BMC Gastroenterology volume 25, Article number: 197 (2025) Cite this article
Gallstones are a common disease of the digestive system, and its complications pose serious risks to human health and impose a significant economic burden on society. Inadequate dietary potassium intake may be associated with the development of gallstones, however, there is a lack of current epidemiological research on this topic.
The purpose of this research was a preliminarily exploration of the relationship between dietary potassium intake and the prevalence of gallstones, providing direction for the next step of quantitativeanalysis on the association between dietary potassium intake and the prevalence of gallstones.
Data from the National Health and Nutrition Examination Survey (NHANES) spanning 2017 to 2020 were used for a cross-sectional analysis. The presence of gallstones was assessed based on the NHANES questionnaire data for the corresponding time frame. To investigate the link between dietary potassium consumption and the likelihood of developing gallstones, multiple logistic regression models were used. Subgroup analyses were conducted based on variables such as age, gender, poverty-to-income ratio (PIR), body mass index (BMI), hypertension, diabetes, dietary supplement use, and physical activity. An analysis of linear associations was carried out using smoothing curves.
The study comprised 6,223 participants aged 20 years and older, excluding pregnant individuals. Among these participants, 671 were diagnosed with gallstones. In the final adjusted model, with a 95% confidence interval (CI) of 0.70 to 0.93, it was determined that dietary potassium intake and gallstone incidence were negatively correlated (OR = 0.81, p = 0.003). Individuals in the highest tertile of dietary potassium intake experienced a 31% lower risk of developing gallstones compare to those in the lowest tertile (OR = 0.69, 95% CI: 0.51–0.94, p = 0.017). In Model 1, the prevalence of gallstones exhibited an inverse relationship with dietary potassium intake. This negative association persisted even after stratifying by variables such as age, gender, PIR, BMI, hypertension, diabetes, dietary supplement use, and physical activity. Sensitivity analyses demonstrated the stability of this relationship.
Our research revealed that increased dietary potassium intake is associated with a lower prevalence of gallstones. Nevertheless, additional prospective studies are required to confirm a precise dietary potassium intake level and the long-term effects of potassium metabolism on gallstone formation.
Gallstones typically develop within the gallbladder or bile ducts [1]. They are categorized into three primary types: cholesterol stones, bilirubin stones, and mixed stones. Among these, cholesterol stonesand those are classified as mixed stones [2]. Gallstones, which may present as either asymptomatic or symptomatic, are chemically classified into two main types: common cholesterol stones and bilirubin (pigment) stones. Black pigment stones are associated with chronic hemolysis, while brown pigment stones are linked to obstructed or infected bile ducts. The majority of gallstones (80–90%) that form in the gallbladder primarily consist of cholesterol (70%), embedded within a matrix of bile pigments, calcium salts, and glycoproteins [3]. In addition to pure and mixed cholesterol stones, pure pigment stones are also identified. Brown pigment stones are associated with biliary tract infections (bacterial and helminthic deconjugation of bilirubin glucuronides) and are more prevalent in Asia. Black pigment stones, which mainly consist of calcium bilirubinate, are found in conditions such as hemolytic anemia, ineffective hematopoiesis, and in patients with cystic fibrosis [4]. The increased enterohepatic cycling of bilirubin is believed to be the cause of black pigment stones [5], a phenomenon also observed in patients with ileal dysfunction, consistent with the finding of elevated bilirubin levels in bile in patients with active ileal Crohn's disease or following ileal resection [6,7,8,9]. However, in patients with bile salt malabsorption, other factors leading to biliary cholesterol supersaturation [9,10,11] may more likely promote the formation of cholesterol gallstones. Gallstones are a prevalent condition, with particularly high incidences rates among American Indians, where the prevalence can reach up to 60–70%. In contrast, among White adults in developed countries, the prevalence ranges from 10 to 15% [12]. Gallstones pose a substantial burden on healthcare systems, a challenge anticipated to escalate with an aging and high-risk population [13]. In the United States (US), gallstone disease is the most frequently diagnosed hospitalized condition among gastrointestinal and liver diseases [14]. The majority of individuals with gallstones remain asymptomatic throughout their lives, yet approximately 10 percent of patients will eventually develop symptoms [15]. Complications associated with gallstones, such as cholecystitis, acute suppurative cholangitis, and pancreatitis, impact between 20 and 40% of individuals diagnosed with gallstones [16]. However, approximately 1–2% of these patients experience complications necessitating surgical intervention annually [17]. Furthermore, the presence of gallstones elevates the risk of gallbladder cancer(GBC), a condition typically associated with a poor prognosis [18]. GBC is the most common malignancy of the biliary tract, representing 80–95% of biliary tract cancers worldwide [19, 20]. Although relatively uncommon, it ranks sixth among all gastrointestinal malignancies. In 2019, an estimated 12,360 new cases were diagnosed, and 3,960 patients died from GBC and other biliary cancer in the United States [21]. Because of the insidious onset, rapid progression, and early asymptomatic characteristics of GBC, diagnosis is usually not made until intraoperative and postoperative pathological examinations, when the disease is already in moderate and advanced stages, and the therapeutic effect are poor [22]. Indeed, the overall mean survival rate for patients with gallbladder cancer is 6 months, with a 5-year survival rate of 5% [23]. Gallstones have traditionally been regarded as an etiological factor for gallbladder cancer according to case–control studies or autopsy studies [20, 24,25,26,27,28]. Most patients with gallbladder cancer have gallstones, and gallbladder cancer rates are well correlated with the prevalence of gallstones disease [20, 28]. In support of this association, an inverse correlation between cholecystectomy for gallstones and gallbladder cancer rates has been described [29]. Convincing evidence also exists for the presence of gallstones as a strongly associated factor for gallbladder cancer etiology [30]. It incurs direct costs amounting to $6.5 billion, and the associated expenditures have been escalating rapidly [31]. Consequently, the identification of reliable and well-controlled clinical indicators is crucial for predicting or preventing the development of gallstones.
Potassium has been recognized as one of the four primary nutrients frequently deficient in the American diet [32]. The recommended intake for potassium was substantially elevated in 2004, when theadequate intake level was established at 4,700 mg per day [33]. Achieving this intake level presents a significant challenge for the majority of Americans. Data from the 2003–2006 NHANES showed that just 3% of Americans achieved the recommended intake levels for potassium [34]. Insufficient dietary intake of potassium has been linked to the onset of various diseases affecting multiple bodily systems, including hypertension, diabetes, stroke, cardiovascular disease, osteoporosis, kidney disease, and non-alcoholic fatty liver disease [35, 36]. Higher potassium intake is associated with a reduced risk of kidney stones [37] and negatively correlated with their recurrence [38, 39]. Recent studies have explored the relationship between dietary minerals(magnesium, copper, iron, cobalt, calcium, zinc.) and gallstones [40,41,42,43,44,45].
Previous research has not explicitly examined the association between dietary potassium intake and the formation of gallstones. Addressing this gap, this study aims to utilize data from the NHANES to assess whether differences in potassium intake exist between individuals with gallstones and those without.
The National Health and Nutrition Examination Survey (NHANES), conducted periodically by the National Center for Health Statistics (NCHS) is an extensive, nationwide survey aimed at evaluating thehealth and nutritional status of Americans of all ages. A population-based survey aimed at both adult and child populations all over the country is scrupulously conceived and intends to obtain reflective data. The survey implements a strong and all-encompassing method, involving health discussions with respondents in their homes, health examinations at mobile health units, and a comprehensive collection of demographic details. The survey includes involves physical examinations, lab tests, health surveys, and chronicles of prescribed medications. This complex methodology ensures a complete assessment of a variety of health dimensions, thereby granting a thorough comprehension of participants'health conditions. The NHANES survey has been endorsed by the Institutional Review Board of the National Center for Health Statistics, with all participants having voluntarily provided their informed consent. NHANES statistical datasets are regularly issued biennially; however, the start of the coronavirus (COVID-19) pandemic in 2019 led to a temporary suspension of the program in March 2020. As a result, information gathered from 2019 up to March 2020 was combined with the 2017–2018 NHANES period to form a sample that is representative of the nation, encompassing pre-pandemic data from NHANES 2017 to March 2020. During this research period, specific inquiries were conducted regarding the past medical history of gallstones.
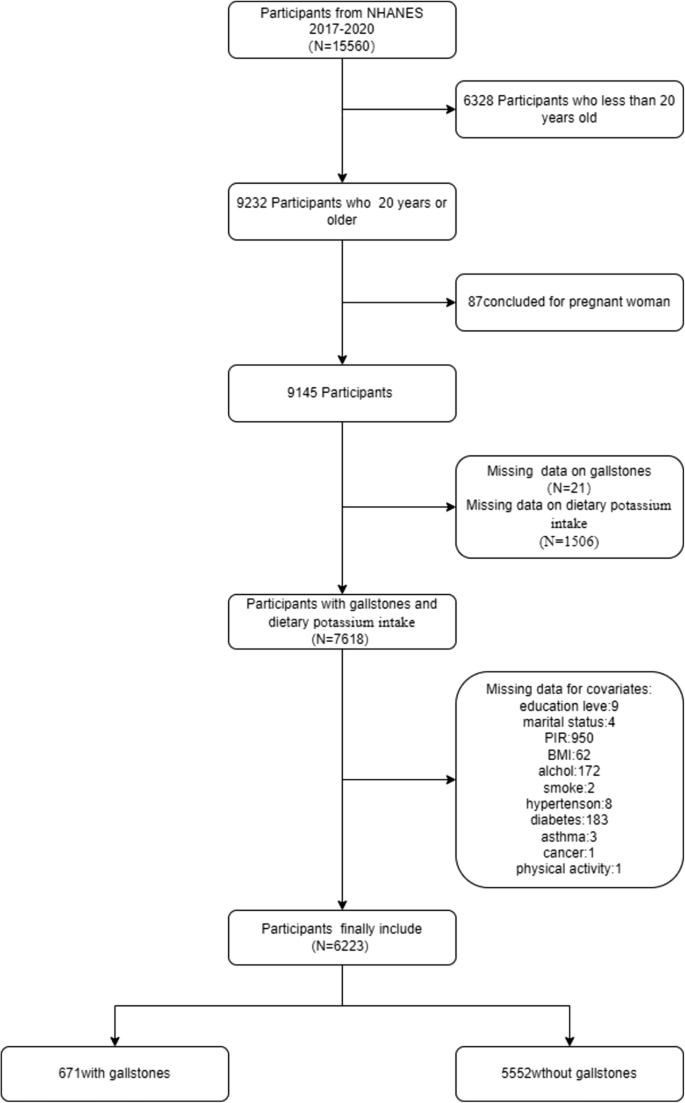
At the outset, this cross-sectional study enrolled 15,560 participants. From this study group, individuals aged 20 years and older (N = 9,232) who completed an interview were included in our analysis. Weexcluded pregnant women (N = 87) and individuals with missing information on gallstones (N = 21), dietary potassium intake (N = 1,506), or covariates (total N = 1,395), which included education level (N = 9), marital status (N = 4), PIR (N = 950), BMI (N = 62), alcohol consumption (N = 172), smoking status (N = 3), diabetes (N = 183), hypertension (N = 8), asthma (N = 3), cancer (N = 1), and physical activity (N = 1). Ultimately,6,223 individuals were included in the final analysis (Fig. 1).
Flowchart of the study. NHANES 2017–2020 enrolled 15,560 participants. Of these,6223 were retained after fulfilling inclusion and exclusion criteria
We identified the presence of gallstones in participants by analyzing their responses to the survey question,"Has a doctor ever diagnosed you with gallstones?". Participants who answered affirmatively were considered to have gallstones, and those who answered negatively were considered not to have gallstones. This method is straightforward and has been utilized in previous research [46, 47].
A multi-faceted approach was implemented to collect data on potassium intake from food and beverages using 24-h dietary recalls. This participant-driven method ensures the accurate collection of data on all food and drink items consumed by an individual within a 24-h period, from one midnight to the next. Each participant was required to complete two 24-h dietary recalls. The first recall was conducted through a face-to-face interview with a researcher at a mobile examination unit, and the second recall was conducted over the phone,3 to 10 days after the first recall [48]. Given that some participants regularly consumed potassium-containing supplements, their intake from these sources was included in their total potassium intake. For participants who completed two 24-h dietary recalls, the average potassium intake from both recalls was calculated and used. In cases where only one 24-h dietary recall was available, the data from that recall were utilized.
In this investigation, we incorporated various potential confounders as adjustment variables, encompassing factors such as age, gender, race, educational level, marital status, the family income-to-poverty ratio (PIR), body mass index (BMI), alcohol consumption, smoking status, diabetes, hypertension, use of dietary supplements, asthma, cancer, physical activity, and dietary information. Race was divided intofour distinct groups: Mexican American, White (not of Hispanic origin), Black (not of Hispanic origin), and Other Ethnicities. Educational achievement was categorized into three levels: fewer than 9 years, between 9 and 12 years, and over 12 years. Marital status was classified into three categories: currently married or living with a partner, previously married (including widowed, divorced, or separated), and never married. The PIR was stratified into three levels: low (≤ 1.35), medium (1.35 to ≤ 3.5), and high (> 3.5) [49]. BMI was calculated by dividing body weight in kilograms by the square of height in meters and was categorized into three ranges: below 25, between 25 and 30, and 30 or above [50]. Participants who had smoked at least 100 cigarettes in their lifetime were identified as smokers [51]. The presence of a history of diabetes, high blood pressure, asthma, or cancer was assessed through a questionnaire survey (yes/no) [52]. Professional trainers linked participants' reports with pharmaceutical and dietary supplement databases to compile information on medications and dietary supplements consumed over the past 30 days [53]. Participants were considered physically active if they engaged in moderate or vigorous sports, fitness programs, or recreational activities for more than 10 min per week; otherwise, they were classified as inactive [53]. Nutritional data were collected through a 24-h dietary recall survey, including assessments of caloric intake (kcal), sugar (g), fat (g), carbohydrates (g), protein (g), water (g), cholesterol (mg), calcium (mg), iron (mg), zinc (mg), copper (mg), sodium (mg), and selenium (mcg). We calculated the mean nutrient intake for each individual across the initial and subsequent 24-h dietary recall periods. The nutritional data were reclassified into binary categories using the median value of the sample's distribution as the cutoff to distinguish between "lower" and "higher" intake levels [54]. Detailed measurements of these variables are accessible through the publicly available NHANES database.
Continuous variables were characterized by the mean (SD) or median (IQR), depending on the data distribution. Categorical variables were summarized as percentages (%). To evaluate differences between groups, one-way ANOVA was used for data that followed a normal distribution, while the Kruskal–Wallis test was applied for data with skewed distributions. Chi-squared tests were used for categorical variables. Logistic regression analyses were conducted to calculate odds ratios (ORs) and their 95% confidence intervals (95% CIs) to assess the relationship between dietary potassium intake and the risk of gallstones. Model 1 was unadjusted. Model 2 was adjusted for sociodemographic variables including age, gender, and ethnicity. Model 3 was further adjusted for a comprehensive range of factors, including age, gender, ethnicity, education level, marital status, PIR, BMI, alcohol consumption, smoking status, diabetes, hypertension, dietary supplement use, asthma, cancer, physical activity, total caloric intake, sugar intake, fat intake, carbohydrate intake, protein intake, water intake, cholesterol intake, and mineral intake (calcium, iron, zinc, copper, sodium, and selenium). To investigate the linear relationship, fitted smoothing curves were applied. Stratified subgroup analyses were performed to evaluate the interaction between dietary potassium intake and the risk of gallstones among participants categorized by age, sex, PIR, BMI, hypertension, diabetes mellitus, dietary supplement use, and physical activity levels. A p-value less than 0.05 was considered statistically significant. All analyses were performed using R software(version 4.3.2, http://www.R-project.org) and the Free Statistics software package (version 1.9.2; Beijing Free Clinical Medical Technology Co. Ltd.).
A total of 15,560 participants completed the interview, of whom 9,233 were aged 20 years and older. We excluded 87 pregnant women,1,506 individuals who lacked data on dietary potassium intake, and 21 individuals who lacked information on gallstones. Additionally, we excluded 1,395 participantsdue to missing data on covariates such as race, educational level, marital status, PIR, BMI, alcohol consumption, smoking status, asthma, cancer, hypertension, diabetes, and physical activity. Consequently, the final dataset for analysis comprised 6,223 participants from the NHANES 2017-March 2020 data. Figure 1 depicts the comprehensive process for inclusion and exclusion.
Table 1 illustrates the baseline demographics of the study group, categorized based on levels of potassium intake. The study sample comprised 6,223 participants, of whom 51.1% were female and 48.9% were male. Among the participants,671 individuals (10.8%) were identified as having gallstones. The mean age of the target population was 50 years, with a standard deviation of 17.3 years. A total of 3,177 individuals, constituting 51.15% of the sample, were female. Participants with greater potassium consumption were more frequently older, male, in marital or cohabitation relationships, and identified as White (not of Hispanic origin). They were also more likely to possess higher educational attainment, enjoy larger household incomes, and exhibit a higher body mass index (BMI). Additionally, these individuals exhibited higher levels of alcohol consumption and engaged in more active physical activity. They demonstrated a lower incidence of hypertension, diabetes, smoking, and asthma. Furthermore, they had higher intakes of calories, proteins, carbohydrates, fats, sugars, cholesterol, and water, as well as increased consumption of various dietary trace minerals, including calcium, iron, zinc, sodium, selenium, and copper.
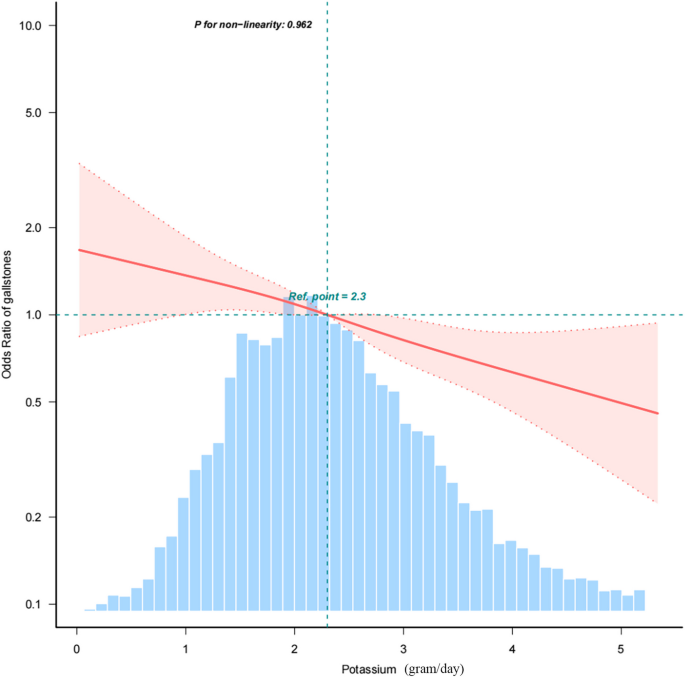
Table 2 The analysis revealed an association between dietary potassium consumption and the incidence of gallstones. In the unadjusted model, higher dietary potassium intake was linked to a lower prevalence of gallstones(OR = 0.83,95%CI:0.77–0.90, p < 0.001). Similarly, in the model with complete variable control (Model 3), this association remained consistent (OR = 0.81,95%CI:0.70–0.93, p = 0.003), indicating a 19% reduction in gallstone incidence for each 1 g increase in potassium intake. Additionally, we transformed dietary potassium intake into a trichotomous variable for sensitivity analysis. The findings indicated a trend suggesting that individuals with greater potassium intake were more likely to experience a decrease in the prevalence of gallstones (OR = 0.69,95%CI:0.51–0.94, p = 0.017). Furthermore, Fig. 2 demonstrates that the smoothed curve analysis shows an inverse linear correlation between dietary potassium consumption and the prevalence of gallstones (P for nonlinear = 0.962).
Figure 2 The relationship between dietary potassium intake and the odds ratio for gallstones is illustrated, with solid and dashed lines representing the predicted values and their corresponding 95% confidence intervals. These estimates were adjusted for various demographic and lifestyle factors, including age, gender, race, education level, marital status, PIR, BMI, alcohol consumption, smoking status, diabetes, hypertension, dietary supplement use, asthma, cancer, and physical activity. Additionally, the analysis accounted for specific dietary components such as total caloric intake, total sugar, total fat, total carbohydrates, total protein, total water, total cholesterol, calcium, iron, zinc, copper, sodium, and selenium intakes. It is important to note that only 98% of the data are displayed in this analysis (to more clearly demonstrate the linear relationship between dietary potassium intake and gallstone prevalence, data points that could distort the visualization have been excluded)
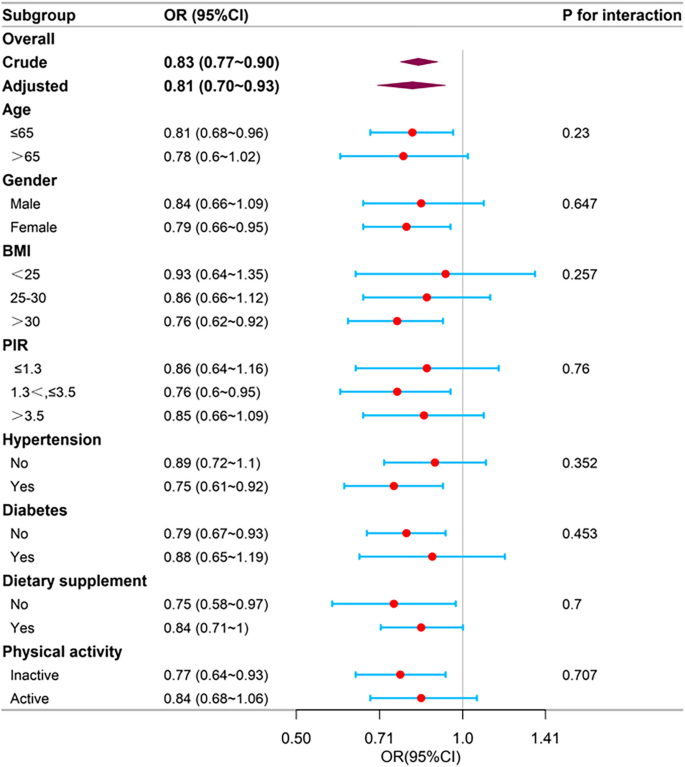
Stratified analyses were conducted to evaluate whether the association between dietary potassium intake and the risk of gallstone formation was influenced by factors including: age, gender, PIR, BMI, hypertension, diabetes, use of dietary supplements, and physical activity levels (see Fig. 3 for details). Following stratification for potential confounding variables, no significant interactions were identified in any of the subgroups.
Analysis of the relationship between dietary potassium intake and the risk of gallstones, stratified by basic demographic factors, lifestyle factors, and dietary elements. For each stratification, the analysis was adjusted for all other variables, excluding the stratification component itself. The variables included in the adjustments were age, gender, race, educational level, marital status, PIR, body mass index (BMI), alcohol consumption, smoking status, diabetes, hypertension, dietary supplement use, asthma, cancer, physical activity, total calorie intake, total sugar, total fat, total carbohydrate, total protein, total water, total cholesterol, calcium intake, iron intake, zinc intake, copper intake, sodium intake, and selenium intake. This approach ensures that the effects of potassium intake on gallstone risk are examined within distinct subgroups while controlling for potential confounding factors
Table 3 The recommended daily potassium intake is set at 4.7 g [33]. However, most Americans struggle to meet this requirement. In the 2003–2006 NHANES representative sample, only 3% of Americans achieved the adequate intake level [34]. On average, Americans consume just over half of the recommended amount, with a daily intake of approximately 2.6 g [55]. Recently, the World Health Organization (WHO) advises a minimum potassium intake of 90 mmol/day (3.5 g/day) for adults, based on conditional recommendation [56]. Based on the above findings, we categorized dietary potassium intake into groups in our study. According to the analysis, among the 6,223 participants in this study,3,784 individuals had a dietary potassium intake of less than 2.6g/d, accounting for 60.81% of the total population. Additionally,1,502 individuals met the average dietary potassium intake but did not reach the WHO-recommended intake level, with a gallstone incidence rate of 9.9%0.937 individuals exceeded the recommended dietary potassium intake, representing 14.14% of the total population, and the prevalence rate of gallstones in this group was 7.2%. As potassium intake increased, the prevalence of gallstones decreased. In the fully adjusted model (Model 3), individuals in the highest dietary potassium intake group (> 3.5 g/d) had a 24% lower risk of developing gallstones compared to those in the lowest intake group (< 2.6 g/d) (OR = 0.76,95% CI:0.64–1.08). Additionally, we conducted subgroup analyses and, after adjusting for all covariates, observed no significant interaction effects across subgroups defined by age, gender, PIR, BMI, hypertension, diabetes, use of dietary supplements, and physical activity levels (Table 4). The inverse relationship between dietary potassium intake and gallstones remained remained consistent in all subgroups, further supporting the robustness of this association across diverse populations.
In this cross-sectional study comprising 6,223 participants, a negative association was observed between dietary potassium intake and the occurrence of gallstones (OR = 0.69,95%CI:0.51–0.94, as presented in Table 2, Model 3). The robustness of this association was affected when adjusting for covariates. A consistent linear relationship between dietary potassium intake and gallstones was identified, supported by the fitted smoothing curves. Interaction tests across subgroups revealed no statistically significant within-group differences, indicating that the association between dietary potassium intake and gallstones was stable across diverse populations. Sensitivity analysis confirmed the stability of this relationship. To the best of our knowledge, this represents the first cross-sectional study examining the link between gallstones and potassium intake. These findings contribute to a more comprehensive understanding of the relationship between potassium and gallstones.
It is important to highlight that existing research has not yet thoroughly investigated the relationship between dietary potassium intake and the occurrence of gallstones. A study examining the relationship between dietary magnesium intake and gallstones revealed a significant linear inverse association between higher magnesium intake and a reduced prevalence of gallstones, with the atherogenic index of plasma (AIP) identified as a mediating factor in this relationship [40]. In contrast, research conducted by Shimeng Yan and colleagues found no significant association between dietary trace minerals such as iron, selenium, and zinc and the prevalence of gallstone disease (GSD). However, they identified a negative linear correlation between dietary copper intake and GSD prevalence, suggesting a potential regulatory role of copper in gallstone formation [41]. Another study focusing on serum iron levels and gallbladder stones proposed that iron deficiency might disrupt liver cholesterol metabolism, thereby contributing to the development of gallstones [42]. Additionally, a study exploring the link betweenblood cobalt levels and gallbladder stones found a significant association between elevated cobalt levels and an increased risk of gallstones, particularly among individuals over 60 years of age, women, those with serum cholesterol levels below 200 mg/dL, individuals with a BMI exceeding 25, and those with hypertension or diabetes [43]. A long-term follow-up study involving 860 middle-aged men demonstrated an inverse relationship between clinically diagnosed gallstones and calcium intake, suggesting that higher calcium consumption may reduce the risk of gallstone formation [44]. Recent research has further highlighted the roles of various minerals in gallstone development. Calcium, iron, and copper were found to potentially enhance the release of inflammatory factors and increase reactive oxygen species levels, both of which are positively associated with gallstone formation. Conversely, magnesium and zinc, due to their antioxidant properties, were negatively correlated with gallstone formation. These findings were supported by measurements of metal ions in gallstones, serum, and bile [45]. Multiple studies have suggested that specific dietary trace minerals may provide beneficial recommendations forthe prophylaxis and therapy of gallstones. Nonetheless it is clear that further investigation is warranted to meticulously examine the link between dietary potassium consumption and the development of gallstones within the broader population. To address this gap, we are utilizing data from the NHANES to delve into the potential association between dietary potassium and gallstones, as well as to assess the dosage effects.
Potassium is a vital nutrient and the predominant cation within intracellular fluid, where it is crucial for maintaining cellular efficiency, particularly in excitable cells such as muscle and nerve tissues [56]. It is abundantly present in foods originating from fruits and vegetables, with potatoes being particularly rich source. Potassium intake is associated with protective effects against hypertension, diabetes, stroke, cardiovascular disease, osteoporosis, kidney disease and non-alcoholic fatty liver disease. Although a link between dietary potassium consumption and the development of gallstones has not been previously established, analogous research has indicated that individuals with higher potassium intake exhibit a reduced likelihood of developing kidney stones [37]. Dietary potassium intake is inversely correlated with the recurrence of kidney stones [38, 39]. Although current research has not clearly established the specific mechanisms linking dietary potassium intake to the development of gallstones, we believe it may be related to the following factors: insulin resistance is currently acknowledged as an independent factor affecting the risk of gallstone formation [57]. Studies using potassium depletion and the hyperglycemic clamp method suggest that reduced potassium levels might lead to glucose intolerance due to compromised insulin release [58, 59]. Furthermore, the association between potassium intake and diabetes was explored in a longitudinal cohort study by Colditz et al.(1992), which encompassed a cohort of female(N = 84,360, aged 34–59) from the Nurse's Health Study. After a six-year follow-up, the research indicated that increased potassium consumption might correlate with a lower likelihood of developing type 2 diabetes mellitus (T2DM) in women with BMI of 29 or lower [60]. In a study encompassing 1,066 participants, researchers delved into the correlation between urinary potassium levels and the susceptibility to developing diabetes. Employing multivariate models that accounted for possible confounding variables like BMI, incorporation of fresh fruits and vegetables in the diet, and additional nutritional elements, the results showed that individuals at the minimum quintile of potassium consumption had over twofold the risk of developing diabetes as those in the uppermost quintile [61]. The link between potassium and T2DM also includes the influence of insulin on potassium metabolism. Elevated levels of plasma insulin are linked to improve cellular ingestion of potassium [62]. Unlike theglycemic response, which exhibits a threshold effect, these kalemia effects persistently intensify with increasing insulin levels [63]. This effect is similarly observed when intravenous insulin is employed as a therapeutic intervention for hyperkalemia, whereby insulin facilitates the translocation of potassium into cells, consequently decreasing its concentration in the bloodstream [63]. There is likely to be a heightened intracellular sodium sensitivity, enhancement of the sodium–potassium adenosine triphosphatase activity, and restriction of potassium outpouring that contributes to these events [62]. The formation of gallstones is triggered by elevated levels of cholesterol or bilirubin in the bile [64]. In a randomized controlled trial (RCT) examining the effects of magnesium and potassium supplements on cholesterol levels and quality of life (QoL) in patients with type 2 diabetes mellitus, it was found that the treatment significantly impacted cholesterol levels, with the most substantial reduction observed in the group receiving potassium supplements [65]. According to a recent study, the risk of gallstones increases with the elevation of serum triglycerides [66]. Another study examining the different correlations between patterns of dyslipidemia and dietary factors showed that triglyceride levels were significantly associated with low calcium, low potassium, low milk, and low dairy intake [67]. The evidence suggests that dietary patterns in children and adolescents characterized by higher intakes of vegetables, fruits, whole grains, fish, low-fat dairy, and legumes(these dietary patterns are also higher in potassium [36], and lower intakes of sugar-sweetened beverages, sweets, and processed meat, are associated with lower blood pressure and improved blood lipid levels, including lower LDL cholesterol, higher HDL cholesterol, and reduced triglycerides later in life [68]. Furthermore, it was recently discovered that intestinal bacteria can facilitate cholesterol crystallization in a mouse model of gallstone formation [69]. A study in a population-based cohort of Chinese adults provided substantial observational evidence of the associations of excessive sodium intake and inadequate potassium intake with the gut microbiota and plasma metabolites [70]. The activation of membrane K+ channels leads to hyperpolarization of the plasma membrane and further suppresses Ca2+ influx into the cell, resulting in relaxation of thegallbladder smooth muscle [71]. Different levels of dietary potassium intake may cause such channel dysfunction, leading to impaired gallbladder motility and gallbladder stasis, which are key factors in thepathogenesis of biliary cholesterol crystallization and gallstones [72].
In the NHANES 2017–2020 year cycle, only 671 individuals were diagnosed with gallstones. Future studies will incorporate a larger population of individualswith gallstones to explore the relationship between the more precise recommended intake of dietary potassium and gallstone incidence. Furthermore, in the sensitivity analysis, as the level of dietary potassium intake continued to increase, the number of individuals meeting the recommended intake decreased. However, a significant downward trend in the prevalence of gallstones was observed, particularly among those with an intake greater than 3.5 g/day. This study is a preliminarily exploration of the relationship between dietary potassium intake and the prevalence of gallstones, providing direction for the next step of quantitative analysis on the association between dietary potassium intake and the prevalence of gallstones. Although this study did not identify the more optimal dietarypotassium intake for the prevention of gallstones, this association is particularly evident among US adults whose potassium consumption meets or surpasses the recommended intake of 3.5 g.
This research has several significant advantages. It represents the inaugural investigation into the connection between dietary potassium intake and the prevalence of gallstones. Regarding the reduction of gallbladder stone prevalence, the study offers valuable insights. Early dietary interventions are a more cost-effective approach to managing the condition. The study included a diverse, multiracial group of adults with varied dietary habits across the United States. Nevertheless, there are a number of inadequacies associated with our study. First, the cross-sectional design of the study precludes the establishment of causality. Second, the study relied on self-reported data and lacked precise imaging diagnostics. Since most gallstones are asymptomatic, the results may have been affected by whether participants had regular medical checkups or received appropriate medical care from their primary care physicians. This also raises the possibility of misdiagnosis regarding the presence or absence of gallstones, which may introduce research bias. Additionally, the gallstone information was obtained from the question “Have you had gallstones?”. The database did not provide detailed clinical variables, such as specificstone composition. We could not distinguish between cholesterol stones and bile pigment stones. Further classification studies can be conducted in the future. Moreover, the medication history data for NHANES between 2017 to 2020 was unavailable. Finally, this study serves as an initial investigation into the link between dietary potassium and the prevalence of gallstones, offering insights for future quantitative research on the relationship between dietary potassium intake and gallstone prevalence. Moving forward it will be essential to incorporate larger and more diverse populations into cohort studies to determine the more precise dietary potassium intake for the prevention and management of gallstones.
This study indicates that higher dietary potassium intake is linked to a lower prevalence of gallstones. This association is particularly evident among US adults whose potassium consumption meets or surpasses the recommended intake of 3.5 g. Our findings suggest that inadequate potassium intake may impact glucose metabolism, lipid metabolism, induce microbial dysbiosis, and lead to electrophysiological irregularities, all of which can contribute to gallstone formation. Moreover, we observed an inverse relationship between dietary potassium intake and gallstone prevalence. However, this finding is subject to the influence of confounding variables and requires validation through additional research. Ultimately, to establish a more precise recommendation for dietary potassium intake and to understand the long-term effect of potassium metabolism on gallstone development, further prospective studies are needed.
The dataset underpinning the findings presented in this paper is readily accessible via the National Health and Nutrition Examination Survey (NHANES) repository, which can be found at https://www.cdc.gov/nchs/nhanes/.
- PIR:
-
Poverty-to-income ratio
- BMI:
-
Body mass index
- NHANES:
-
National Health and Nutrition Examination Survey
- T2DM:
-
Type 2 diabetes mellitus
- T:
-
Tertiles
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- GSC:
-
Gallbladder cancer
- HDL:
-
High-Density Lipoprotein
- LDL:
-
Low-Density Lipoprotein
- AIP:
-
Atherogenic index of plasma
- US:
-
United States
The authors extend their sincere thanks to the participants and researchers who contributed to the National Health and Nutrition Examination Survey (NHANES). They also acknowledge NHANES for making their data accessible and open-source, which facilitated this research.
The authors disclose that financial support was obtained for the research, authorship, and/or publication of this article. This work was funded by the 2023 Natural Science Foundation of Inner Mongolia Autonomous Region, with the grant number 2023MS08051.
The human-involving studies received approval from the Ethical Review Board at the National Center for Health Statistics. These studies were carried out in compliance with local laws and institutional protocols. Participants' legal guardians or next of kin provided written informed consent for theirinvolvement in the research. The data utilized in this research were anonymized and are publicly accessible on the NHANES website.
Not applicable.
The authors declare no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Yang, S., Jiao, N., Wang, J. et al. Association between dietary potassium intake and the prevalence of gallstones in American adults: an assessment of data from the national health and nutrition examination survey. BMC Gastroenterol 25, 197 (2025). https://doi.org/10.1186/s12876-025-03744-y