BMC Medical Ethics volume 26, Article number: 83 (2025) Cite this article
Taiwan passed the Patient Right to Autonomy Act in 2016 and introduced a legal document called advance decision to address dilemmas in making life-sustaining treatment (LST) decisions for incompetent patients. However, the proportion of Taiwanese adults who have completed an advance decision remains low, and public preference trends are unclear.
A cross-sectional telephone survey was conducted among Taiwanese adults using a structured questionnaire to assess preferences regarding five types of LSTs across four hypothetical clinical scenarios (late-stage motor neuron disease, severe dementia, irreversible coma, and terminal cancer). Participants were categorized based on their preference patterns, and factors associated with each subgroup were analyzed.
Of the 3188 individuals contacted, 2440 declined to participate, and 748 (24.3%) respondents were successfully interviewed. A total of 747 responses were included in the analysis. Latent class analysis identified four preference subgroups: pro-forgo (more than half of the respondents), neutral, aggressive, and motor-neuron-disease specific. Older age, higher education, and better quality of life were associated with a greater likelihood of belonging to the pro-forgo group, while being male, unmarried, currently not working, or not residing in northern Taiwan were associated with a lower likelihood.
Most respondents expressed a consistent preference to forgo LSTs in the hypothetical clinical scenarios. This suggests that the advance decision, implemented in 2019, may align with public needs. However, given the low completion rate and prevalent preference patterns, policymakers should increase efforts to ensure that those in need have access to appropriate resources and consider implementing a tiered signing process.
Delivering goal-concordant care is essential to healthcare quality, but it remains especially challenging for patients at the end of life or those with impaired consciousness [1,2,3]. Most people prefer to discontinue life-sustaining treatments (LSTs) and opt for palliative or hospice care when their physical condition deteriorates significantly [4,5,6].However, in the absence of explicit treatment refusals from patients, decisions to terminate or withhold LSTs in those unable to express their wishes can place physicians in ethically complex situations [7, 8]. Although sustaining life is typically viewed as a fundamental benefit, this assumption becomes less clear under such conditions. To address this dilemma, various forms of advance directives (AD), such as living wills, have been developed over the past decades [9]. While the specific content of these documents may vary, they share the common purpose: to allow individuals to articulate their care preferences in advance, based on hypothetical clinical scenarios [10]. When a patient later encounters one of these situations, decisions guided by their AD can be ethically justified under the principle of autonomy [11].
In Taiwan, the legally recognized living will—the letter of intent for the choice of hospice palliative care or life-sustaining treatment—was established under the Hospice Palliative Care Act (2000). This document allows individuals to record preferences for “do-not-resuscitate” (DNR) orders and the refusal of LST, which becomes applicable once a terminal condition has been diagnosed by two specialist physicians [12, 13]. However, this document does not apply to non-terminal conditions such as a permanent vegetative state or coma, despite many people’s preference to forgo LST in such circumstances. To address these gaps, Taiwan enacted the Patient Right to Autonomy Act in 2016, creating a new legal document known as advance decision. This expands the applicable clinical conditions to include irreversible coma, permanent vegetative state, severe dementia, and other incurable and unbearable conditions, such as motor neuron diseases (MNDs), where no effective treatment is available [14].Additionally, the advance decision explicitly includes artificial nutrition and hydration (ANH) among the interventions that can be refused in advance. After three years of preparation, this new law and its associated document came into effect in January 2019.
Despite the legal advances, the uptake has been limited. As of December 2023, only about three out of every thousand Taiwanese adults aged 20 or older have signed an advance decision. Therefore, public preferences regarding LST in these scenarios remain poorly understood. To assess and reflect on the current state of advance decision implementation in Taiwan, we conducted a national telephone survey of the general population. Respondents were presented with four hypothetical clinical scenarios based on the legal conditions defined in the advance decision and asked about their preferences regarding five LST options. We then used latent class analysis to identify distinct preference patterns and examined the sociodemographic factors associated with each subgroup.
This cross-sectional, national phone survey was conducted by the Public Opinion Center of Shih Hsin University in November 2019. Participants aged 20 years and older were randomly selected from 22 counties and cities in Taiwan using Chunghwa Telecom landline phone numbers as the sampling frame. Computer-assisted personal interviewing (CAPI) was used to collect and manage data. Verbal consent was obtained after interviewers explained the purpose of the survey and confirmed participants’ age and willingness to participate. In total, 3,188 individuals were contacted, of whom 2,440 refused, yielding 748 completed interviews (response rate: 24.3%). No personally identifiable information was collected.
The Patient Right to Autonomy Act, enforced in Taiwan in January 2019, permits competent adults to document their preferences for LSTs through an advance decision under specific clinical conditions. Four clinical scenarios were designed: irreversible coma, terminal colorectal cancer, severe dementia, and late-stage MNDs. Each scenario involved extreme physical decline and fell within the scope of the Act. Respondents rated their preference for five LSTs—antibiotics for pneumonia, dialysis for renal failure, artificial ventilation, cardiopulmonary resuscitation (CPR), and nasogastric tubes for dysphagia—using a 5-point Likert scale (1 = definitely do not want, 2 = probably do not want, 3 = unsure, 4 = probably want, 5 = definitely want). (See Additional file 1). The questionnaire was adapted from the Life Support Preferences Questionnaire proposed by Coppola [15],which has demonstrated good validaty and has been widely used to assess individual or surrogate preferences for LSTs [16,17,18].
The demographic characteristics included gender, age (years), marital status (unmarried, married, divorced/separated/widowed), education level (elementary, junior high, high school, college or above), occupation (white-collar, blue-collar, currently not working, other), and geographic region (northern, central, southern, eastern Taiwan). Other characteristics included self-rated quality of life (1–5 scale), religious affiliation (yes/no), presence of any of the following chronic diseases (hypertension, diabetes, cardiovascular disease, kidney disease, liver disease, cancer, neurological disease, chronic obstructive pulmonary disease; coded as yes/no), and experience caring for a family member with a severe illness or at the end of life (yes/no).
Descriptive statistics of the LST preferences in hypothetical scenarios are reported. Latent class analysis was conducted to categorize respondents into subgroups according to their preferences for LST in each clinical scenario. The latent class analysis utilizes observed variables to characterize distinct unobserved subgroups (latent classes). We aimed to identify and recognize these unobserved, categorical subgroups. First, we determined the optimal number of latent classes among 2 to 5 groups based on model fit indicators (Akaike information criterion and Bayesian information criterion). We then conducted a one-way ANOVA with Scheffé post-hoc test to compare the differences in attitudes toward the use of LST to determine which groups were the most and least willing to undergo LST. Finally, we defined the group least inclined to undergo LST as the pro-forgo group and used logistic regression to investigate which characteristics were associated with being in this group. We used Stata version 16 to perform latent class analysis. Other data analyses were conducted using the IBM SPSS statistical package (version 25.0, SPSS; Chicago, IL, USA). All statistical analyses were two-tailed.
Of the 748 respondents successfully interviewed, 747 were included in the analysis (Table 1); one was excluded due to substantially incomplete data. Among the included participants, 327 were men (43.8%) and 420 were women (56.2%). The mean age was 53.9 years (standard deviation = 14.7 years). Most participants were married (78.8%), and nearly half had a university degree (49.5%). More than 40% were white-collar workers, and more than 40% were not currently working (retired, homemakers, or students). Nearly 80% rated their quality of life as very good or good, whereas only 6.2% felt their quality of life was bad or very bad. Almost one-third had no religious affiliation, and one-third had a chronic illness. More than half had experienced caring for a family member who was seriously ill or at the end of life (54.9%). Table 2 shows that most respondents inclined to refuse (no and probably no) LSTs across all clinical scenarios (70.2–92.8%). Among the five LSTs, artificial ventilation and CPR were the least prefered. Respondents expressed the most definite attitudes in the irreversible coma scenario.
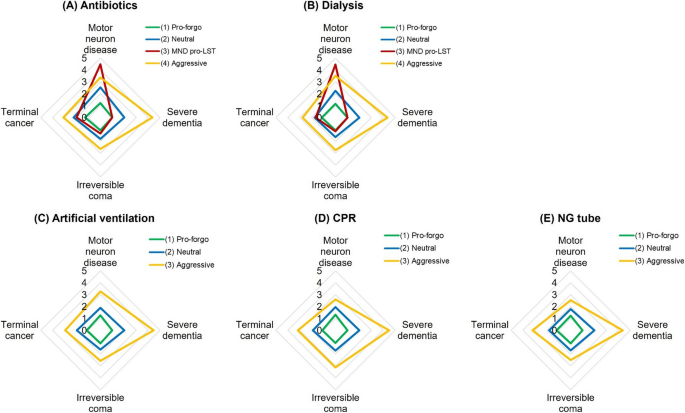
Based on the model fit indices, the latent class analysis revealed that two treatments, antibiotics and dialysis, fit into four groups (pro-forgo, neutral, MND pro-LST, aggressive). By contrast, artificial ventilation, CPR, and nasogastric tubes fit into three groups (pro-forgo, neutral, aggressive). Table 3 shows the group sizes and the mean scores for willingness to undergo LSTs under the four clinical situations. Higher scores indicate a greater willingness to undergo LST. Among the five LSTs, the pro-forgo group had the highest proportion of participants, ranging from 56.4% to 79.3%. Figure 1 presents the mean willingness scores for each LST in a radar plot. The one-way ANOVA results for the preference for life-sustaining treatment were significant across the groups. According to the Scheffé post-hoc test, the pro-forgo group had the lowest mean scores, indicating the most support for forgoing LST. In contrast, the aggressive group had the highest intention to have LST. And the fourth group was only identified in antibiotics and dialysis, presenting an increased willingness to undergo these two treatments in MND scenarios (Fig. 1).
Table 4 presents the results of the logistic regression model for the pro-forgo group. Overall, men were less willing to forgo LST than women. Specifically, concerning dialysis, artificial ventilation, and CPR, there were 33%, 50%, and 40% fewer odds for men to express a position to withhold treatments than women. Furthermore, older adults were more supportive of forgoing LST. The odds increased by 2% for each additional year of age for antibiotics, dialysis, artificial ventilation, and CPR. Unmarried individuals took a relatively anti-forgo stance than married individuals; 39% to 57% fewer odds of supporting forgoing antibiotics, artificial ventilation, CPR, and nasogastric tubes. Compared to those with elementary education, respondents with higher education had higher odds of supporting forgoing dialysis, artificial ventilation, and CPR. Respondents who did not work had lower odds of supporting forgoing CPR than white-collar workers. Notably, the higher the quality of life of a respondent self-rated, the higher the odds for them to express a positive attitude toward forgoing artificial ventilation, CPR, and nasogastric tube. Additionally, those with experience caring for the family had higher odds of being supportive of forgoing dialysis and CPR. Finally, compared to those living in northern Taiwan, those living in other areas had lower odds of being positive about forgoing artificial ventilation, CPR, or nasogastric tube, especially those living in eastern Taiwan.
The latent class analysis revealed that certain groups exist in the Taiwanese general public, which was sorted according to their preference patterns regarding LST. For artificial ventilation, CPR, and nasogastric tube, three subgroups were identified (pro-forgo, neutral, and aggressive). For antibiotics and dialysis, four subgroups were identified (pro-forgo, neutral, aggressive, and MND-specific pro-LST). More than half of the respondents belonged to the pro-forgo group, and we identified specific sociodemographic characteristics associated with the pro-forgo group.
The pro-forgo group comprised the majority of the study population (ranging from 56.4% to 79.2%), indicating that most respondents intended to forgo all life-sustaining treatments under the specified clinical conditions. Similar findings have been reported in surveys conducted in other countries [4,5,6].
The neutral group consisted of individuals who didn’t have a definite preference; their choice may vary depending on the situation (ranging 8.7% ~ 14.2%). Several factors—including treatment burden, expected outcome, and the likelihood of the outcomes— can influence preferences regarding LST [19].The treatment burden is a multidimensional concept encompassing both subjective and objective aspects, such as the invasiveness, impact on health or well-being, feasibility of adherence to the treatment, potential financial cost, and the burden on significant others [20].One Korean study also found that the perception of socioeconomic burden influenced attitudes toward who should make the end-of-life decision—whether the patient or the family [21].Since the scenarios in our questionnaire were limited to outcome-related information (e.g., survival period, with or without functional or cognitive impairment), the variability in preferences observed within the neutral group was likely due to differing individual perceptions of treatment burden.
Participants in the aggressive group (ranging from 9.8% to 20.6%) preferred all active treatments across all scenarios. Notably, within this group, more individuals accepted tube feeding than artificial ventilation (18.9% vs. 9.8%). Similar findings have been reported in Japanese studies [6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23]. This suggests that participants in the aggressive group regarded tube feeding as a more acceptable intervention than artificial respiration. In many cultures, feeding is considered a form of basic care and holds symbolic and social significance [24].As a result, withholding or withdrawing feeding tubes has sparked more controversy than other LSTs [25,26,27,28].However, tube feeding is now recognized as a medical therapy that, like other treatments, should not be used regularly [29]. For patients with severe diseases such as late-stage dementia, tube feeding can cause more harm due to the complications and the potential use of physical restraints [25,26,27,28,29,30]. Nevertheless, unlike other LSTs, tube feeding in cases of terminal illness or persistent vegetative state may still be considered basic care in some cultures and religions [31].
In addition, respondents in the aggressive group were more willing to undergo LST in the context of severe dementia than in other clinical scenarios, indicating that they may not recognize "severe dementia" as an end stage of the disease. This may due to the prognostic uncertainty surrounding dementia. The disease has a unique trajectory characterized by a prolonged course from diagnosis to death, often without acute deterioration. Moreover, the cognitive impairment associated with dementia complicates clinical judgments [32, 33].As a result, accurately predicting prognosis in dementia is challenging. Patients with late-stage dementia are often more likely to receive active treatment than those with terminal cancer [33, 34].
Finally, the MND-specific pro-LST group (ranging from 8.2% to 8.8%) emerged only in the context of antibiotics and dialysis—treatments generally perceived as lower burden. Aside from their strong preference for these two interventions in MND scenario, this group’s overall treatment preferences were similar to those of the pro-forgo group. MND is less prevalent than cancer, dementia, or coma. Patients suffering from these diseases gradually lose physical function until paralyzed completely, yet retain full cognitive function. Given that this state can persist for a prolonged period,, the desire for low-burden treatments to sustain life may be reasonable, as patients can still communicate meaningfully. This group is therefore likely composed of individuals familiar with the nature of MND.
Being in the pro-forgo group was associated with specific demographic and social characteristics. Individuals who were older, had higher levels of education, and reported better quality of life were more likely to support forgoing life-sustaining treatment in all clinical scenarios. In contrast, being male, unmarried, currently not working, or reside outside northern Taiwan were associated with a lower likelihood to be in the pro-forgo group, suggesting these individuals may prefer receiving at least one form of LST in the given scenarios.
This study found that gender and age were influential factors in preferences for LST, consistent with previous findings. Most studies have reported that older individuals and women are more likely to decline LSTs [4,5,6, 22, 23, 35, 36]. However, a study conducted in Singapore reported contrary result for women [35]. A Dutch national survey indicated that individuals with higher educational attainment were more likely to refuse CPR and ANH in cases of advanced cancer and dementia [4], aligning with our findings.
Although some Taiwanese studies have indicated that lower socioeconomic status—measured through occupational categories and income—is associated with more aggressive care in terminal cancer patients [37,38,39,40], our study found no such association. This discrepancy may be due to the use of health insurance claims data in previous studies, which do not necessarily reflect patients’ preferences. Moreover, Taiwan's National Health Insurance program enables individuals to access affordable health care, potentially reducing the influence of financial concerns on treatment preferences.
Our study found that self-rated quality of life, being unmarried, and currently not working were significant factors. A review article from the United States noted that among racially or ethnically diverse groups, African Americans tend to prefer life support and generally report lower trust in the healthcare system [41].Although further research is required, we suggest that these factors may be link to individual’s trust in the healthcare system and broader society. Respondents who rated their quality of life positively may have more favorable personal experiences with their environment, fostering great trust and social connections. Conversely, those who are unmarried and currently not working may have fewer social interactions, increasing the risk of perceived social isolation (loneliness), which is known to be a risk factor for feeling unsafe and distrusting the environment; consequently, they will behave more defensively and self-protectively [42, 43].
A regional difference was also observed in preference for tube feeding. Respondents living outside of northern Taiwan were more likely to favor nasogastric tube use. Cultural beliefs may play a stronger role in shaping perceptions of tube feeding. In Taiwanese culture, having a sense of food satisfaction concerns whether a person can die without regret; otherwise, the dead may become tragic starving souls [44].In Taiwan, the legitimacy of withholding or withdrawing tube feeding as a form of LST wasn't acknowledged until the enactment of the Patient Right to Autonomy Act. Individuals residing in or near the capital region (northern Taiwan) may be more attuned to recent legal developments, which could explain the observed regional differences. However, we expect this gap to narrow over time as public awareness increases.
This study has several limitations. First, because the telephone survey included only landline users, the average age of respondents was relatively high (53.9 years), with over 40% being retirees or homemakers. Second, although we provided concise descriptions and explanations for each disease scenario, respondents may still have found it difficult to fully understand the medical conditions. Third, as the study relied on hypothetical scenarios to assess people's preferences, the findings may not fully reflect real-world decisions—despite prior studies suggesting that preferences for LSTs can be consistent, especially among individuals who have expressed a wish to forgo treatments [45,46,47]. However, whether these hypothetical preferences translate into actual clinical behavior remains uncertain [48].
A major strength of this study is the use of latent class analysis as the primary statistical method. This approach allows for the identification of unobserved subgroups within the data and enables the analysis of associated factors at the group level than the individual level.
Most people expressed a consistent intention to refuse LSTs in clinical conditions perceived as incurable or associated with extremely low physical or cognitive function. This finding suggests that the advance decision established under the Patient Right to Autonomy Act, enacted in 2019, may effectively respond to public needs. However, despite its potential to help individuals avoid unwanted care in the future, the majority of Taiwanese adults haven’t yet signed this legal document. Policymakers should prioritize investigating the barriers to the uptake of advance decision and develop strategies to ensure equitable and accessible resources for those who wish to complete them.
Moreover, our analyses identified several distinct preference patterns within the population, indicating that individuals can be categorized into several groups based on their attitudes toward LSTs. For the majority, the preference to forgo LST remained consistent across various clinical conditions and treatment types. This raises the question of whether the current standardized process for making advance decisions, which involves a lengthy (60–90 min) session with a physician explaining all five clinical conditions and requiring separate decisions for each, is necessary for everyone. Healthy individuals may primarily need the opportunity to reflect on end-of-life issues and express a general preference regarding LSTs. In contrast, older adults or those with chronic diseases may require more condition-specific information. A tiered approach that tailors the advance decision process to individuals at different life stages may present a more efficient and practical solution.
The datasets used and/or analyzed during the current study are available from the corresponding author, Duan-Rung Chen, upon reasonable request (email:[email protected]).
- AD:
-
Advance directive
- ANH:
-
Artificial nutrition and hydration
- CAPI:
-
Computer-assisted personal interviewing
- CPR:
-
Cardiopulmonary resuscitation
- DNR:
-
Do-not-resuscitate
- LST:
-
Life-sustaining treatment
- MND:
-
Motor neuron disease
- NG:
-
Nasogastric tube
Not applicable.
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The survey was funded by the National Taiwan University Hospital, grant number NTUH.108-S4390 (The preference of life-sustaining treatment of Taiwanese people) and this study was supported by the National Science and Technology Council, grant number 109–2511-H-002–016-MY3 (Withhold and withdrawal of life-sustaining treatment in patients with permanent vegetative state and minimally conscious state), and grant number 113–2410-H-002–067-SS2 (Enhancing Societal Readiness for Advancing Advance Care Planning Culture). This study was also supported by the Population Health and Welfare Research Center from the Featured Areas Research Center Program within the framework of the Higher Education Sprout Project by the Ministry of Education (MOE) in Taiwan (grant number NTU-114L900401).
During the phone survey, informed consent was obtained verbally after the interviewer had explained the survey's purpose and confirmed the respondent's age and willingness to participate. No personally identifiable information was included. Ethical approval was granted by the Research Ethics Committee of the Office of National Taiwan University Hospital (No. 201909058RINC, 17 October 2019).
Not applicable.
The authors declare no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
Tsai, D.FC., Juang, YC., Kuo, CT. et al. Preferences for life-sustaining treatments in advance decisions: a cross-sectional survey of Taiwanese general public. BMC Med Ethics 26, 83 (2025). https://doi.org/10.1186/s12910-025-01242-0