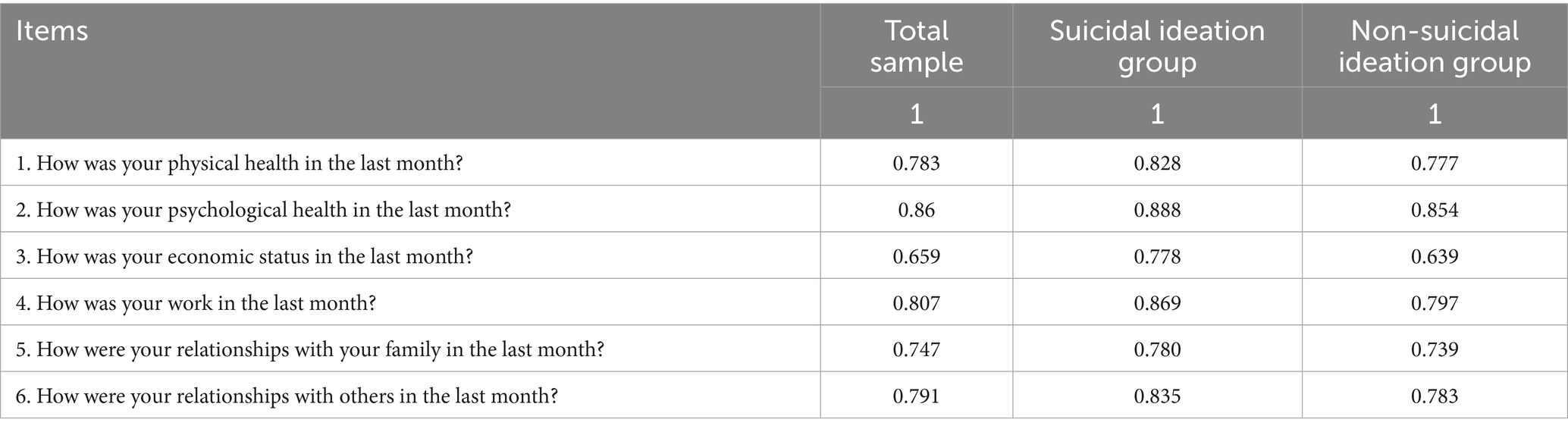
Corrected item-total score correlation
The correlation coefficients between each item of QOLS-6 and the total scores of the suicidal ideation group and the non-suicidal ideation group were 0.673–0.829 and 0.512–0.769, respectively. Cronbach’s α coefficients if item deleted ranged from 0.879–0.902 among suicidal ideation group and varied from 0.807–0.856 among non-suicidal ideation group. The details were shown in Table 3.
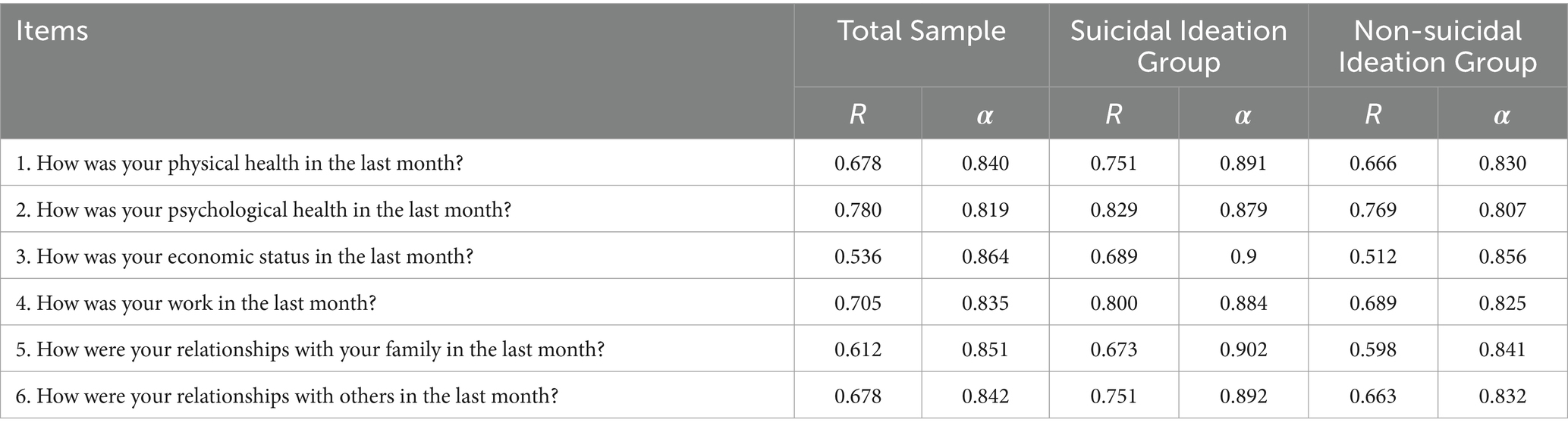
Table 3. Corrected part-whole correlations and Cronbach’s α if item deleted of QOLS-6 among suicidal ideation group and non-suicidal ideation group.
Construct validity
Exploratory factor analysis
For the overall sample, the KMO value was 0.818, and Bartlett’s test of sphericity: χ2 = 12160.210, p < 0.001. The exploratory factor analysis was determined to be suitable for both the suicidal ideation group (KMO = 0.841, Bartlett’s test of sphericity: χ2 = 1264.004, p < 0.001) and the subsample A (KMO = 0.805, Bartlett’s test of sphericity: χ2 = 5208.881, p < 0.001). These results indicate that the data met the necessary criteria for factor analysis, with adequate sampling adequacy and significant correlations among variables.
One common factor was extracted using exploratory factor analysis. The cumulative variance contribution rate was 60.37% for the total sample, 69.00% for the suicide ideation group, and 58.32% for the subsample A, respectively. Exploratory factor analysis extracted one common factor, with Eigenvalue >1.0 and a clear inflection point in the scree plot. Scree plots of exploratory factor analysis of total sample, suicidal ideation group and subsample A are shown in Figures 1A–C. The results of the parallel analysis showed that the eigenvalue of the first factor exceeded the eigenvalue of the first factor in the simulated data set. However, the eigenvalue of the second factor did not exceed the second factor in the simulated data. Consequently, we specified the extraction of only one factor using the promax method of oblique rotation. As shown in Figures 2A–C. Component matrix for each item of the QOLS-6 is shown in Table 4.
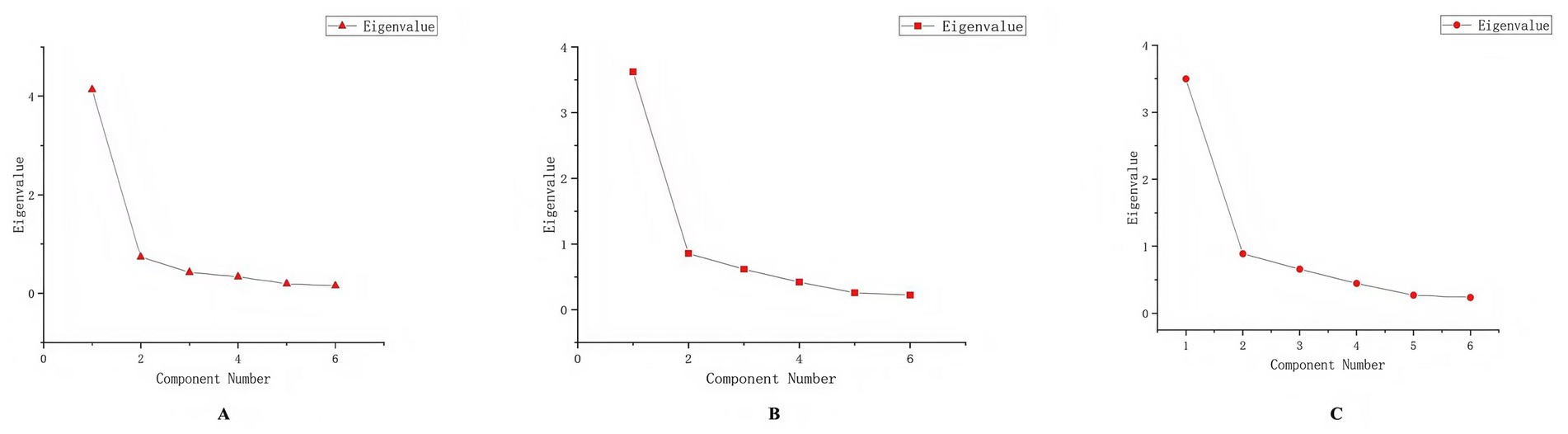
Figure 1. Scree plots from the exploratory factor analysis for (A) the total sample, (B) the suicidal ideation group, and (C) subsample A.

Figure 2. Parallel analysis plots from the exploratory factor analysis for (A) the total sample, (B) the suicidal ideation group, and (C) subsample A.
Confirmatory factor analysis
CFA was conducted on subsample B (n = 1838). As shown in the left panel of Figure 3, the fit indices for the single-factor model did not meet satisfactory standards (χ2 = 891.837, p < 0.001, CFI = 0.838 NFI = 0.837, SRMR = 0.048, RMSEA = 0.231). Considering that quality of life generally encompasses physical and mental health, economic status, and interpersonal relationships (The WHOQOL Group, 1998), and based on the specific content of the scale, correlations were added between items 1 and 2, items 3 and 4, and items 5 and 6. The fit indices improved (χ2 = 33.757, p < 0.001, CFI = 0.995, NFI = 0.994, SRMR = 0.012, RMSEA = 0.050). As shown in the right panel of Figure 3. Consequently, confirmatory factor analysis suggested that a three-factor solution was superior to a one-factor structure.
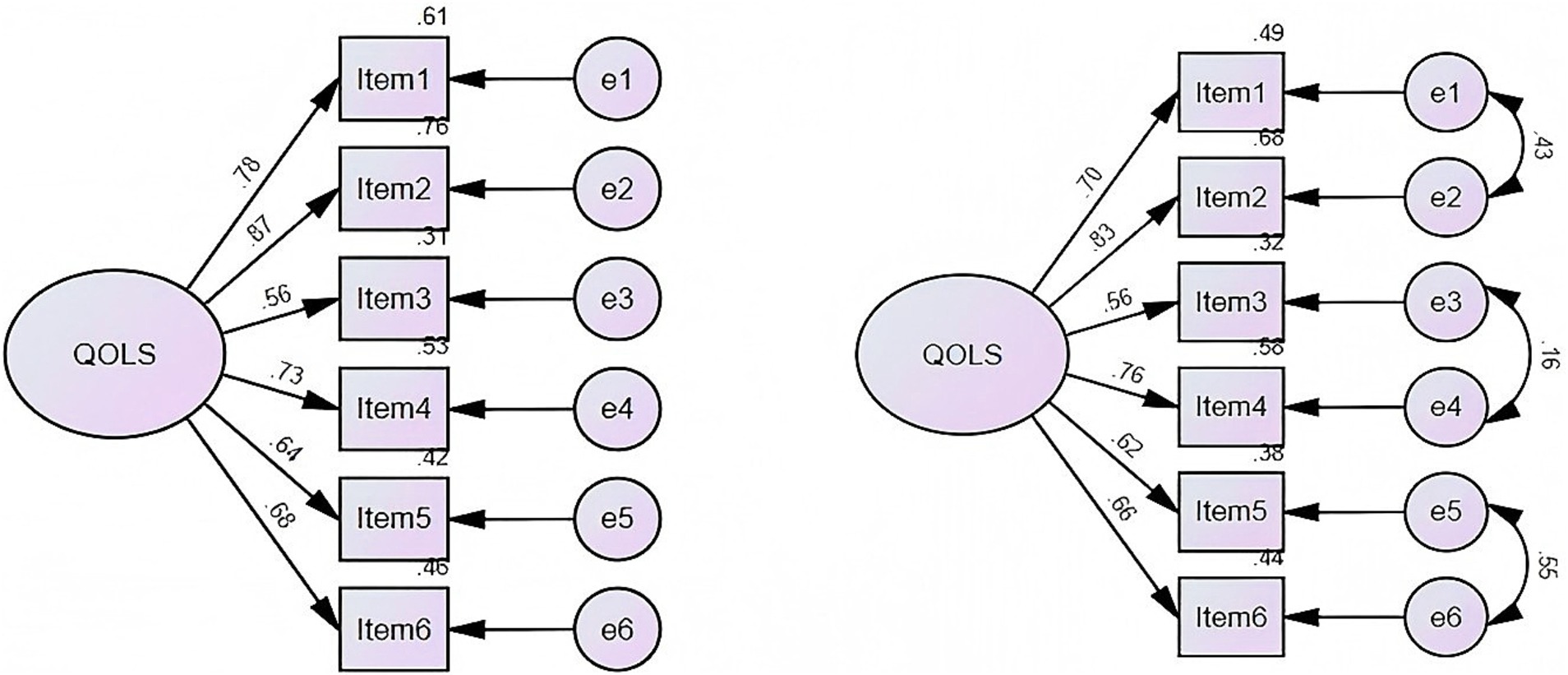
Figure 3. Pathway diagram of the confirmatory factor analysis of the one-factor (left panel) and three-factor (right panel) model for the QOLS-6.
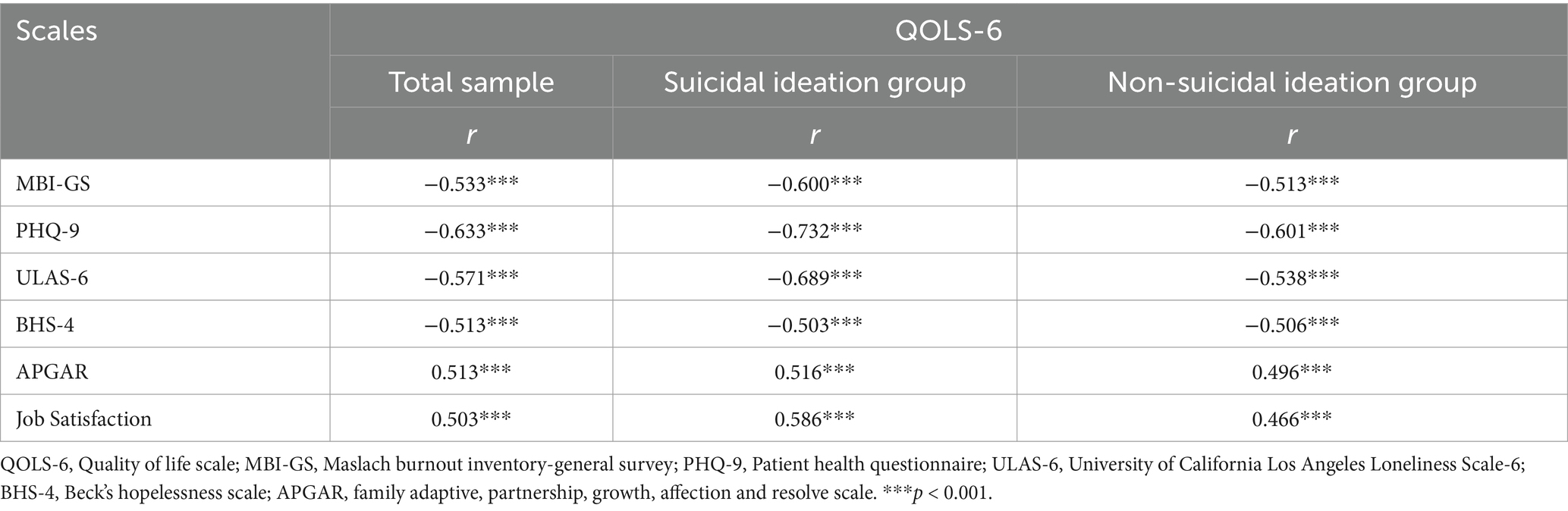
Concurrent validity
Table 5 shows significant correlations between QOLS-6 and other scales. The quality of life among bank employees is positively associated with family function and job satisfaction (p < 0.001), while showing negative associations with job burnout, depression, loneliness, and hopelessness (p < 0.001). In both the total sample and the suicidal ideation group, QOLS-6 exhibits a strong correlation with all other scales (p < 0.01). In the non-suicidal ideation group, QOLS-6 is strongly positively correlated with MBI-GS, PHQ-9, ULAS-6, and BHS-4 (p < 0.01), and moderately negatively correlated with APGAR and Job Satisfaction (p < 0.01).
The results of this study showed that QOLS-6 had good reliability and validity. QOLS-6 is a practical tool to assess the quality of life among the bank occupational population.
The scale was also utilized in a psychological autopsy study conducted among elderly individuals at risk of suicide in rural China (He et al., 2021), demonstrating commendable reliability and validity. However, the mean quality of life scores observed within both the suicide group and non-suicidal ideation group were comparatively lower than those reported in this study, potentially attributable to varying conditions influencing quality of life across diverse groups. Consequently, it is imperative to conduct specific analyses when formulating intervention strategies. The study shows good internal consistency of QOLS-6 in overall sample, and both in the suicidal ideation group and the non-suicidal ideation group. One of the best methods for evaluating internal consistency is Cronbach’s α coefficient, which were used to assess the reliability of QOLS-6. The Cronbach’s α coefficient of the QOLS-6 scale was 0.865. For the suicidal ideation group and the non-suicidal ideation group, the Cronbach’s α coefficients were 0.908 and 0.857, respectively. Also, QOLS-6 has good uniformity and stability in this study. The similar result was reported in the research among suicide elderly (He et al., 2021).
The split-sample EFA-CFA design within the non-suicidal group provides rigorous evidence for the unidimensionality of QOLS-6. The exploratory factor analysis supports a single-factor structure for the QOLS-6, with the analysis revealing only one common factor. This result differs from the finding of two factors identified in the research on elderly people who committed suicide in rural areas (He et al., 2021). Such a discrepancy may be attributed to differences in the characteristics of the populations studied. Confirmatory factor analysis revealed a three-factor structure (physical-mental health, economic-occupational status, and family-social relationships), which significantly improved model fit compared to the original single-factor model (CFI = 0.995 vs. 0.838, RMSEA = 0.050 vs. 0.231). This multidimensional structure aligns with the theoretical framework of quality of life proposed by the World Health Organization. Furthermore, the improved fit indices of the adjusted model suggest that incorporating correlations between items allows for a better capture of the underlying relationships between dimensions. A possible reason why EFA failed to extract three factors is the high correlation among measurement items. When different dimensions of the scale are closely related, EFA may underestimate the number of factors, leading to discrepancies between the factor structures identified by EFA and CFA (Sanatkar and Rubin, 2023). Moreover, EFA is a data-driven approach that assumes factors are uncorrelated by default (Mindrila, 2017). However, different dimensions of quality of life are often interrelated. As a result, EFA may fail to identify an underlying multifactor structure. In contrast, CFA is theory-driven and tests a predefined factor structure based on prior theoretical support. By accounting for correlations among factors, CFA provides a more accurate representation of the theoretical framework. Therefore, the findings support the classification of this scale into three distinct factor dimensions. This finding further validates the interrelationships among the different dimensions of the scale and provides valuable insights for future improvements to the scale.
In this study, quality of life was positive with family function and job satisfaction, negative with job burnout, depression, loneliness, and hopelessness. Depression can seriously lower the quality of life (Malhi and Mann, 2018). The sense of loneliness among elderly in China is negatively correlated with their quality of life (Zhu et al., 2018). Despair plays a mediating role between quality of life and suicide (Chen et al., 2022). A high quality of life reduces depression, hopelessness and suicidal ideation (Büsselmann et al., 2019). Good family function can improve the quality of life for older adults (He et al., 2021). Previous studies have shown similar results, so based on the correlation between these factors, the QOLS-6 also demonstrates good concurrent validity.
Quality of life is closely related to suicidal ideation, and a deep understanding of the relationship between them is helpful to prevent suicide. A large number of studies at home and abroad have proved that suicidal ideation is associated with low quality of life, including rural elderly people (He et al., 2021), community residents (van Spijker et al., 2020), Parkinson’s patients (Santos-García et al., 2023) and so on. In this study, it shows that employees with suicidal ideation have a lower quality of life.
This study, by examining the reliability and validity of the QOLS-6 among bank employees in Guangxi, particularly distinguishing between groups with and without suicidal ideation, demonstrates the scale’s applicability and reliability across different psychological states, holding significant practical implications. The findings not only validate the broad applicability of the scale in mental health assessments but also provide an effective tool for monitoring and intervention in high-stress occupational groups, such as bank employees. Through scientific evaluation of employees’ quality of life, management can promptly identify and address potential mental health issues, enabling targeted support and intervention measures to enhance overall quality of life and job satisfaction.
This study also has limitations. Due to the use of a self-administered questionnaire, the study participants and subjectivity may cause certain bias in data quality and accuracy. Secondly, this study focuses on the bank workers in Guangxi, and further investigation is needed for other groups or countries of people, and more other factors should be taken into consideration. The study aimed to verify the reliability and validity of the QOLS-6 among bank employees, and thus did not conduct an in-depth analysis of the population with suicidal ideation. Future research could explore this topic more extensively, which would help to more comprehensively reveal the characteristics and psychological mechanisms of individuals with suicidal ideation, thereby providing a more scientific basis for formulating targeted intervention strategies.
This study, based on the theoretical framework of quality of life and the design of the scale’s content, measured and analyzed the quality of life of bank employees. Confirmatory factor analysis (CFA) indicated that three latent factors could be extracted from the quality of life scale in this population, and the three-factor model exhibited a better fit than the single-factor model, aligning with theoretical expectations. Additionally, validity testing demonstrated that the scale performed well in terms of concurrent validity. Finally, reliability analysis showed that the internal consistency reliability of the scale reached a high level.
In conclusion, this study confirmed the applicability of the quality of life scale among bank employees in Guangxi, demonstrating its good reliability and validity. The scale can serve as an effective tool for assessing the quality of life of bank employees. However, further assessments of its reliability and validity across different populations and regions are recommended to better evaluate its factor structure.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Medical Ethics Committee of Guangxi Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
QH: Writing – original draft, Formal analysis. QM: Writing – review & editing. HH: Data curation, Investigation. XB: Data curation, Investigation. JZ: Writing – review & editing. ZM: Writing – review & editing, Project administration. GC: Writing – review & editing, Funding acquisition.
The author(s) declare that financial support was received for the research and/or publication of this article. This work was provided by Guangxi Medical University 2020 Undergraduate Innovation and Entrepreneurship Training Program Project (Grant No.: 202010598173).
We are grateful to all the respondents for participating in this study. We also have all thank the investigators for the data collection.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
QOLS-6, Quality of life scale; MBI-GS, Maslach burnout inventory-general survey; PHQ-9, Patient health questionnaire; ULS-6, University of California Los Angeles Loneliness Scale-6; BHS-4, Beck’s hopelessness scale; APGAR, Family adaptive, partnership, growth, affection and resolve scale.
Burckhardt, C. S., and Anderson, K. L. (2003). The quality of life scale (QOLS): reliability, validity, and utilization. Health Qual. Life Outcomes 1:60. doi: 10.1186/1477-7525-1-60
Büsselmann, M., Nigel, S., Otte, S., Lutz, M., Franke, I., Dudeck, M., et al. (2019). High quality of life reduces depression, hopelessness, and suicide ideations in patients in forensic psychiatry. Front. Psych. 10:1014. doi: 10.3389/fpsyt.2019.01014
Chen, G., Mo, Q., Chen, X., Yu, B., He, H., Wang, G., et al. (2022). Quality of life, hopelessness, impulsivity, and suicide in the rural elderly in China: a moderated mediation analysis of psychological autopsy data. Front. Public Health 10:900156. doi: 10.3389/fpubh.2022.900156
Chen, H., Sun, Y., Song, Z., Lin, Z., Sang, Y., Fu, X. A., et al. (2024). Association of depressive symptom severity and suicidal ideation with health-related quality of life among stroke survivors, NHANES 2005-2018. Psychiatry Res. 336:115891. doi: 10.1016/j.psychres.2024.115891
Galiana, L., Oliver, A., Arena, F., De Simone, G., Tomás, J. M., Vidal-Blanco, G., et al. (2020). Development and validation of the short professional quality of life scale based on versions IV and V of the professional quality of life scale. Health Qual. Life Outcomes 18:364. doi: 10.1186/s12955-020-01618-3
Geçkil, T., and Şendoğdu, A. A. (2021). The impact of perceived organizational democracy on the quality of work life: an investigation in the banking sector. Anemon Muş Alparslan Üniversitesi Sosyal Bilimler Dergisi, 9, 497–507.
Goldney, R. D., Fisher, L. J., Wilson, D. H., and Cheok, F. (2001). Suicidal ideation and health-related quality of life in the community. Med. J. Aust. 175, 546–549. doi: 10.5694/j.1326-5377.2001.tb143717.x
Gür, K., Pinar, R., and Erol, S. (2016). Health related quality of life and related factors among bank call center employees. Nobel Med, 12.
Haspels, H. N., de Vries, M., and van den Akker-van Marle, M. E. (2023). The assessment of psychometric properties for the subjective wellbeing-5 dimensions (SWB-5D) questionnaire in the general Dutch population. Qual. Life Res. 32, 237–245. doi: 10.1007/s11136-022-03234-8
He, H., Bai, X., Chen, G., Zhang, Y., and Ma, Z. (2020). Incidence of suicidal intention and its related factors among employees in a bank of Guangxi. J. Guangxi Med. Univ. 37, 2270–2275. doi: 10.16190/j.cnki.45-1211/r.2020.12.031
He, H., Mo, Q., Bai, X., Chen, X., Jia, C., Zhou, L., et al. (2021). Studying suicide using proxy-based data: reliability and validity of a short version scale for measuring quality of life in rural China. PeerJ 9:e12396. doi: 10.7717/peerj.12396
Ki, M., Lapierre, S., Gim, B., Hwang, M., Kang, M., Dargis, L., et al. (2024). A systematic review of psychosocial protective factors against suicide and suicidality among older adults. Int. Psychogeriatr. 36, 346–370. doi: 10.1017/s104161022300443x
Li, Y. (2022). Carrying out humanistic Care for the Banking Industry under the current situation and psychological counseling. Work J. Jilin Finan. Res. 4, 53–56.
Li, X., and Liu, Y. (2021). Thoughts on the work-life balance of employees in county-level banks in second-tier cities and countermeasures. China Collect. Econ. 27, 90–91.
Li, C., and Shi, K. (2003). Influence of fairness of distribution and fairness of procedure on job burnout. Acta Psychol. Sin. 5, 677–684. doi: 10.1016/j.jpsychores.2012.12.017
Ma, Z., He, Q., Nie, G., Jia, C., and Zhou, L. (2020). Reliability and validity of short Beck hopelessness scale in psychological autopsy study among Chinese rural elderly. Int. Psychogeriatr. 32, 525–531. doi: 10.1017/s1041610219001315
Makovski, T. T., Schmitz, S., Zeegers, M. P., Stranges, S., and van den Akker, M. (2019). Multimorbidity and quality of life: systematic literature review and meta-analysis. Ageing Res. Rev. 53:100903. doi: 10.1016/j.arr.2019.04.005
Oladeji, B. D., Taiwo, B., Mosuro, O., Fayemiwo, S. A., Abiona, T., Fought, A. J., et al. (2017). Suicidal behavior and associations with quality of life among HIV-infected patients in Ibadan, Nigeria. J. Int. Assoc. Provid. AIDS Care 16, 376–382. doi: 10.1177/2325957415617829
Phillips, M. R., Yang, G., Zhang, Y., Wang, L., Ji, H., and Zhou, M. (2002). Risk factors for suicide in China: a national case-control psychological autopsy study. Lancet 360, 1728–1736. doi: 10.1016/s0140-6736(02)11681-3
Sanatkar, S., and Rubin, M. (2023). An exploratory investigation of the reliability and validity of the independent-interdependent problem-solving style scale. Int. J. Psychol. 58, 30–41. doi: 10.1002/ijop.12878
Santos-García, D., de Deus Fonticoba, T., Cores Bartolomé, C., Feal Panceiras, M. J., García Díaz, I., Íñiguez Alvarado, M. C., et al. (2023). Suicidal ideation among people with Parkinson's disease and comparison with a control group. Int. J. Geriatr. Psychiatry 38:e5919. doi: 10.1002/gps.5919
Schriesheim, C., and Tsui, A. S. (1980). Development and validation of a short satisfaction instrument for use in survey feedback interventions. Western Academy of Management Meeting.
Smilkstein, G. (1978). The family APGAR: a proposal for a family function test and its use by physicians. J. Fam. Pract. 6, 1231–1239.
Spitzer, R. L., Kroenke, K., and Williams, J. B. (1999). Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders. Patient health questionnaire. JAMA 282, 1737–1744. doi: 10.1001/jama.282.18.1737
Sun, Y., Luk, T. T., Wang, M. P., Shen, C., Ho, S. Y., Viswanath, K., et al. (2019). The reliability and validity of the Chinese short Warwick-Edinburgh mental well-being scale in the general population of Hong Kong. Qual. Life Res. 28, 2813–2820. doi: 10.1007/s11136-019-02218-5
Tan, L. T., Østbye, T., Visaria, A., and Malhotra, R. (2023). Derivation, and establishment of the validity and reliability, of the CASP-11-SG quality of life scale among community-dwelling older adults. Qual. Life Res. 32, 295–306. doi: 10.1007/s11136-022-03238-4
Tentama, F., and Suwandi, G. F. (2020). The quality of work life scale: a psychometric study and its application for the employee. Int. J. Sci. 50, 68–81.
The WHOQOL Group (1998). Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL Group. Psychol. Med. 28, 551–558. doi: 10.1017/s0033291798006667
van Krugten, F. C. W., Busschbach, J. J. V., Versteegh, M. M., Hakkaart-van Roijen, L., and Brouwer, W. B. F. (2022). The mental health quality of life questionnaire (MHQoL): development and first psychometric evaluation of a new measure to assess quality of life in people with mental health problems. Qual. Life Res. 31, 633–643. doi: 10.1007/s11136-021-02935-w
van Spijker, B. A. J., Batterham, P. J., Calear, A. L., Wong, Q. J. J., Werner-Seidler, A., and Christensen, H. (2020). Self-reported disability and quality of life in an online Australian community sample with suicidal thoughts. J. Affect. Disord. 263, 707–714. doi: 10.1016/j.jad.2019.11.050
Wang, H. L., and Zhao, X. M. (2008). Analysis of the health status of Bank employees in different altitude areas. Qinghai Med. J. 5, 57–58.
WHOQOL (1993). Study protocol for the World Health Organization project to develop a quality of life assessment instrument (WHOQOL). Qual. Life Res. 2, 153–159. doi: 10.1007/BF00435734
Xue, H., Omar Din, N. N., Balakrishna, S., and Zainal, N. (2024). Relationship between motivation determinants and job satisfaction among the employees of Bank of China, Shanghai. Int. J. Acad. Res. Bus. Soc. Sci. 14, 825–840. doi: 10.6007/IJARBSS/v14-i1/20475
Zhou, L., Li, Z., Hu, M., and Xiao, S. (2012). Reliability and validity of ULS-8 loneliness scale in elderly samples in a rural community. J. Central South Univ. 37, 1124–1128. doi: 10.3969/j.issn.1672-7347.2012.11.008
Zhou, J., Xu, L., Pan, J., Wang, M., Zhou, P., Wang, W., et al. (2024). A comparative study of Chinese medicine quality of life assessment scale (CQ-11D) and EQ-5D-5L and SF-6D scales based on Chinese population. Qual. Life Res. 33, 113–122. doi: 10.1007/s11136-023-03512-z
You may also like...
Diddy's Legal Troubles & Racketeering Trial

Music mogul Sean 'Diddy' Combs was acquitted of sex trafficking and racketeering charges but convicted on transportation...
Thomas Partey Facing Rape & Sexual Assault Charges

Former Arsenal midfielder Thomas Partey has been formally charged with multiple counts of rape and sexual assault by UK ...
Nigerian University Admission Policy Changes

JAMB has clarified its admission policies, rectifying a student's status, reiterating the necessity of its Central Admis...
Ghana's Economic Reforms & Gold Sector Initiatives

Ghana is undertaking a comprehensive economic overhaul with President John Dramani Mahama's 24-Hour Economy and Accelera...
WAFCON 2024 African Women's Football Tournament

The 2024 Women's Africa Cup of Nations opened with thrilling matches, seeing Nigeria's Super Falcons secure a dominant 3...
Emergence & Dynamics of Nigeria's ADC Coalition

A new opposition coalition, led by the African Democratic Congress (ADC), is emerging to challenge President Bola Ahmed ...
Demise of Olubadan of Ibadanland
Oba Owolabi Olakulehin, the 43rd Olubadan of Ibadanland, has died at 90, concluding a life of distinguished service in t...
Death of Nigerian Goalkeeping Legend Peter Rufai

Nigerian football mourns the death of legendary Super Eagles goalkeeper Peter Rufai, who passed away at 61. Known as 'Do...