Archives of Public Health volume 83, Article number: 161 (2025) Cite this article
- HIV-related neurocognitive disorders are a growing public health issue, especially in older people living with HIV/AIDS (PLWHA). The aim of this study is to evaluate the relationship between cognitive performance and route of HIV transmission in an older group of PLWHA.
- In this cross-sectional study, conducted between November 2022 and July 2023, we enrolled PLWHA aged 50 years or older, treated with highly active anti-retroviral therapy, and with a low/undetectable viral load. Cognitive assessment was performed with HIV Dementia Scale.
In total, 268 subjects were enrolled. Cognitive impairment was present in 20.9% of the participants. According to a logistic model, people who contracted HIV through sexual transmission had 74% lower odds of cognitive impairment compared to those who contracted HIV through intravenous substance use (OR: 0.26, 95%CI 0.12–0.56). The adjustment for confounders confirmed lower odds for sexual transmission (OR: 0.27, 95%CI 0.12–0.60).
The route of HIV transmission is potentially associated with cognitive impairment in PLWHA, with patients infected via intravenous substance use being at higher risk.
Text box 1. Contributions to the literature | |
|---|---|
• This is one of the few studies in the literature that highlights the possible role of HIV transmission route in influencing cognitive performance in a large group of older people living with HIV. | |
• This study supports the need for early neurocognitive screening in people living with HIV, together with psychiatric and immunological assessments. | |
• This study identifies as a high-risk subgroup for cognitive impairment individuals with a history of intravenous substance use, informing targeted public health interventions. |
HIV-associated neurocognitive disorders (HAND) are an increasingly significant public health concern. Although highly active anti-retroviral therapy (HAART) has significantly increased quality of life and life expectancy of people living with HIV/AIDS (PLWHA), HAND remain a common finding, especially in older patients [1,2,3]. These disturbances encompass a range of impairments, from mild deficit to severe dementia, negatively influencing quality of life, everyday activities and autonomies [4, 5]. The underlying mechanisms contributing to cerebral damage in PLWHA are likely multifactorial. Studies suggest that this damage derives from a direct viral damage, together with the immune response to HIV infection [6]. Also, although HAART has surely revolutionized the treatment of the infection by reducing viral load and dramatically improving PLWHA’s prognosis, the prevalence of HAND has not decreased proportionally. This discrepancy suggests the influence of other mechanisms beyond viral load [7, 8]. Several factors have been studied as potentially associated to the risk of HAND, such as the individual immune response, co-infections, comorbidities [9], and advanced age [10, 11]. Also, genetic predisposition can play a role in HAND susceptibility [12, 13], as well as psychiatric concerns, such as depressive mood [14]. The possible impact of the route of HIV transmission has received less attention in the literature. Very few studies have investigated it as a possible determinant of cognitive deficit, much less in elderly population, and for these reasons, there is no global consensus yet [15, 16].
This gap highlights the need for more research, given the current epidemiological background.
The aim of this study is to evaluate if cognitive performance of a group of older PLWHA are related to the route of HIV transmission.
Cross-sectional study.
PLWHA aged 50 years or older, consecutively evaluated at the Immunology Unit of the University Hospital of Monserrato, Cagliari, Italy, between November 2022 and July 2023 were included. Inclusion criteria required patients to have a duration of HIV infection of at least 10 years, be under HAART, and have a current viral load < 500 RNA copies/µl [17,18,19]. People younger than 50 years, with a duration of HIV infection of less than 10 years, with a detectable HIV-RNA levels ≥ 500 copies/µl, who did not complete the cognitive assessment for any cause, or who did not provide informed consent were excluded.
Considering confidence level: 95%, confidence interval: 5%, anticipated prevalence (P): 0.5, Z-score (z): 1.96, and error margin (e): 6%, the final sample (N) should consist of at least 267 subjects, according to the formula:
$$\:N=\:\frac{{z}^{2}*P\:(1-P)}{{e}^{2}}$$
The enrolled subjects were evaluated for:
The enrolled subjects also underwent a blood venous sampling to test:
The Shapiro-Wilk test was used to assess normal distribution of the variables. The variables were presented as medians and interquartile ranges (IQRs) or as frequencies (%), where appropriate. Categorical variables were compared with the chi-squared test.
In order to group the sample, we considered HDS scores: “absence of cognitive impairment” for scores > 10, and “cognitive impairment” for scores ≤ 10 [20]; PHQ-2 scores: “absence of depression” for scores < 3, and “depression” for scores ≥ 3 [23]; route of HIV transmission: use of intravenous substances, sexual, mixed or unclear. In detail, the latter group included all participants for whom a clear single transmission route could not be determined.
Cognitive impairment was used as the dependent variable in logistic regression models, with the route of HIV transmission as the independent variable. Their results were expressed as Odds Ratios (OR), and 95% Confidence Intervals (95%CI). The control of confounding effects was studied prior directed acyclic graph (DAG), designed according to the previous literature on the topic. Finally, age, depressive symptoms, cholinesterase, and CD4+/CD8 + T-cell ratio were considered as potential confounders. The goodness of fit of the regression models was expressed with the area under the ROC curve (AUC).
The results are reported indicating p-values in reference to 95%CI.
RStudio software (version 2024.12.0 + 467) was used for the statistical analysis.
According to the inclusion criteria, we analyzed data from 268 subjects with HIV infection under effective HAART regimen, aged 50 years or older. The median age was 58 (IQR 55–62), and most of the subjects were male (163 subjects, 60.8%). The control of HIV infection was demonstrated by the current CD4 + T-cell count, the median of which was 756/µl, and a median CD4+/CD8 + T-cell ratio greater than 1. In total, 97 subjects (36.2%) acquired HIV infection through intravenous substance use, 121 (45.1%) through sexual transmission, and the remaining 50 subjects (18.7%) through other causes, or due to multiple causes simultaneously. Women more commonly acquired HIV infection through substances use (49.7%), while men through sexual transmission (61.0%). According to HDS, 56 subjects (20.9%) were found to have.
cognitive impairment, especially men (26.4%, vs. 12.3% among women, p = 0.009). According to PHQ-2 scores, 201 subjects (75.0%) reported depressive symptoms within the past two weeks, without significant sex- (p = 0.220) nor cognitive impairment-related differences (p = 0.386). Additional characteristics of the enrolled subjects are detailed in Table 1.
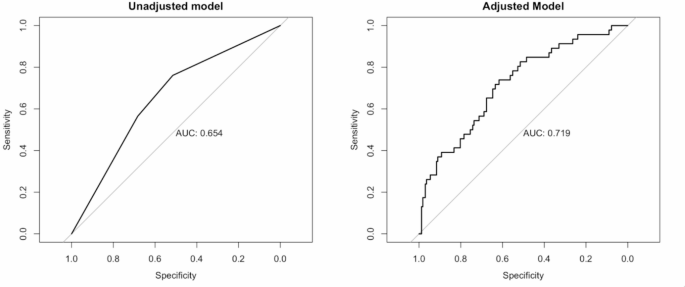
The sample was divided according to HDS scores in two subgroups: those with cognitive impairment (made up of the aforementioned 56 subjects), and those with adequate cognitive capacities (the remaining 212 subjects). This dichotomized variable was used as the dependent variable in a logistic regression. Its independent variable was the route of HIV transmission. The use of intravenous substances was considered as the reference. The unadjusted model (AUC: 0.654, see Fig. 1) showed that people who contracted HIV via sexual transmission had 74% lower “odds” of having cognitive impairment compared to people who contracted HIV through substances use (OR: 0.26, 95%CI 0.12–0.56), as displayed in Table 2. People who contracted HIV through other routes were also less likely to have cognitive impairment, but the CI of the OR crossed the null effect line (OR: 0.66, 95%CI 0.26–1.55), indicating less certainty in this result, as displayed in Table 2. In order to control the model for potential confounders, we designed the appropriate DAG, based on the literature on the topic, and age, depressive symptoms, CD4+/CD8 + T-cell ratio, and cholinesterase were considered as potential confounders (see Supplementary material, Figure S1). We performed, therefore, the adjusted regression (AUC: 0.719, see Fig. 1), which confirmed the lower probability to have cognitive impairment among people who contracted HIV through sexual transmission (OR: 0.27, 95%CI 0.12–0.60), as displayed in Table 2.
Goodness of fit of regression models designed to explore the role of HIV transmission on cognitive impairment. AUC, Area Under the ROC Curve
Thanks to the advent of new HAART, the life expectancy of PLWHA has increased. However, new challenges have emerged, one of the most significant being HAND, that represents a significant public health issue [2]. Neurocognitive deficits are common among PLWHA, particularly when the infection is not adequately treated. However, even individuals with well-controlled viral loads remain at risk [1, 2, 14]. Understanding the factors that influence these disturbances remains a key priority for scientific research. In this context, the current study aimed to explore the role of HIV transmission route as a potential factor influencing cognitive performance in older PLWHA. In our study, we examined 268 PLWHA, all of whom had achieved viral load control [17,18,19]. About 21% of them showed cognitive impairment, a prevalence that partially aligns with the scientific literature, falling at the lower limit. In detail, a recent meta-analysis on the topic showed that the prevalence of asymptomatic impairment is around 23.5%, while the prevalences of mild and major neurocognitive disorder settle around 13% and 5%, respectively [26]. A relevant aspect emerging from our research is the significant difference in the likelihood of showing cognitive deficit based on the route of HIV transmission. Specifically, individuals who contracted the infection through the intravenous substance use showed a significantly higher probability compared to those who contracted the infection through sexual transmission. It should be noted that our study also encompassed patients for whom a definitive single transmission route could not be identified, reflecting the inherent complexity and overlap of transmission mechanisms in real-world settings. This classification acknowledges that, despite best efforts, certain cases do not fit neatly into exclusive categories due to mixed exposures or ambiguity in patient history, thus making this group a necessary and justified category for accurate representation of the sample. Although no universal agreement has been reached on the relationship between cognitive impairment and HIV transmission, our results are supported by previous studies on psychiatric depression impairment in PLWHA [27], that showed higher risk of depression in people with a history of intravenous substance use. Several studies documented the harmful impact the use of substances to neuroinflammation, since chronic inflammation and substances-mediated neurotoxicity may boost the direct brain damage caused by HIV [28]. Neuroinflammation, in turn, exacerbates HIV-related neuronal damage [29, 30]. Other factors may also be called into account. For example, the higher comorbidity burden that affects individuals who use intravenous substances [31, 32], or even the later seek for medical care compared to subjects who contracted the infection through other routes [33]. Also, substance use is usually related to lower education and income, together with a general socioeconomical instability, that may in turn negatively affect the cognitive-affective sphere [34, 35]. Conversely, the relationship between high-risk sexual behaviors and neuropsychological outcomes has been studied in the opposite direction. In fact, scientific studies showed that neuropsychological dysfunctions are usually associated with risky sexual behaviors [36, 37]. Our findings have been further confirmed by the multivariable analysis, which controlled for potential confounding variables, including age, depression, liver function (as indicated by cholinesterase) and immunological status (as indicated by CD4+/CD8 + T-cell ratio). Previous research has identified these factors as potential contributors to the risk of developing cognitive impairment, reinforcing the need for a comprehensive approach in this population [14, 38,39,40,41,42].
Our study examined a sample of older PLWHA with a relatively large size compared to studies with a similar design, and we believe that this is a significant strength of the study, together with the multidimensional assessment of the participants, not limited to the mere cognitive evaluation, but encompassing also psychiatric, functional, and immunological factors. Also, to the best of our knowledge, this is the first study with this design and these outcomes conducted on a population of PLWHA of such advanced age. We also acknowledge some limitations, such as the lack of a formal diagnosis, since we only relied on the impairment deriving from HDS scores. Indeed, it has been demonstrated that HDS shows good specificity in detecting cognitive impairment, but also an overall moderate sensitivity [43, 44], and it may have limited the precision of our stratification. Also, a longitudinal design would have allowed us to track cognitive changes over time, helping us to draw specific profiles of the cognitive decline progression. Moreover, we were not able to perform a complete assessment of inflammatory biomarkers. Including them in our logistic model would have enriched the quality and the robustness of our findings. Finally, the relatively low prevalence of cognitive impairment in our population, together with the monocentric nature of the study limits the generalizability of the findings, especially due to cultural and healthcare system differences. It highlights areas for future multicentric research, all the more so because of the lack of studies with similar design in the scientific literature so far.
In conclusion, our results support the hypothesis that the route of HIV transmission may be related with cognitive deficit in older PLWHA. Specifically, early assessment of cognitive function, especially in people with a history of intravenous substance use, should be prioritized. Future research should aim to deepen the neurobiological mechanisms underlying these differences, in order to develop personalized intervention tailored to mitigate the risk of cognitive disfunction.
No datasets were generated or analysed during the current study.
- AIDS:
-
Acquired Immuno-Deficiency Syndrome
- ADL:
-
Activities of Daily Living – Katz Index
- AUC:
-
Area Under the ROC Curve
- CI:
-
Confidence Interval
- DAG:
-
Directed Acyclic Graph
- HAART:
-
Highly Active Anti-Retroviral Therapy
- HDS:
-
HIV Dementia Scale
- HIV:
-
Human Immunodeficiency Virus
- IADL:
-
Instrumental Activities of Daily Living
- IQR:
-
Interquartile Range
- OR:
-
Odds Ratio
- PHQ-2:
-
Patient Health Questionnaire – two items
- PLWHA:
-
People Living With HIV/AIDS
- TSH:
-
Thyroid Stimulating Hormone
Not applicable.
This research received no external funding.
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of the University of Cagliari (protocol code PG/2022/4078, 9 November 2022). Informed consent to participate was obtained from all subjects involved in the study.
The manuscript does not include any individual person’s data.
The authors declare no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Salis, F., Belfiori, M., Ortu, F. et al. Is there a relationship between the route of HIV transmission and cognitive performance in older individuals living with HIV?. Arch Public Health 83, 161 (2025). https://doi.org/10.1186/s13690-025-01657-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13690-025-01657-6