BMC Oral Health volume 25, Article number: 452 (2025) Cite this article
Dens invaginatus (DI) is a developmental anomaly arising from excessive proliferation or distortion of the enamel organ during tooth formation, often leading to the creation of a pocket or dead space within the tooth. This report presents a case of Type II DI in a maxillary lateral incisor with unique anatomy, diagnosed through cone-beam computed tomography (CBCT) and further analyzed with micro-computed tomography (micro-CT) post-extraction.
A 20-year-old male patient presented with recurrent pain and gingival swelling around the apex of tooth #22 for 12 months, unresponsive to antibiotic therapy. CBCT examination revealed a well-defined radiolucent area measuring approximately 10.3 × 9.9 × 7.0 mm at the apex of tooth #22, with an oval shape and distinct cortical border. The CBCT images confirmed that the invagination extended into the pulp chamber but did not reach the root apex. Based on these findings, a diagnosis of Type II DI with chronic apical periodontitis was established. The patient opted for extraction, and histopathological analysis of the apical lesion confirmed a periapical granuloma. Micro-CT analysis of the extracted tooth revealed that the invagination communicated with the external oral cavity via a pit in the crown and with the internal root canal system, serving as the conduit for pulp infection. Multiple apical accessory canals were identified, contributing to the persistent periapical infection and development of a periapical granuloma.
This case highlights the complexity of DI and the challenges in treatment due to its unique anatomical features. The report underscores the value of three-dimensional imaging techniques, such as CBCT, in the diagnosis and management of DI.
Dens invaginatus (DI) arises from excessive proliferation or distortion of the enamel organ into the dental papilla during the morpho-differentiation phase of tooth development [1]. This condition can result in the formation of a pocket or anatomic dead space on the tooth surface following eruption [2]. The thin lining of the invagination in DI tends to trap bacteria, leading to early caries and consequently pulp necrosis [3]. The anomaly originates in the early stages of tooth development, specifically during the cap stage, where abnormal pressure or growth disturbances causes the enamel organ to invaginate into the dental papilla. As the tooth continues to develop, the invaginated enamel organ proliferates and differentiates alongside the surrounding dental tissues, potentially extending into the root and forming a complex internal structure that may encompass enamel, dentin, and pulp tissue [2, 4,5,6]. The etiology of DI remains controversial and unclear, with genetic or mechanical theories being the most widely accepted explanations [7]. A genetic predisposition is suggested by familial clustering and the high prevalence of DI in specific ethnic groups [8]. It is hypothesized that external forces from adjacent tooth germs, along with trauma and infections, may contribute to the invagination of enamel into the dental papilla [7]. Furthermore, factors such as focal growth retardation or acceleration of the tooth bud, as well as restrictions imposed by the dental arch on the enamel organ, have also been considered as potential contributors [9]. Reported prevalence rates of DI vary significantly, ranging from 0.04% to12% across different studies [9, 10]. This variation is likely attributed to racial differences, as well as differing diagnostic criteria and investigation methods.
DI predominantly occurs in permanent teeth, although it has occasionally been observed in deciduous teeth; among tooth types, maxillary lateral incisors are most commonly affected, followed by maxillary central incisors and canines [11]. The morphological features of this invagination exhibit considerable variability in terms of depth and structural complexity. Several classification systems have been proposed to characterize this anomaly. Among these, the most widely adopted classification system was established by Oehlers [5], who categorized DI into three types based on radiographic characteristics: Type I, where the invagination is confined to the crown and does not extends beyond the cemento-enamel junction (CEJ); Type II, where the invagination extends beyond the CEJ but does not reach the entire root length; Type IIIa, where the invagination penetrates through the root and opens in the periodontal ligament space via a pseudo-foramen; and type IIIb, where invagination traverses the root and contacts the periapical region at the apical foramen (Fig. 1). Oehlers [5, 6] also identified various crown shapes associated with the three types of DI, including normal crowns with a pronounced lingual or palatal pit, as well as conical, barrel-shaped, or peg-shaped crowns featuring an incisal pit. Chen et al. [12] reported that Type I (87.5%) was the most prevalent form in a Chinese subpopulation, significantly higher than the incidence of Type II (12.23%) and Type III (0.72%). DI increases the risk of developing pulpal pathosis, which may be attributed to the absence of enamel in the invagination and the presence of remnants of the dental papilla or periodontal connective tissue [2, 13]. Previous scholars have reported that the enamel within the invagination could be hypoplastic [14]. This condition heightens the risk of microbial penetration and subsequent infection of the pulp tissue, potentially resulting in pulp necrosis.
Classification of dens invaginatus. (Image source: Sathorn C, Parashos P. Contemporary treatment of class II dens invaginatus. Int Endod J. 2007;40 (4):308 − 16.)
In this report, we present a case of Type II DI affecting a maxillary lateral incisor, which ultimately required extraction due to refractory apical periodontitis. Pre-treatment evaluation was performed using cone-beam computed tomographic (CBCT), and post-extraction analysis was conducted using micro-computed tomography (micro-CT). The unique anatomy of this tooth may offer valuable insights for appropriate dental management strategies.
A 20-year-old male presented to the Department of Dentistry at the Affiliated Hospital of Nantong University on March 18, 2024, with a 12-month history of recurrent pain and swelling in the left anterior maxillary region. Prior to this visit, the patient had sought treatment at a local rural clinic, where he was prescribed ornidazole and amoxicillin (500 mg each, twice daily) for 10 days. However, the symptoms persisted despite adherence to the antibiotic regimen. The patient denied any history of trauma or previous dental interventions in the affected area. No periapical radiographs were documented during the prior treatment.
Intraoral examination revealed that tooth #22 exhibited a barrel-shaped morphology, characterized by a depression at the incisal edge and the absence of the palatal fossa and developing groove. A small dark pit was observed at the foramen coecum. A palpable swelling, tender upon palpation, was noted on the anterior maxilla, adjacent to the apical area of tooth #22. The tooth demonstrated sensitivity to percussion and exhibited Grade I mobility. Thermal testing indicated that tooth #22 was non-vital, although the color of the crown remained normal. Examination of the contralateral lateral incisors revealed normal findings.
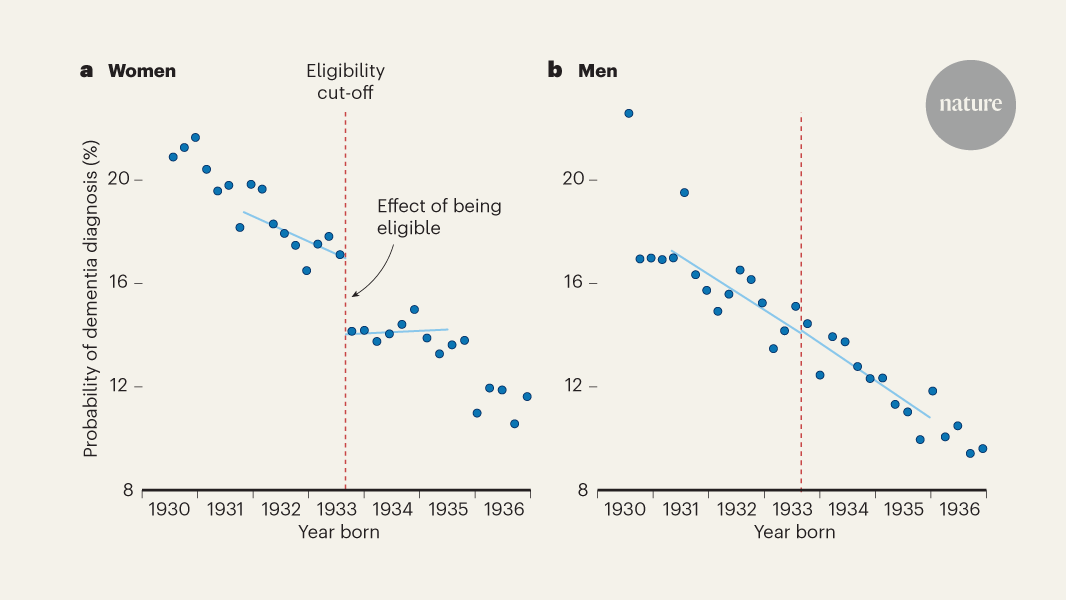
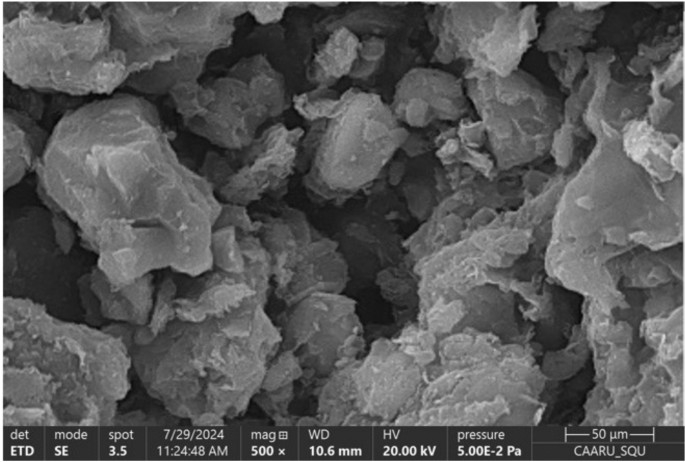
Given the complexity of the symptoms and the need for detailed anatomical evaluation to establish an accurate diagnosis, a CBCT scan (3D eXam I, KaVo Dental GmbH, Germany) was performed with adherence to the “as low as reasonably achievable” (ALARA) principle for radiation dose optimization. The CBCT images (Fig. 2A-C) revealed a well-defined radiolucent area measuring approximately 10.3 × 9.9 × 7.0 mm at the apex of tooth #22, with the radiolucent margin extending from the apex to the middle third of the root. The apical lesion exhibited an oval shape with a distinct cortical border. The enamel invagination extended beyond the CEJ and reached the mid-root level, indicating a type II DI. Due to the voxel size limitation of 250 μm, it was unclear whether the invaginated canal communicated with the main root canal. Based on the clinical and CBCT findings, a diagnosis of type II DI with associated pulpal necrosis and chronic apical periodontitis was established. Given the complexity of the root/canal structure and the extent of bone defect, the prognosis of conservative treatment was considered uncertain. The patient was informed of the available treatment options, which included extraction or endodontic therapy with surgical intervention. Considering the complexity of treatment procedure, the high dental cost, and the uncertain success rate, the patient opted for extraction. Consequently, tooth #22 was extracted (Fig. 2D-F), and the periapical lesion was thoroughly removed. The excised periapical lesion was submitted for histopathological examination, which confirmed the diagnosis of a periapical granuloma (Fig. 3). The granulomatous tissue was predominantly infiltrated with inflammatory cells, including lymphocytes, plasma cells, neutrophil, and macrophages, without evidence of an epithelium-lined lumen.
A case of Type II dens invaginatus (DI) in the tooth #22. (A-C) Dental CBCT examination: (A) paramaniac view, (B) sagittal view, (C) coronal view; (D-F) extracted tooth #22 with DI: (D) buccal view, (E) lingual view, (F) occlusal view (arrow indicates a dark pit at the foramen coecum); (G-L) micro-CT examination: (G) coronal section (arrow indicates a connection between the invaginated pseudo canal and the true main canal), (H) axial section, (I) sagittal section (arrow indicates an enamel defection at the button of the invaginated canal), (J) palatal view of the 3D reconstructed tooth model (Tooth #22 displays a barrel-shaped crown featuring an incisal pit), (K) 3D reconstruction of the invaginated pseudo canal (blue), and (L) 3D reconstruction of the true main canal (red) and the invaginated canal (blue)
Histopathological analysis of the excited periapical lesion confirmed the diagnosis of a periapical granuloma (hematoxylin-and-eosin staining, scale bar is 50 μm)
To gain a more detailed understanding of the anatomy of DI, the extracted tooth was scanned using a micro-CT device (SkyScan1174; Bruker-microCT, Kontich, Belgium) with a voxel size of 32 μm. Both the tooth structures and the root canal system were reconstructed in three dimensions (3D). The 2D (Fig. 2G-I) and 3D (Fig. 2J-L) micro-CT images revealed that the invagination communicated with the external oral cavity via an incisal pit at the foramen coecum and with the main root canal at the mid-root level, serving as a conduit for pulp infection. The enamel surrounding the invagination exhibited uneven thickness, with an enamel and dentin defect at the apical end forming a connection to the pulp cavity. The enamel and the underlying dentine were completely folded into the root, creating a concentric structure and a “pseudo root canal” at the center, while compressing the original pulp cavity into a concentric, sheet-like structure, thereby complicating access to the main root canal during root canal therapy. Additionally, apical ramifications with five accessory canals were also identified at the root apex (Fig. 2L).
Early detection of DI is crucial to prevent complications such as pulpitis and/or periapical periodontitis. The invagination acts as a potential pathway for microorganisms and irritants to reach the pulp, potentially leading to inflammation and necrosis [9]. DI is a dental anomaly with potential genetic and ethnic predispositions [7, 8]. During tooth development, ectomesenchymal signaling pathways are crucial in controlling the growth and folding of the enamel organ. A deficiency in specific molecules can lead to irregularly shaped teeth and defects in the developing tooth germ. Therefore, the hypothesis that genetic factors could be responsible for DI is plausible [2, 9]. DI has been association with various syndromes, including those with genetic origins such as Williams, Nance-Horan, and Ekman-Westborg-Julin syndromes [9]. Pokala and Acs [15] documented a case where an individual with a deletion at chromosome 7q32 exhibited DI alongside other dental anomalies, such as hypodontia. These findings suggest a potential genetic basis for DI, highlighting the importance of considering genetic and possibly ethnic factors in its etiology. Additionally, the prevalence of DI varies among ethnic groups, suggesting an ethnic predisposition. For instance, certain populations, including the Chinese populations [5, 12], exhibit a higher incidence of DI and barrel/shovel-shaped maxillary lateral incisors, which could be attributed to genetic variations or environmental factors specific to those groups. Understanding these predispositions is essential for early diagnosis and management, enabling clinicians to identify high-risk individuals and implement preventive measures effectively [12].
Although teeth with DI often exhibit atypical crown shapes, such as conical, peg-shaped, barrel-shaped, or dilated forms [4], these morphological abnormalities do not consistently indicate the presence of a DI lesion. DI is frequently discovered incidentally during radiographic examinations, where the invagination appears as a deep, enamel-lined fissure, often associated with the formation of a radiolucent pocket [16]. This condition results in complex root canal morphology, posing significant challenges for endodontic treatment. Oehlers’ classification, based on 2D radiographic images, may underestimate the true extent and complexity of the invagination, as it is a 3D structure with varying extensions in different planes [2]. Therefore, CBCT is particularly valuable for the accurate diagnosis and management of DI [12].
Treatment strategies for DI, such as root canal therapy, removal of the invagination, intentional replantation, and surgical intervention, are determined based on the classification of DI and the condition of the pulp and periapical tissues [4, 17]. Sealing the invaginations is recommended as a prophylactic measure when the pulp is not infected. For lesions that are not extensive, the application of flowable composite is generally adequate for sealing. In more severe cases, particularly those near the pulp, the use of mineral trioxide aggregates or bioceramic materials may be more appropriate [8]. In instances involving deep periodontal pockets, periodontal flap surgery may also be indicated. However, a study has demonstrated a failure rate of 13.4% for prophylactic invagination treatments after a follow-up period of six months or longer, with all reported failures occurring in cases of Type II DI [17]. Consequently, periodic follow-up examinations are essential to prevent the development of periapical disease. In this case, given the absence of a radicular groove and the patient’s age of 25, with periapical periodontitis symptoms emerging only in the past year, we speculate that early prophylactic sealing of the invagination post-eruption could have prevented pulp necrosis and the development of a periapical granuloma, thereby preserving the tooth. However, the pit at the occlusal foramen coecum (Fig. 2F), which is the entrance to the invagination, along with the mildly barreled tooth shape, may be easily overlooked during dental examination. Even if identified, these features may not necessarily lead to the consideration of DI and the need for sealing.
Once the invagination becomes infected, more complex treatment modalities are required. Advances in pulp biology and recent clinical research on vital pulp therapy have provided new insights into biologically driven treatment options [18]. In cases where uninflamed pulp tissue remains and the pulp has not undergone complete necrosis, pulpotomy may be considered, particularly in immature teeth, to promote continued root development [18]. Under magnification, hemostasis is achieved, the degree of inflammation is assessed, and inflamed pulp tissue is excised to allow the remaining healthy tissue to recover and heal [19]. However, if the inflammation progresses, root canal treatment may ultimately be necessary. In recent decades, pulp revascularization has emerged as a promising treatment for immature teeth affected by DI, with several successful cases reported [20,21,22]. This technique specifically designed for immature permanent teeth with necrotic pulp, aiming to promote root development by harnessing the differentiation potential of remaining stem cells [11].
There is currently no consensus on whether the invagination should be removed, particularly in Type II and III DI. While retaining the invagination may enhance root strength, residual debris within the invagination can impede effective cleaning and obturation of the root canal system, potentially compromising treatment outcomes [11]. In instances where the invagination does not communicate with the root canal system via accessory canal(s) or dentin defects, the pulp may remain vital and healthy, allowing for the isolated treatment of invagination [8, 23]. Regardless of the presence of an apical lesion, nonsurgical endodontic treatment should be prioritized [24]. Although, the complex anatomy of DI may reduce the success rate of such treatments, surgical intervention should not be considered as the initial approach. To improve success rates, the use of an operating microscope and CBCT is essential for thorough cleaning, shaping, and filling of the root canal system [23]. Recent advances in contemporary endodontics have introduced splints based on internal anatomical information derived from CBCT, facilitating guided and minimally invasive access to the pulp cavity [25]. Following root canal treatment, periodic follow-up is necessary to assess therapeutic efficacy. If treatment failure is detected, endodontic surgery or intentional replantation may be considered. Should these interventions fail and the lesion remains uncontrollable, extraction may become the final option [26].
In this case, it is regrettable that the patient chose extraction over attempting therapeutic intervention. The preoperative CBCT examination and post-extraction micro-CT analysis reveal that the primary challenge in treating this case lies in effective removal of the pulp and pathological tissues from the root canal system, particularly in the coronal and middle third levels. Figure 2B and J show that the invagination is entirely embedded in the center of the tooth, making its removal extremely challenging. The central pseudo root canal was expected to contain periodontal tissues rather than the dental pulp, and it does not communicate with the external periodontal space. The blind canal terminates apically with enamel and dentin defects that connect to the main root canal through gaps or tubules. A more prudent strategy would be to preserve the invagination and establish a pathway through it to access the main root canal and apex. However, the pulp chamber was severely compressed by the invagination, complicating the ability of instruments to reach the working length and thoroughly clean the entire root canal space. Large amounts of debris and uninstrumented areas may remain in the irregular area of the pulp chamber after canal instrumentation. Theoretically, sufficient canal irrigation or deeper penetration with small files using ultrasonics is recommended to remove tissues from the irregular space of the root canal system. Additionally, the presence of apical ramification and a periapical granuloma suggests that conventional root canal treatment is unlikely to completely eliminate infectious debris within the root canal system. Consequently, the prognosis is poor without the intervention of apical surgery. As illustrated in Fig. 2L, micro-CT imaging revealed the presence of multiple (five) apical accessory canals that were not detectable using CBCT. These accessory canals may contribute to persistent apical inflection and the development of a periapical granuloma. Apicoectomy with a 3 mm apical resection can effectively remove the majority of the apical delta and infected tissue, which are challenging to clean and shape using conventional endodontic techniques. However, root-end resection may expose irregular canal spaces and complex anatomical structures associated with the invagination. Meticulous retropreparation and retrofilling of these areas are critical to achieving predictable periapical healing. Although no endodontic treatment or apical surgery was performed in this case, it highlights the importance of a detailed analysis of the root canal system in cases of DI, particularly in differentiating between an invaginated “pseudo root canal” and the true main root canal system.
This study has several limitations that warrant acknowledged. First, the analysis is based on a single case of DI with atypical tooth anatomy, which limits the generalizability of the findings to a broader population. Second, while the patient’s decision to undergo extraction facilitated detailed micro-CT evaluation, the clinical relevance of the observed anatomical variations remains theoretical, as no conservative therapeutic interventions were pursued. A clearer understanding of endodontic treatment options could have significantly influenced the patient’s decision regarding tooth extraction. Informing the patient about the potential for tooth preservation through advanced endodontic procedures, such as root canal therapy, and/or apical surgery, might have led to a preference for less invasive options. Educating the patient on the success rates, benefits, and potential complications of these treatments could have provided a more comprehensive perspective, potentially favoring tooth preservation over extraction. Additionally, the costs and time involved in endodontic treatment versus extraction might have influenced the decision. Finally, demographic factors such as ethnicity, age, and gender significantly influence the presentation of this dental anomaly [8, 12, 27]. To mitigate potential selection bias and enhance the generalizability of the findings, future research should prioritize multi-centered, in vivo CBCT studies involving larger, ethnically diverse cohorts across a wider age range.
In conclusion, this case report highlights the intricate and unique morphological characteristics of the root canal system in a maxillary lateral incisor with Type II DI. The invaginated radicular region is particularly susceptible to establishing pathways of communication with both the external oral environment and the internal root canal system, thereby increasing the risk of endodontic and periodontal infections.
Data is provided within the manuscript.
- CBCT:
-
Cone-beam computed tomography
- CEJ:
-
Cement-enamel junction
- DI:
-
Dens invaginatus
- micro-CT:
-
Micro-computed tomography
Not applicable.
Supported by Suzhou “Medical Health Science and Technology Innovation” Project (SKY2022030).
This case report has been approved by the Ethics Committee of Ninth People’s Hospital of Suzhou with the approval number # KY2022-089-01. Informed consent was obtained from the subject.
Written informed consent was obtained from the patient for publication of this case report.
The authors declare no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Zhou, W., Jiang, R., Gu, Y. et al. Unique anatomy of a rare type II dens invaginatus in a maxillary lateral incisor: a case report. BMC Oral Health 25, 452 (2025). https://doi.org/10.1186/s12903-025-05823-8