BMC Psychiatry volume 25, Article number: 554 (2025) Cite this article
Mechanical restraint, a widely utilized yet contentious restrictive intervention in psychiatric practice, adversely affects both physical and psychological well-being of patients. Understanding the determinants associated with its implementation is crucial for reducing its clinical application. Current studies have primarily evaluated factors influencing mechanical restraint use and related organizational adaptations, but these investigations are limited to short-term observations. Furthermore, research examining correlates in patients subjected to recurrent mechanical restraint episodes in open psychiatric wards remains scarce, with biological contributing factors particularly lacking empirical evidence.
This study aimed to analyze differences between inpatients experiencing single versus multiple restraint episodes in the open psychiatric ward setting and identify factors associated with multiple restraint occurrences.
This study is a retrospective analysis of electronic health record data from patients who underwent mechanical restraint in the open psychiatric ward of a Class III Grade A general hospital in China between 2016 and 2021. The data encompassed sociodemographic information, clinical characteristics, and biological indicators.
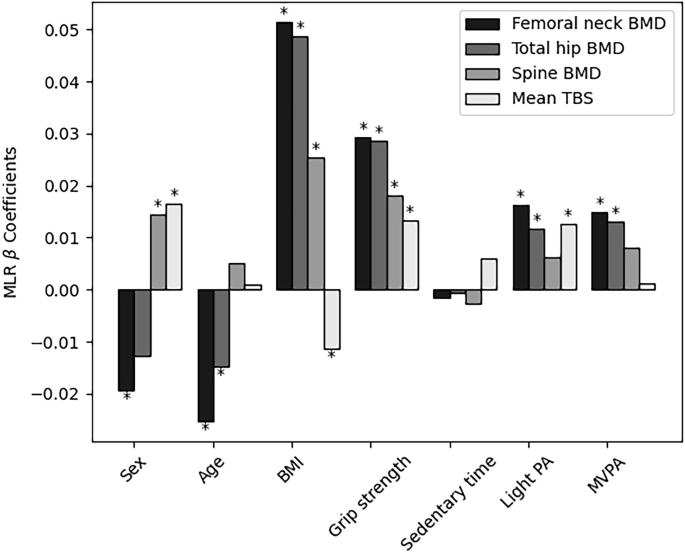
The study included a total of 449 patients who underwent mechanical restraint during hospitalization. Of these, 63.5% experienced a single episode of restraint, while 36.5% experienced multiple episodes. Furthermore, compared to patients with a single episode of mechanical restraint, those with multiple episodes exhibited a significantly earlier timing of the first restraint (p = 0.011), a prolonged hospital stay (p = 0.044), and relatively higher creatine kinase levels (p = 0.008). Multivariate analysis identified the timing of restraint (OR: 0.947, p = 0.005) and the duration of hospitalization (OR: 1.034, p = 0.003) as significant predictors of multiple restraint episodes.
Among psychiatric inpatients in open wards, those subjected to multiple restraints exhibited earlier occurrence of the first restraint after admission, prolonged hospital stays, and relatively higher serum creatine kinase levels at admission. These findings suggest that in clinical practice, repeated restraint may potentially prolong hospitalization duration. Monitoring serum creatine kinase levels at admission may aid in identifying patients at risk for repeated restraints. Furthermore, early risk identification and the implementation of alternative interventions are critical to reducing the necessity for restraint interventions.
Restraint is defined as a compulsory intervention that restricts an individual’s freedom of movement [1]. Currently, it primarily includes the following types: (1) Environmental restraint: Defined as restricting a patient’s free access to their environment, often used to prevent patients from leaving a specific area [2]. (2) Psychological restraint: Involves any decision or plan that limits patient privileges and participation in activities [3]. (3) Chemical restraint: Refers to the use of medication to manage a patient’s behavior, which is not part of the standard treatment or dosage for the patient’s condition [4]. (4) Physical restraint: Further categorized into manual, mechanical, and physical-psychological restraints. Among these, mechanical restraint (MR) refers to the direct application of a mechanical device to the patient’s body or in close proximity, which is difficult for the patient to remove, aiming to prevent, restrict, or control the patient’s freedom of physical movement [1].
Patients with mental illnesses often exhibit behaviors such as excitement, agitation, aggression toward others, property destruction, impulsivity, elopement, and non-compliance with treatment due to the influence of psychiatric symptoms. These behaviors necessitate the use of compulsory medical interventions, such as restraints. MR is primarily employed in emergency situations to manage patients who display potentially dangerous behaviors associated with mental illness and fail to respond to de-escalation strategies. Its application aims to ensure the safety of both the patients themselves and others, as well as to prevent destructive behaviors [5,6,7]. In the field of mental health, MR is widely utilized.A 2020 report on the use of MR in psychiatric wards across Pacific Rim countries revealed that New Zealand experienced 0.031 restraint events per million people per day, Japan recorded 98.8 restraint events per million people per day, and Australia had 0.165 restraint events per million people per day [8]. In China, the utilization rate of psychiatric restraints remains notably high and continues to rise. According to statistics, the rate increased from 42.6% in 1994 to 54.1% in 2019 [9].
The use of MR remains a subject of global controversy. Due to its coercive nature, the long-term or inappropriate application of MR can adversely affect both the physical and psychological well-being of patients. For instance, it may lead to recurrent trauma, deep vein thrombosis in the lower limbs, the development of negative emotions, and prolonged hospitalization [10]. Additionally, improper use of MR can result in permanent injuries (such as to the wrists, legs, or nerves) or even death [11]. Furthermore, MR can undermine patients’ self-esteem and autonomy, erode their trust in healthcare professionals, and negatively impact therapeutic relationships [12, 13]. Qualitative studies have also demonstrated that MR is a traumatic experience, which not only interferes with the therapeutic process [14] but also creates ethical dilemmas for healthcare staff [15].In recent years, significant efforts have been made at local, national, and international levels to reduce the use of MR and other forms of restraint [7, 8, 16]. However, the current utilization of MR in the mental health field remains relatively prevalent. Studies have reported that 53.6% of patients undergoing MR have experienced more than one episode of restraint [17], and this group of frequently restrained patients accounts for a substantial proportion of restraint occurrences [18]. Multiple restraints tend to exacerbate the traumatic experiences of patients and may also be associated with more complex conditions and refractory mental illnesses.Therefore, studying the factors associated with patients experiencing multiple restraints is of significant importance. It aims to identify vulnerable patient groups at risk of repeated restraints, improve interventions to reduce the frequency of restraint use, and enhance the overall treatment and experience of patients.
However, research on the factors associated with multiple restraints has been limited in recent years. The following factors have been identified as potentially associated with experiencing multiple restraints: age [18,19,20,21], previous hospitalization history [18], not being readmitted within 30 days of previous discharge [20], length of hospitalization [18,19,20, 22], and disease diagnosis (bipolar disorder and personality disorder) [19]. Nevertheless, the findings of these studies are inconsistent. Moreover, current research on factors influencing multiple MR episodes remains scarce, with retrospective study durations ranging from 1 to 3 years. In some studies, patients experienced dual restraints, pharmacological restraints, and MR. The identified influencing factors primarily focus on sociodemographic, clinical characteristics, and organizational factors, with limited exploration of biological indicators.Previous studies have reported that violent behavior or threats of violence are common indications for the use of MR [23]. Violent and aggressive behaviors in patients with mental illnesses are associated with certain biological indicators [24,25,26], such as creatine kinase, cortisol, and thyroid hormones. However, there is a paucity of research investigating whether these biological indicators are factors influencing the experience of MR or multiple MR episodes. Investigating the multifaceted influencing factors of MR holds significant clinical importance for reducing its occurrence.Furthermore, previous studies have predominantly focused on patients in mixed psychiatric institutions and acute psychiatric wards, with a notable lack of related research on patients in open psychiatric wards.
With the transformation and evolution of medical models, the open management approach in psychiatric departments has gradually gained adoption. Compared to patients in closed wards who undergo compulsory treatment, patients in open wards voluntarily accept treatment, are permitted to move freely in and out of the wards, and engage with society, which is more conducive to maintaining and restoring social functioning. They also experience greater respect for their human rights and personal dignity [20]. However, the prevention of risks such as patient suicide, elopement, and violence has become a significant management challenge. The use of compulsory treatment interventions, including restraint during emergency situations, is often unavoidable, which conflicts with the initial emphasis on respecting patient autonomy and self-esteem. This may result in more intense traumatic experiences and negative emotions among patients, ultimately affecting treatment outcomes and recovery.Therefore, it is imperative to investigate the factors influencing the use of MR in open psychiatric wards to reduce its application. Some studies have reported that the use of MR in open psychiatric wards is associated with factors such as gender, diagnosis (e.g., schizophrenia), and stimulant abuse [27]. However, there is a notable lack of research on factors related to patients experiencing multiple restraints.
In this study, we focused on an open psychiatric ward—a clinical setting that has been scarcely explored in prior research. Additionally, we targeted patients subjected to restraint within this understudied context, encompassing both those with single and multiple episodes of restraint. To enhance the robustness of our findings, we extended the retrospective observation period to six years and included a larger sample size (n = 449). Additionally, biological indicator variables were incorporated. This study aimed to analyze differences between inpatients experiencing single versus multiple restraint episodes in the open psychiatric ward setting and identify factors associated with multiple restraint occurrences. We addressed the following research questions: (1)What are the significant differences between inpatients experiencing single versus multiple restraint episodes in open psychiatric wards? (2)What factors are associated with the occurrence of multiple restraint episodes in this setting?
Study design
This study is a retrospective study.
Participants
This study included hospitalized patients who had undergone mechanical restraint in the open wards of the mental health center at a Class III Grade A general hospital -the highest level in China’s hospital accreditation system-in Sichuan Province, China, between January 1, 2016, and December 30, 2021. Diagnoses were made according to the International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10). Inclusion criteria: (1) Patients who had experienced mechanical restraint. (2) Blood tests were conducted within 24 h after admission. (3) Completed demographic data were collected. Exclusion criteria: (1) Any brain, heart, muscle, or endocrine disorders. (2) Patients who had engaged in intense physical exercise or were restrained before blood collection. (3) Pregnancy. (4) Patients exhibiting fever within 24 h of blood collection.(5) Received depot antipsychotics in the last 6 months.
Data were extracted from the institution’s electronic medical record system, with the following variables collected from patients’ medical records: (1) Sociodemographic factors, including age, gender, marital status, and education level; and (2) clinical factors, including diagnosis, whether it was the first admission, timing of restraint (for patients with multiple restraints, the time of the first restraint after admission was recorded), duration of restraint, length of hospitalization, history of violence, and frequency of restraint. (3) Biological indicators including cortisol, adrenocorticotropic hormone (ACTH), alkaline phosphatase (ALP), creatine kinase (CK), and thyroid function tests, with the first blood test results within 24 h after admission collected for both single-restraint and multiple-restraint patients. Additionally, this study employed the Chinese version of the Broset Violence Checklist (BVC) for violence risk assessment. The BVC was translated and adapted into Chinese by Chinese scholars in 2016, demonstrating a content validity index of 0.93 and a Cronbach’s alpha coefficient of 0.76, indicating good internal consistency reliability. The scale comprises six items: confusion, irritability, boisterousness, physical threats, verbal threats, and attacks on objects. Each item is scored as 0 or 1 based on the presence of the corresponding behavior, with a maximum total score of 6. Higher scores indicate a greater likelihood of future violent behavior [28].
The study utilized single and multiple restraints as grouping criteria, and data entry and analysis were conducted using SPSS 26.0 statistical software. For normally distributed continuous variables, independent t-tests were applied, while non-normally distributed variables were analyzed using the Mann-Whitney U test. Categorical variables were assessed using the chi-square test. Logistic regression analysis was performed with the occurrence of multiple MR as the dependent variable to explore related influencing factors. A p-value of less than 0.05 was considered statistically significant.
Sociodemographic characteristics
This study included a total of 449 psychiatric patients who underwent MR during hospitalization, consisting of 201 males (44.8%) and 248 females (55.2%). Among them, 63.5% of the patients experienced a single restraint, while 36.5% experienced multiple restraints. The two subgroups demonstrated no significant differences in age, gender, marital status, or education level (Table 1).
Clinical characteristics
In the comparison of clinical characteristics, patients with schizophrenia and mental disorders accounted for the highest proportion among all restrained patients, with 35.4% in the single-restraint group and 41.5% in the multiple-restraint group. However, there was no significant difference in diagnoses between the two subgroups. Compared to the timing of restraint in the single-restraint group (Median = 4 days, IQR = 2 ∼ 8), the timing of restraint in the multiple-restraint group occurred earlier (Median = 3 days, IQR = 1.25 ∼ 7), and the difference was statistically significant (p = 0.011). Additionally, compared to the length of hospital stay in the single-restraint group (Median = 18 days, IQR = 14 ∼ 26), the multiple-restraint group had a significantly longer hospital stay (Median = 20 days, IQR = 15 ∼ 26), and the difference was statistically significant (p = 0.044) (Table 2).
Biological indicators
In the comparison of laboratory-related biological indicators, there were no statistically significant differences between the single-restraint group and the multiple-restraint group in terms of cortisol, adrenocorticotropic hormone, alkaline phosphatase, or thyroid function-related indicators. However, in the comparison of creatine kinase levels, the multiple-restraint group had higher creatine kinase values (Median = 111.5, IQR = 66.75 ∼ 229) than the single-restraint group (Median = 87, IQR = 62 ∼ 155.5), and the difference was statistically significant (p = 0.008) (Table 3).
In the logistic regression analysis, the timing of restraint was significantly associated with multiple restraints. The earlier the first restraint occurred after admission, the higher the risk of multiple restraints (OR: 0.947, 95% CI: 0.911–0.984, p = 0.005). Additionally, the occurrence of multiple restraints was significantly correlated with the length of hospital stay (OR: 1.034, 95% CI: 1.011–1.057, p = 0.003). However, no statistically significant relationship was observed between multiple restraints and serum creatine kinase levels (Table 4).
The present study revealed that more than 36.5% of all patients who experienced restraint underwent multiple restraints during their hospitalization, a proportion higher than that reported by Guzman-Parra (2.59%) [20]. This discrepancy may be attributed to the younger mean age of patients who underwent multiple MR in our study (29.6 years) compared to the mean age of patients in Guzman-Parra’s study (38.6 years). Younger age has been associated with an increased risk of multiple restraints [18, 20], likely due to the greater difficulty in managing aggressive and disordered behaviors in younger populations [29]. Additionally, Guzman-Parra’s study was conducted from 2012 to 2014, during which an intervention program to reduce mechanical restraints was implemented in their department at the beginning of 2013, potentially contributing to the lower proportion of patients with multiple MR. Furthermore, the results of this study were lower than those reported by Chinese scholars Gao et al. (53.6%) [17], likely because our study focused on patients in open wards and did not include closed wards or acute psychiatric wards, where the majority of patients receive compulsory treatment and the use of MR may be more prevalent. Based on these findings, scientific and rigorous nursing identification and intervention should be implemented as early as possible for psychiatric open ward inpatients who experience multiple MRs.
The results of this study indicate that patients who experienced multiple restraints underwent their first restraint earlier compared to those who experienced a single restraint. Furthermore, the earlier the first restraint occurred after admission, the higher the risk of multiple restraints. Mechanical restraint events were most likely to occur within the first week of hospitalization, consistent with findings from other studies [17, 30,31,32], which have confirmed a higher risk of restraint during the initial phase of hospitalization. Previous research has also demonstrated that early initial physical restraint is associated with increased restraint use (an 11% increase) [30]. This may be attributed to the relatively severe symptoms of patients in the early stages of admission, frustration with repeated treatments, and a higher incidence of aggressive behaviors during the initial hospitalization period [33]. Therefore, it is recommended to monitor emotional or physical distress symptoms as early as possible after admission, maintain a positive attitude, and implement mental health education to help patients quickly adapt to ward routines and learn useful strategies. These measures can alleviate potential conflicts and provide patients with appropriate support to relieve physical or psychological distress, thereby reducing the need for MR [27]. Additionally, the early application of pharmacological treatments and de-escalation measures can help avoid the use of coercive interventions [34, 35]. Establishing a good doctor-patient relationship early after admission facilitates the initiation of treatment and the application of verbal de-escalation and other de-escalation strategies prior to restraint [36]. Patient interviews also emphasize the importance of maintaining communication and constructive interaction between patients and staff in situations where restraint might be considered [37].
Regarding the effect of MR on the length of hospitalization, previous studies have demonstrated that the use of restraints during hospitalization is significantly associated with prolonged hospital stay [5, 30, 38], suggesting that MR is linked to extended hospitalization. This study also found that receiving multiple MRs during hospitalization is significantly correlated with a longer hospital stay. Patients who experienced multiple restraints had significantly longer hospital stays compared to those who experienced a single restraint. Regression analysis further revealed that the longer the hospital stay, the higher the risk of multiple restraints, which aligns with findings from other studies [18, 20]. This may be attributed to the fact that patients requiring longer hospital stays tend to have more severe or unstable conditions and exhibit more difficult-to-control or aggressive behaviors [15, 39], ultimately leading to the implementation of multiple restraints by hospital staff. Although it can be hypothesized that multiple MRs may contribute to prolonged hospitalization, due to the limitations of the study design, a causal relationship between receiving multiple MRs and increased hospital stay cannot be established. Therefore, the potential association between receiving multiple MRs and increased hospitalization time warrants further systematic investigation. If a causal relationship is identified between reducing the frequency of MR use and shortening hospitalization time, it would have significant psychological and economic implications, as MRs can cause patient distress and numerous adverse outcomes, and longer hospital stays are associated with high medical costs and disease burden [40].
Serum creatine kinase (CK), also known as creatine phosphokinase (CPK), is composed of three isoenzymes: CK-MM, CK-MB, and CK-BB. It is widely distributed in skeletal muscle, cardiac muscle, and brain tissue. CK reversibly catalyzes the conversion of creatine and adenosine triphosphate (ATP) into phosphocreatine and adenosine diphosphate (ADP), thereby ensuring an adequate energy supply for tissue cells. Previous studies have reported elevated CK levels in patients with psychiatric disorders, such as schizophrenia and affective psychoses [41]. Specifically, serum CK levels are elevated in patients with schizophrenia exhibiting aggression, and elevated CK levels are positively correlated with the risk of aggression [42]. Additionally, serum CPK levels at the time of hospital admission have been shown to correlate with aggressive behavior prior to admission as well as with the need for isolation due to the risk posed to others during hospitalization [43]. Furthermore, elevated CK levels at admission are associated with an increased likelihood of any type of aggression, including verbal and physical aggression.A strong association has been observed between aggressive behavior and the use of restraints, with higher CK levels detected in individuals who engaged in aggressive behavior during hospitalization for mental illness and in those who were restrained compared to those who were not restrained [24, 41]. This study found that patients subjected to multiple MR episodes had significantly higher creatine kinase (CK) levels at admission compared to those with single episodes (p = 0.008), with mean values exceeding the normal range. Elevated CK levels may reflect heightened internal stress responses [43], potentially attributable to psychomotor agitation-induced hypermetabolic muscle activity and subsequent CK-MM elevation via muscle injury-mediated enzyme release [44].
All biomarker measurements were conducted within 24 h post-admission, consistent with the CK level assessment timeframe in previous studies [41, 42], thereby reflecting only the observed baseline status without accounting for stress-related CK fluctuations, which limits result generalizability. Additionally, Due to the retrospective design of this study, the inconsistent intervals between repeated blood tests in constrained patients rendered these data difficult to interpret and analyze. Therefore, repeated blood test indicators were not collected, and trends in CK levels among MR patients across different time periods could not be described.These findings nevertheless suggest that psychiatric patients presenting with relatively elevated baseline CK levels warrant clinical attention through comprehensive risk assessment, with corresponding preventive or intervention measures guided by combined risk evaluation and clinical judgment. Future prospective studies could be conducted to further explore the relationship between CK level changes at regular intervals and MR in patients with multiple restraints.
Our study has several limitations. First, it is a retrospective study design that focuses solely on analyzing the variables collected. It lacks data on patients’ prior experience with restraints and does not account for several other factors that may influence the decision to use MR, such as those related to staff and ward conditions. Second, this study was conducted exclusively in an open psychiatric ward of a Class III Grade A general hospital in China, which may limit the generalizability of the findings to patients in closed wards or acute psychiatric settings.Again, Our study did not assess the intervals between initial and recurrent restraints in patients undergoing multiple restraint episodes. Future studies should analyze temporal patterns of restraints in this population to better characterize their clinical profiles and identify potential periodicity in the occurrence of restraints. However, this study has the advantage of having six years of data and a large number of variables collected, all from the same health care unit, whose staff and environment in which restraint was administered remained relatively stable.
This study may assist healthcare professionals in identifying patient characteristics associated with frequent MR use. The cohort exhibited earlier initial restraint episodes and prolonged hospitalizations, highlighting the importance of establishing therapeutic alliances at the earliest clinical stage. Early risk identification, coupled with the development of tailored preventive strategies and alternative interventions for this population, could optimize clinical management and reduce MR utilization. Furthermore, by exploring biological indicators in restrained patients, this work provides novel insights into the profiling of individuals prone to repeated restraints and advances a biologically informed perspective for MR management.Future research is warranted to further investigate the biological signatures of psychiatric patients subjected to restraint, with the aim of identifying durable and stable biomarkers associated with MR episodes. The incorporation of such biological indicators into clinical risk assessment and decision-making processes could provide novel insights for characterizing restrained patients and reducing the use of MR.
Among psychiatric inpatients in open wards, those subjected to multiple restraints exhibited earlier occurrence of the first restraint after admission, prolonged hospital stays, and relatively higher serum creatine kinase levels at admission. These findings suggest that in clinical practice, repeated restraint may potentially prolong hospitalization duration. Monitoring serum creatine kinase levels at admission may aid in identifying patients at risk for repeated restraints. Furthermore, early risk identification and the implementation of alternative interventions are critical to reducing the necessity for restraint interventions.
The datasets generated and/or analyzed during the current study are not publicly available but can be obtained from the corresponding author upon reasonable request.
Not applicable.
This study was conducted in compliance with the Declaration of Helsinki and was reviewed and approved by the Ethics Committee of West China Hospital of Sichuan University (Approval Number: K2021010). Due to the retrospective nature of the study and the use of anonymized data, the requirement for informed consent from participants was exempted.
Not applicable.
The authors declare no competing interests.
Not applicable.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Wen, S., Guo, L., You, Q. et al. Influencing factors of the implementation of mechanical restraint in open psychiatric ward: a retrospective study (2016–2021). BMC Psychiatry 25, 554 (2025). https://doi.org/10.1186/s12888-025-06969-z




(3).jpeg)