Lipids in Health and Disease volume 24, Article number: 127 (2025) Cite this article
Infertility is a multifaceted condition influenced by metabolic and biochemical factors. Uric acid (UA) and high-density lipoprotein cholesterol (HDL-C) may individually affect reproductive health. The UA-to-HDL-C ratio (UHR), an emerging indicator of chronic inflammation and metabolic status, may be associated with infertility because of its connections to metabolic disorders, disrupted reproductive processes, and other related factors. Nevertheless, evidence of the relationship between the UHR and infertility remains limited and controversial. Therefore, potential associations were analyzed in this study.
In this cross-sectional study, data from the 2013–2020 National Health and Nutrition Examination Survey (NHANES) were utilized, a nationally representative survey assessing the health and nutritional status of the U.S. population. Female participants aged 18–45 years (n = 6502) whose infertility status was determined through self-reported responses to reproductive health questions were included. The primary outcome was infertility, defined on the basis of responses indicating difficulty in conceiving over the past year. Between-group differences were analyzed via Student’s t test or the Mann‒Whitney U test for continuous variables or the chi-square test for categorical data. The independent association between infertility status and the log UHR was assessed by log computes logarithms by default natural logarithms. Subgroup analyses were performed to assess the strength of the results.
The mean log UHR of the women in the infertility group was significantly greater than that of the women in the noninfertility group (5.34 vs. 5.22, P < 0.001). Adjusted analyses revealed that an increase in the log UHR was associated with greater odds of infertility (odds ratio (OR) = 1.830, 95% confidence interval (CI) 1.396–2.401). Subgroup analysis revealed that women younger than 35 years with an elevated log UHR faced an even greater risk of infertility (OR = 2.716, 95% CI 1.784–4.162; P < 0.001).
An elevated UHR is associated with a higher risk of infertility, and this knowledge may be beneficial for developing a nonpharmacological intervention for improving fertility outcomes. Further research is needed to clarify the direct impact of the UHR on female infertility, which could inform future strategies for prevention and treatment.
Infertility is defined as the inability to conceive during childbearing years, despite having regular, unprotected intercourse for at least 12 months. Infertility has emerged as a substantial public health challenge that impacts approximately 8 to 15% of couples in their reproductive years worldwide, resulting in substantial emotional and economic burdens [1, 2]. Recent research highlights the role of metabolic imbalances as contributors to infertility, and there has been particular interest in the uric acid (UA)-to-high-density lipoprotein cholesterol (HDL-C) ratio (UHR); the UHR may provide insight into reproductive health, as it reflects both inflammatory and metabolic status. Managing metabolic health in infertile women presents unique challenges; despite the increasing awareness of these factors, comprehensive biomarkers that integrate metabolic and inflammatory status to guide diagnosis and treatment strategies are lacking.
The UHR involves a combination of inflammatory and metabolic status indicators, reflecting the combined effect of UA and HDL-C levels on reproductive health. A high UHR may increase the risk of infertility, especially in cases linked to metabolic and inflammatory imbalances. On the one hand, UA, a metabolite from purine breakdown, is linked to metabolic syndrome and recognized as an inflammatory marker that is potentially disruptive to reproductive functions. Studies suggest that elevated UA levels may increase the risk of poor ovarian response and infertility, likely through oxidative stress, inflammation, and endothelial dysfunction [3]. On the other hand, HDL-C plays an important role in lipid metabolism and cardiovascular health while significantly influencing reproductive outcomes. Clinical studies indicate that lower HDL-C levels increase infertility risk through multiple mechanisms, specifically by regulating reproductive hormonal balance, endometrial receptivity, and ovarian function [4,5,6].
The UHR has emerged as a promising marker with superior evaluative capabilities in individuals with conditions such as metabolic syndrome, coronary artery disease, hypertension [7,8,9,10,11], age-related diseases, and mortality across diverse populations, highlighting its potential in clinical risk assessment and management [12,13,14,15]; additionally, the UHR may provide a more comprehensive understanding of metabolic status and its potential influence on reproductive function. In particular, a high ratio could suggest an imbalance in oxidative stress and lipid metabolism, which might interfere with the complex processes involved in conception and pregnancy. For example, the ratio could indicate that hormonal regulation, ovarian function, and endometrial quality are atypical. Although the potential of the UHR in evaluating metabolic status is well documented, its role as a predictive tool for infertility remains unclear. The focus of research has been primarily on the individual effects of UA and HDL-C levels on reproductive health, and the UHR in infertile populations has been specifically investigated in only a few studies. This gap underscores the need for further exploration of the clinical relevance of the UHR in female infertility.
The hypothesis of this study was that an elevated log UHR is linked to a greater risk of infertility in women. Therefore, this study was performed on the basis of 2013–2020 National Health and Nutrition Examination Survey (NHANES) data. Understanding the relationships among UA levels, HDL-C levels, and infertility could pave the way for the development of novel diagnostic and therapeutic approaches for couples struggling with infertility.
In this study, data from the NHANES, a nationally representative cross-sectional survey conducted by the National Center for Health Statistics (NCHS), were utilized. The NHANES uses a multistage probability sampling design to evaluate the health and nutritional status of the noninstitutionalized population in the United States. A cross-sectional design was chosen for its efficiency in capturing health-related variables and associations at a specific time point, making it ideal for analyzing large-scale population datasets such as the NHANES population. Unlike longitudinal studies, which track participants over time to explore trends or causality, cross-sectional studies provide a cost-effective and timely approach to identifying associations. All NHANES protocols were approved by the NCHS Research Ethics Review Board, and written informed consent was obtained from all participants.
Female participants aged 18–45 years from the 2013–2020 NHANES cycles (n = 6502) were initially included. Participants with missing data on infertility status (n = 978), HDL-C levels (n = 327), UA levels (n = 17), or other key covariates (n = 1009) were excluded; the remaining participants composed the final sample for analysis.
Fasting blood samples were used to measure UA and HDL-C levels. The log-transformed UHR (log UHR) [16] was calculated by dividing the natural logarithm of UA (µmol/L) by that of HDL-C (mmol/L).
Infertility status was assessed with a reproductive health questionnaire. The participants were classified as infertile if they answered “yes” to the following question: “Have you tried to become pregnant for at least a year without becoming pregnant?”
The following covariates [7, 8] were selected on the basis of their potential to influence the relationship between the log UHR and infertility risk: age (< 35 years, ≥ 35 years); race/ethnicity (non-Hispanic white, non-Hispanic black, Mexican-American, other); marital status (married, other); educational level (below high school, high school, above high school); lifestyle factors, including smoking status (never, former, current) and alcohol consumption status (never, former, current); anthropometric variables, including body mass index (BMI; <25, 25–30, ≥ 30 kg/m²); and clinical indicators, including hypertension status (yes, no), diabetes status (yes, no), alanine aminotransferase (ALT) levels, aspartate aminotransferase (AST) levels, creatinine levels, and blood urea nitrogen levels.
The participants were divided into infertile and fertile groups. The Shapiro‒Wilk test was conducted to assess the normality of the continuous variables. Continuous variables are expressed as the means ± standard deviations (SDs) and were analyzed via Student’s t test or the Mann–Whitney U test. Variables that did not meet normality assumptions are presented as medians with interquartile ranges. Categorical variables are expressed as percentages and were analyzed via the chi-square test. The independent association between the log UHR and infertility risk was assessed through multivariable logistic regression models. Multicollinearity among independent variables was assessed using variance inflation factor (VIF) analysis. A threshold of VIF < 10 was used to indicate the absence of significant multicollinearity. All the variables in the model demonstrated VIF values well below this threshold, confirming the robustness of the regression analysis. The crude model was unadjusted; Model 1 was adjusted for age, race, marital status, educational level, and BMI; and Model 2 was further adjusted for smoking status, alcohol consumption status, hypertension status, diabetes status, ALT levels, AST levels, creatinine levels, total cholesterol levels and blood urea nitrogen levels. The log UHR was analyzed as both a continuous variable and a categorical variable (quartiles, a statistical method of dividing data into four equal parts, which not only facilitates the analysis of continuous variables but also provides a clearer perspective for identifying patterns and trends) [17, 18]. Considering that clinical indicators and outcomes are usually not simple linear relationships, restricted cubic spline (RCS) analysis [19, 20], a segmented polynomial method, was used to assess nonlinear relationships between the log UHR and infertility risk. This approach ensures the smoothness of the curve, making the data fit closer to the true association curve, which is better suited to improving predictive performance. Subgroup analyses and interaction tests were conducted to explore the effects of covariates on the associations. All analyses were performed via R version 4.3.1, with P < 0.05 (two-tailed) considered to indicate statistical significance.
In total, 4171 participants were included in the analysis, 3621 of whom were categorized as fertile and 550 of whom were categorized as infertile on the basis of their responses to the reproductive health questionnaire (Fig. 1). The baseline characteristics of the two groups are summarized in Table 1. Significant differences between the infertile and fertile groups were observed across multiple variables. The women in the infertility group were, on average, older (36 vs. 33 years, P < 0.001) and had higher rates of smoking, obesity, hypertension, and diabetes (P < 0.001 for all). Additionally, infertile participants had elevated levels of UA (P < 0.001) and total cholesterol (P = 0.026), along with reduced HDL-C levels (P < 0.001). The log UHR values were notably higher in the infertility group than in the noninfertility group (P < 0.001). These findings suggest that metabolic and demographic factors differ significantly between women with and women without infertility, highlighting the potential relevance of the log UHR as a biomarker.
Furthermore, variables such as race, educational level, alcohol consumption status, and ALT, AST, creatinine, and blood urea nitrogen levels were not significantly different between the groups (P > 0.05).
The VIF analysis indicated no significant multicollinearity among the independent variables, with all values being less than 10. The association between the log UHR and infertility risk was assessed via multiple logistic regression analysis. As shown in Table 2, the log UHR was significantly positively correlated with infertility risk across all the models.
According to the crude model, the odds ratio (OR) was 2.048 (95% confidence interval (CI): 1.642–2.557, P < 0.001), indicating a strong association. After adjusting for age, race, marital status, educational level, and BMI in Model 1, the positive relationship remained significant (OR = 1.854, 95% CI: 1.432–2.405, P < 0.001). Model 2 was further adjusted for smoking status, alcohol consumption status, hypertension status, diabetes status, alanine aminotransferase (ALT) levels, aspartate aminotransferase (AST) levels, creatinine levels, total cholesterol levels, and blood urea nitrogen levels (OR = 1.830, 95% CI: 1.396–2.401, P < 0.001).
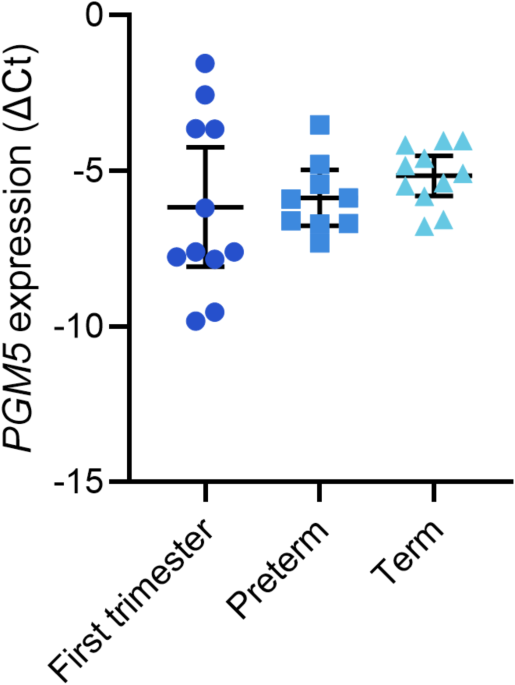
When the log UHR was categorized into quartiles, participants with a UHR in the highest quartile presented a greater risk of infertility than did those with a UHR in the lowest quartile according to fully adjusted Model 2 (OR = 1.701, 95% CI: 1.246–2.331, P < 0.001). This consistent association was further supported by RCS analysis, which revealed a linear increase in infertility risk as the log UHR increased (Fig. 2). These findings suggest that a higher log UHR is independently associated with an increased risk of infertility. Early identification of elevated log UHR levels in women undergoing fertility treatments could facilitate the provision of timely and targeted interventions.
Subgroup analyses were performed to evaluate the consistency of the association between the log UHR and infertility across various demographic and clinical subgroups (Table 3). Interaction tests were conducted to determine whether the relationship between the log UHR and infertility risk was influenced by covariates.
The results indicated that age significantly modified the association (P < 0.001). Among women younger than 35 years, the relationship was notably stronger, with an OR of 2.716 (95% CI: 1.784–4.162), indicating an increased risk of infertility in this group. This suggests that younger women with higher log UHR values may represent a particularly vulnerable population, potentially requiring targeted interventions.
The absence of significant interactions for covariates such as race, marital status, educational level, smoking status, alcohol consumption status, BMI, hypertension status, and diabetes status (P > 0.05) suggests that the association between the log UHR and infertility risk remains consistent across these diverse subgroups. However, the association appeared slightly more pronounced among non-Hispanic white and black women, married individuals, individuals with higher educational levels, current smokers and drinkers, individuals with a BMI of either < 25 kg/m2 or ≥ 30 kg/m2, and individuals without hypertension or diabetes. However, the lack of statistical significance suggests that these variations were not substantial enough to modify the overall relationship.
These findings suggest that the log UHR is a robust marker of infertility risk across diverse subgroups, with age being a significant modifier. The stronger association observed in younger women underscores the need for early identification and management of metabolic and lipid-related risks in this population to mitigate infertility risk effectively.
In this cross-sectional study, it was found that women with infertility had significantly higher log UHR values than those without infertility. Multivariate regression analyses demonstrated a consistent positive association between the log UHR and infertility risk, with a linear trend indicating that a higher log UHR was linked to an increased risk of infertility. These findings highlight the potential of the log UHR as a marker for infertility risk, underscoring the importance of metabolic health management in reproductive planning.
Female infertility is a condition with a complex etiology and is influenced by multiple biological mechanisms and pathways. Notably, female fertility is highly dependent on the successful regulation of energy metabolism. Metabolic disturbances have clinically important consequences for human reproduction [21].
Compared with the evaluation of HDL-C and UA levels separately, the UHR has superior evaluative capabilities and is a recently proposed novel index of metabolism and inflammation, such as that observed in individuals with metabolic syndrome, type 2 diabetes mellitus, Hashimoto’s thyroiditis, coronary artery disease, and hypertension [7,8,9,10,11]. This is the only study in which indirect evidence of a connection was obtained. The association between the UHR and infertility can be attributed to its reflection of underlying disruptions in oxidative stress and lipid metabolism, both of which are critical to reproductive function. The study revealed a significant association between an elevated log UHR and an increased risk of infertility, suggesting that an imbalance in oxidative stress and lipid metabolism may contribute to impaired fertility. The two major components of the UHR, namely, UA and HDL-C levels, may be involved in the pathophysiological mechanisms related to infertility.
These results suggest that the log UHR is positively related to infertility, indicating that lowering the log UHR may help decrease the risk of infertility. It was hypothesized that the mechanism by which a higher UHR increases the risk of infertility may be related to the following two factors.
On the one hand, UA, as both an antioxidant and a pro-oxidant, may contribute to female reproductive disorders through mechanisms such as oxidative stress, inflammation, and mitochondrial dysfunction [22,23,24]. High UA levels can increase reactive oxygen species (ROS) production, activate inflammatory pathways such as the MCP-1 and NF-κB pathways, damage reproductive tissues, and impair follicular development and sperm quality [25, 26]. Elevated UA levels are also linked to chronic low-grade inflammation, which is associated with infertility risk, particularly in individuals with conditions such as polycystic ovary syndrome (PCOS), for whom elevated UA levels contribute to insulin resistance and anovulatory infertility [27,28,29]. The study revealed that UA and total cholesterol levels were higher in infertile women than in noninfertile women, which is consistent with the findings of previous studies. However, while these associations are being explored, the direct effect of UA levels on female fertility remains to be fully elucidated.
On the other hand, research has shown that disrupted HDL-C metabolism negatively impacts female fertility. HDL-C is the only lipoprotein found in significant amounts in follicular fluid, and its size and composition are linked to embryo quality. Cholesterol accumulation within cells can affect oocyte viability by altering calcium channels and disrupting cell survival pathways [30]. Additionally, HDL-C may influence fertility through its effects on hormonal balance, particularly by interacting with sex hormone-binding globulin (SHBG) and affecting hormone availability [31]. Miettinen reported that SR-BI knockout mice with abnormal HDL-C levels were infertile [32], whereas Zhuang et al. [33] linked increased visceral fat to infertility risk. However, Zhu et al. [34] reported no significant association between HDL-C levels and female infertility risk on the basis of genetic data from two large databases. While some studies suggest a lack of a significant association between HDL-C levels and infertility risk, these findings show lower HDL-C levels in infertile women, supporting the hypothesis that metabolic changes, including those in HDL-C metabolism, can impair reproductive health.
Overall, elevated UA levels contribute to oxidative stress, damage oocyte DNA, impair oocyte quality, reduce fertilization rates, and compromise embryo development. Oxidative stress also disrupts folliculogenesis, hormonal balance, and endometrial receptivity by altering key implantation proteins such as integrins and cytokines. Low HDL-C levels diminish the effects of oxidative stress and inflammation, exacerbating UA-induced oxidative damage. The UHR integrates these factors, with a high UHR reflecting oxidative stress and disrupted lipid metabolism. This imbalance creates an unfavorable environment for fertility, affecting egg quality, ovarian function, and uterine receptivity, ultimately hindering conception and pregnancy.
By identifying individuals with high UHR, doctors may be able to detect early signs of metabolic disturbances and oxidative stress, enabling the use of more targeted interventions to improve fertility outcomes. Potential therapeutic approaches might include antioxidant supplementation, lifestyle modifications (such as diet and exercise), and pharmacological treatments to normalize lipid metabolism and reduce oxidative damage.
The present study revealed a significant association between the log UHR and infertility risk. These findings align with the hypothesis that metabolic alterations may adversely affect reproductive capabilities. The log UHR could be integrated into infertility management protocols as a routine screening marker, particularly for women with concurrent metabolic or immune abnormalities. Early identification of women with elevated log UHR levels and regular monitoring of changes in the log UHR in women undergoing fertility treatments may enable timely interventions, including nonpharmacological approaches such as lifestyle modifications, dietary adjustments, and physical activity, to optimize metabolic health and improve pregnancy outcomes. Future research should prioritize exploring the predictive value of the log UHR across diverse populations, the correlation of the UHR with various infertility symptoms, the long-term effects of an elevated log UHR, the underlying mechanisms linking the UHR to infertility, and the potential benefits of metabolic-targeted interventions. This approach provides a more comprehensive understanding of its clinical significance and utility.
Longitudinal studies with larger sample sizes and more comprehensive assessments of confounding factors could provide more definitive answers. Additionally, understanding the underlying relationships by which the log UHR influences infertility could lead to the development of novel therapeutic strategies for infertility treatment and the establishment of evidence-based guidelines for managing UHR in the context of reproductive health.
This study has several strengths. First, its objectivity and credibility were ensured by the use of data from the NHANES, a nationally representative survey conducted with standardized protocols. Second, the inclusion of multiple covariates helped reduce potential sources of confounding, thereby enhancing the robustness of the findings. Finally, the large, nationally representative sample size further increased the reliability and generalizability of the results.
A limitation of the study is that the cross-sectional approach prevents the establishment of causality [35], and the retrospective nature of the questionnaire may lead to inaccuracies in self-reported data. Reliance on self-reported infertility data can lead to biases such as recall bias, where participants may misremember or underreport their infertility history, and social desirability bias, where stigma surrounding infertility might result in incomplete or misleading responses. Additionally, heterogeneous interpretations of infertility by respondents could lead to inconsistencies in clinical definitions. Moreover, the absence of male-specific information in the questionnaire introduces the potential for unaccounted confounding factors related to male infertility. Another limitation is the relatively small sample size, which may limit the generalizability of the findings to the broader population. While an association between the log UHR and infertility risk was identified in this study, the underlying mechanisms remain unclear. In future studies, researchers should include larger and more diverse cohorts and use longitudinal or experimental designs to gain a deeper understanding of these relationships.
An elevated log UHR is significantly associated with an increased risk of infertility in women, highlighting the critical link between metabolic health and reproductive outcomes, which is consistent with the hypothesis. The log UHR could serve as a valuable biomarker for identifying women at greater risk of infertility and may be beneficial for developing early intervention and personalized care strategies for improving fertility outcomes.
The findings suggest that UHR can enhance fertility treatment by guiding interventions, improving patient outcomes, and optimizing reproductive health management. Integrating UHR into clinical practice may directly impact patient care and fertility success. In summary, the UHR is a promising biomarker and therapeutic target for improving reproductive health outcomes.
No datasets were generated or analysed during the current study.
- NHANES:
-
National Health and Nutrition Examination Survey
- NCHS:
-
National Center for Health Statistics
- BMI:
-
Body Mass Index
- ALT:
-
Aspartate aminotransferase
- AST:
-
Alanine aminotransferase
- UA:
-
Uric Acid
- HDL-C:
-
High-Density Lipoprotein Cholesterol
- UHR:
-
Uric acid-to-High-density lipoprotein cholesterol Ratio
- OR:
-
Odds Ratio
- CI:
-
Confidence Interval
- ROS:
-
Reactive Oxygen Species
- MCP-1:
-
Monocyte Chemotactic Protein-1
- NF-κB:
-
Nuclear Factor kappa B
- SHBG:
-
Sex Hormone-Binding Globulin
- KO:
-
Knockout
- VATA:
-
Visceral Adipose Tissue Area
- MVP:
-
Million Veteran Program
- GLGC:
-
Global Lipids Genetics Consortium
- IVW:
-
Inverse Variance-Weighted
We extend our gratitude to the NHANES database for offering their platform and providing valuable datasets that made this research possible.
This study was supported by the General Program sponsored by the Basic Research Fund of the Shenzhen Natural Science Foundation (No. JCYJ20230807110317036), the Clinical Medicine Research “735 Plan” in 2024, and the Seventh Affiliated Hospital, Sun Yat-sen University (No. ZSQY202473524).
This study utilized publicly available data, with informed consent obtained from all participants by the original data collectors. As the analysis was conducted on deidentified data, there were no direct ethical implications. All procedures adhered to the relevant guidelines and regulations to ensure the integrity and ethical compliance of the research.
Not applicable.
The authors declare no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Kong, Y., Lin, M., Fu, Y. et al. Elevated log uric acid-to-high-density lipoprotein cholesterol ratio (UHR) as a predictor of increased female infertility risk: insights from the NHANES 2013–2020. Lipids Health Dis 24, 127 (2025). https://doi.org/10.1186/s12944-025-02521-w