H syndrome presenting with bilateral cheek enlargement and an SLC29A3 gene variant
H syndrome presenting with bilateral cheek enlargement and an SLC29A3 gene variant
An adolescent girl presents with bilateral cheek enlargement, hyperpigmentation and hypertrichosis of the lower extremities with otological, cardiac, endocrine, and hepatosplenic involvement. Clinical findings supplemented by histopathological and wide exome sequencing results led to the diagnosis of H syndrome. The genetic testing showed a homozygous frameshift mutation in the SLC29A3 gene involving unique exon and codons. This case highlights the unique characteristics of H syndrome observed in a Filipino female with a variant of the SLC29A3 gene mutation.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
H syndrome is a rare autosomal recessive genodermatosis caused by SLC29A3 gene mutations.1 The term was coined in 2008 after describing 10 patients from consanguineous Arab families presenting with characteristic cutaneous and multisystemic manifestations.2 There are only approximately 130 cases of H syndrome reported in the literature.3 Here, we present a case of H syndrome with bilateral cheek enlargement and a variant of the SLC29A3 gene mutation in an adolescent female. This is the first case of H syndrome documented in Filipino ethnicity to the best of the authors’ knowledge.
The patient is the second child of a non-consanguineous marriage. No other relatives are affected. The patient does not have limitations in activities of daily living and no developmental delays, but her appearance affects her self-esteem.
An adolescent female was referred to our institution for gradual, painless, bilateral cheek hypertrophy which started at 2 years of age. No work-up was done, but a previous diagnosis of sialolithiasis was given to the family and conservative management was advised. During this period, the patient also developed hyperpigmented patches with hypertrichosis on the left lower extremity. On physical examination, she presented with severe stunting and wasting with height of 131 cm (below third percentile) and weight of 28.5 kg (Body mass index (BMI) 16.6 kg/m2) (below third percentile). Bilaterally, her cheeks were diffusely enlarged with no palpable masses but with overlying telangiectasias (figure 1A). There were neither palpable intraoral masses nor lymphadenopathies. A grade 3/6 systolic murmur on the left upper parasternal border was noted. She had secondary amenorrhoea and delayed development of secondary sexual characteristics with breast sexual maturity rating of Tanner stage 2 and absence of pubic hair. She had symmetric, diffuse, fairly defined, indurated brown plaques and patches with overlying black coarse terminal hairs, associated with warmth and tenderness on the hypogastric and sacral area, bilateral anterior, medial, and lateral thighs and legs, with sparing of the knees (figure 1B–E). The upper extremities, chest, palms and soles were unaffected.
Based on the clinical findings, a diagnosis of H syndrome was suspected. Pure tone audiometry revealed normal hearing thresholds on the right ear and mild sensorineural hearing loss on the left ear, both with a 4 kHz notch. Thoracic CT scan with intravenous contrast showed bilateral pleural and pericardial thickening with mild hepatosplenomegaly. Meanwhile, the patient’s 2D echocardiogram and chest x-ray were unremarkable. Her complete blood count and peripheral blood smear showed microcytic hypochromic anaemia with low haemoglobin (75 g/L), normal white cell count and thrombocytosis (676×109 /L), while erythrocyte sedimentation rate (ESR) was normal (10 mm/hour). She had normal fasting blood sugar (89.3 mg/dL) and HbA1c (4.8%). Endocrine work-up showed follicle-stimulating hormone and luteinizing hormone on the low-normal levels while insulin-like growth factor 1 was low (73.26 ng/mL). A 5-mm skin biopsy of the bilateral thighs revealed a fibrohistiocytic proliferation with lobular panniculitis, and immunostaining showed cells to be positive with CD68 and S100 and negative with CD1a and PAS (figure 2). Craniofacial MRI revealed symmetric hypertrophy with focal fatty infiltration of the facial muscles, temporalis and masseter. The mandible, maxilla, zygoma, sphenoid and clivus exhibited bony expansion. Similarly, in the skeletal survey, there was symmetric medullary expansion with cortical thinning detected in the maxilla, mandible and zygoma. An ultrasound-guided core needle biopsy of the right cheek was done, which also revealed sections of fibrohistiocytic proliferation with panniculitis, with CD68-positive and CD1a-negative staining patterns. These were similar to the biopsy findings on the skin and consistent with H syndrome. The IgG4 levels of the patient were within normal limits, making IgG4-related disorders less likely. Furthermore, whole genome sequencing was performed which revealed a homozygous frameshift mutation variant in SLC29A3, Exon 6, c.1350_1354del (p.Val451Aspfs*103), disrupting the last 25 amino acids of the SLC29A3 protein and extending the protein by 77 additional amino acid residues.
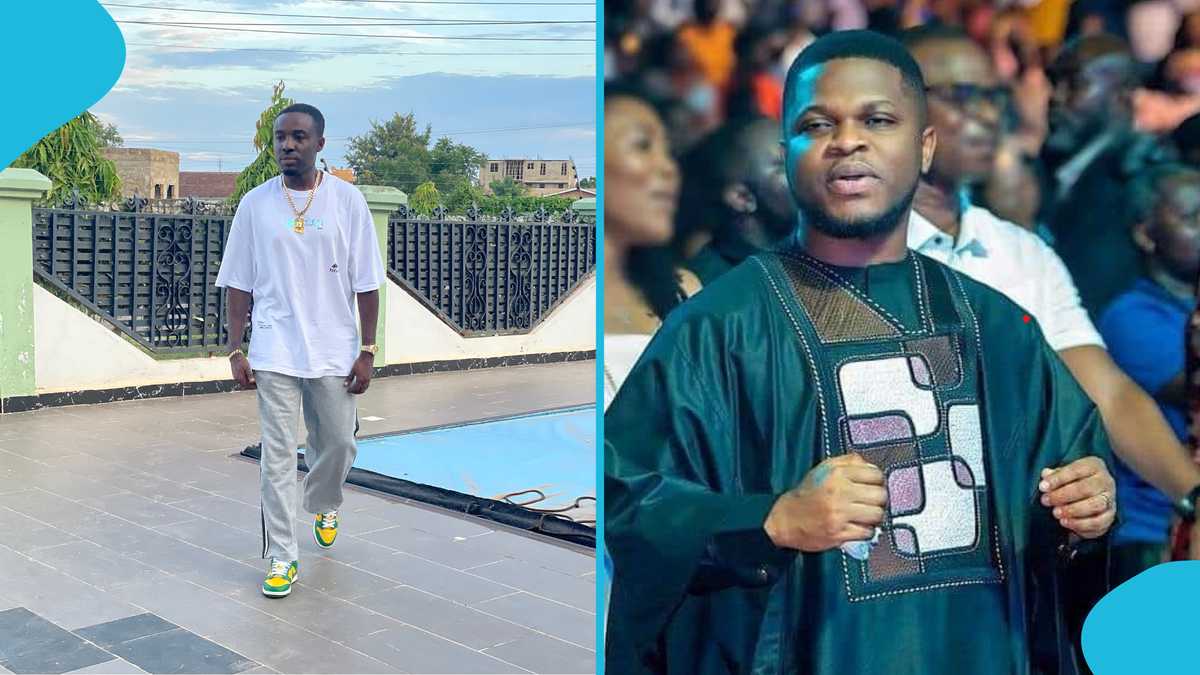
Figure 2
Histopathological images of the patient: (A) basketweave hyperorthokeratosis, acanthosis and basal layer hyperpigmentation with multiple hair follicles, (B, C) dense diffuse perivascular, interstitial, perineural and periadnexal infiltrates composed of foamy histiocytes, lymphocytes, plasma cells, mast cells and multinucleated giant cells most prominent in the deep dermis to subcutaneous fat, (D) membranous fat changes in the subcutis, (E) CD68 staining of cells of interest, (F) S100 staining of cells of interest.
H syndrome is part of a disease spectrum known as histiocytosis-lymphadenopathy plus syndrome, along with three other conditions namely, pigmented hypertrichosis with insulin-dependent diabetes mellitus (PHID), Faisalabad histiocytosis and familial Rosai-Dorfman disease (RDD). Aside from sharing a genetic cause, these conditions have overlapping signs and symptoms, such as the presence of hyperpigmentation and histiocytosis on histopathology. PHID is differentiated from the others by the presence of insulin-dependent diabetes mellitus.4 Faisalabad histiocytosis typically presents with periorbital swelling,5 while the most common manifestation of familial RDD is cervical lymphadenopathy.6
Currently, the approach to the patient’s treatment is supportive and symptomatic. The patient was treated with Naproxen 275 mg two times per day to aid in analgesia as well as anti-inflammation, and she was also given iron supplementation to help correct the anaemia. She was started on hormone replacement therapy to address signs and symptoms of hypogonadism. Laser hair removal with long-pulsed 1064 nm neodymium-doped yttrium aluminium garnet (Nd:YAG) laser is being done every 4 weeks for hypertrichosis. The patient has been referred to appropriate subspecialty clinics including the genetics clinic for interpretation of genetic test results and counselling, and adolescent medicine for psychosocial support.
The patient has good compliance to medications and procedures with no adverse reactions reported. There is decreased pain and tenderness on bilateral lower extremities. The patient’s skin lesions, as well as the enlargement of the bilateral cheeks along with other symptoms, are being monitored as progression may be a sign of active inflammation. The mild sensorineural hearing loss will be monitored annually while hepatosplenomegaly, pleural and pericardial fibrosis will be monitored symptomatically, with referrals to appropriate subspecialties for co-management. Since management of H syndrome is symptomatic, other immunosuppressants such as methotrexate and IL-6 inhibitors may be used as needed.
H syndrome (OMIM #602782) is a rare autosomal recessive genodermatosis first coined in 2008 since most of the clinical features observed in affected patients start with the letter ‘H’.1 2 The disorder stems from mutations in the SLC29A3 gene which codes for the human equilibrative nucleoside transporter-3 (hENT3). This protein is responsible for the transport of nucleosides to organelles, and its dysfunction leads to inflammation and histiocyte proliferation in various tissues.7 The hallmark of H syndrome is its cutaneous manifestation of hyperpigmentation with induration and hypertrichosis, which is observed in 68% of the patients.1 These usually appear on the inner thighs and shins with classic sparing of the knees. On histopathology, the dermis and subcutaneous tissues are infiltrated primarily by CD68-positive histiocytes along with fibrosis, as observed in our patient. Other manifestations of H syndrome which are also observed in the patient include hearing loss, low height, symptoms of hypogonadism- amenorrhea and delayed development of secondary sexual characteristics and facial telangiectasias. Although not observed in the patient (figure 1F), H syndrome may also commonly manifest with valgus or flexion contractures. Some patients also present with swelling or masses in other parts of the body such as the scrotum.1 2 8 Enlargement and fibrosis of internal organs are also seen in our patient which manifested as hepatosplenomegaly, as well as pleural and pericardial thickening on CT scan. This is consistent with other case reports stating that pericardial involvement is the most common form of cardiac anomaly in H syndrome.2 9 Another form of fibrosis that has been reported in multiple cases is retroperitoneal fibrosis.7 10 A not-as-common presentation in H syndrome exhibited by the patient is the bilateral enlargement of the cheeks. In one case report, an 11-month boy exhibited signs and symptoms of H syndrome including hepatosplenomegaly, hyperpigmentation and hypertrichosis. The patient also exhibited a cheek lesion which showed histiocytosis with polymorphous infiltration positive for CD68 and S100 and negative for CD1a.11 Various haematological and laboratory abnormalities have been described in cases of H syndrome, including anaemia, low levels of insulin-like growth factor 1 levels, follicle-stimulating hormone and luteinising hormone compatible with prepubertal levels, as seen in our patient. Inflammatory markers such as ESR7 12 are often elevated in patients with H syndrome; however, normal levels in our patient may be due to the absence of frank acute inflammation. Insulin-dependent diabetes mellitus may also be the sole manifestation in some cases.13 Lastly, cases of H syndrome have also had hearing loss as a prominent feature, but as with the other clinical features of the syndrome, this would vary in presentation. Cases have been reported between mild to severe sensorineural hearing loss, with regular follow-ups recommended for audiological evaluation, both subjectively and objectively.14
Aside from the hyperpigmentation and hypertrichosis, the most prominent characteristic in our patient is the bilaterally enlarged cheeks. No previous cases have reported this unique presentation of bilateral cheek involvement, and we believe that the mechanism of developing such features is similar to that of the other skin changes, as the histopathological results corroborate. In an article by Shiloh et al15, the authors have proposed an intermediate pathway relating SLC29A3 mutation to the activation of the mitogen-activated protein kinase/extracellular signal-regulated kinase (MAPK/ERK pathway) via toll-like receptors (TLR7/8) leading to cytokine release (figure 3).15 We believe that this pathway has led to the inflammation and fibrosis of the skin and tissues of the face.
Figure 3
SLC29A3 mutation leads to dysfunction of human equilibrative nucleoside transporter-3 (hENT3) and activation of mitogen-activated protein kinase/extracellular signal-regulated kinase (MAPK/ERK) pathway. (1) After target cell phagocytosis by monocytes, dysfunctional hENT3 impairs transport of degraded nucleosides to the cytoplasm leading to accumulation in lysosomes. (2) Accumulation of nucleosides activatese TLR7/8. (3-4) Downstream pathway activates MEK and ERK. (5) Increased activity of phosphorylated ERK increases production of proinflammatory cytokines. (7a,7b) This mechanism leads to inflammation and fibrosis of the cheeks and skin. Adapted from Meyer, LK & Nichols, KE. Hyperactive TLR signalling: putting the “H” in H syndrome. Blood. 2023;142(20):1679–1681. doi:10.1182/blood.2023022381, with permission from Elsevier. Licence number: 5957900308759.
Although H syndrome may be diagnosed clinically, the definitive diagnosis is through genetic testing.16 The patient’s whole genome sequencing revealed a homozygous frameshift mutation variant in SLC29A3, Exon 6, c.1350_1354del (p.Val451Aspfs*103), a mutation that has also been observed in individuals with clinical features of SLC29A3-related conditions. However, as of this writing, the identified mutation is classified as a variant of uncertain significance, and its role in causing H syndrome remains inconclusive due to the rarity of both the condition and the specific mutation. Ideally, genetic testing of both parents and a sibling would have helped determine carrier status and provide further clarity, but this was not pursued due to financial limitations in a resource-poor setting such as the Philippines. Despite this, the clinical findings and diagnostic findings including histopathology are still consistent with the diagnosis of H syndrome.
The management of H syndrome is primarily symptomatic, and monitoring is warranted to detect other systemic manifestations of H syndrome early in their course. Nonsteroidal anti-inflammatory drugs have been shown to decrease the severity of symptoms.11 12 Immunosuppressants have been tried in the treatment of H syndrome, but among these, IL-6 receptor inhibitors such as tocilizumab showed the most promising response in terms of normalising levels of inflammatory markers and improving skin lesions, among others.3 7 17 Recently, molecular targeted therapies have also been used off-label, and among them, mitogen-activated extracellular signal-regulated kinase (MEK) inhibitor trametinib has shown efficacy in controlling histiocytic infiltration and systemic inflammatory manifestations through interruption of the aforementioned MAPK/ERK pathway.15 Lastly, laser procedures for hair removal have been shown to address hypertrichosis permanently.16
The following experiences, thoughts and sentiments of our patient and her mother are translations.
Mother:
I was often frustrated over my daughter’s condition at the time when her previous consultations in our locale yielded no answers. I would take her to the hospitals where tests would be ordered, but nothing definitive would be said about the results, and no prescriptions would be given to help heal her. I was sorrowful at the thought of her succumbing to this illness, so we later decided to come here for treatment, and we were eventually referred to Dermatology through Otorhinolaryngology and Pediatrics.
According to her doctors, H syndrome affects hearing, her lower extremities, hormones, height and other things that begin with the letter ‘H’. From my understanding, H syndrome is so rare that only a few people in the world have it. I have never heard of this disease before, and that terrified me. People always ask me what she has, and this is what I tell them.
I have not quite accepted the fact that she has this condition. As a parent, I want to find a cure for my child or at least to control her illness, so that she can lead a normal life, get good education, and secure stable employment. She finds it difficult living with this disease. Although she has grown accustomed to it, she sometimes hides behind me when we leave our house, because people stare and gossip. I often worry about how she will be, particularly when her father and I are gone. Who will guide her and take care of her? Thankfully, her vital organs are not involved thus far, and her skin has smoothened, lightened, and is much less warm and painful.
I still cannot fully comprehend her illness, but what I know is that I am happy now that she is taking medications and undergoing laser treatment. During our follow-up visits, we see that she is improving overall through close monitoring. We have almost given up seeking medical attention before, but I am glad that we did not.
Patient:
I feel embarrassed and self-conscious of my face and legs. I just do not want others to see me. I am scared to fail due to my frequent absences from school. I am anxious that I might not be able to go to college because of my condition. I do not think I can commute to school alone; I want my mother with me. Please help me continue to get better. I want my cheeks to become smaller, and the skin on my legs to become lighter and smoother. The laser treatment can sometimes be uncomfortable, but I can and will brave the discomfort. I am also in less pain on my lower extremities compared with before. I am no longer as saddened by my illness. I just live my life playing with friends and watching anime. I have accepted my fate.
Consent obtained from parent(s)/guardian(s).