Harm Reduction Journal volume 22, Article number: 106 (2025) Cite this article
Drug consumption rooms (DCRs) are harm reduction facilities providing safer and hygienic setting for supervised administration of drugs aimed at decreasing negative health and social consequences of drug use. The first DCR in Czechia was opened in September 2023 in city of Brno in a mobile form operating in a socially excluded area (SEA). A research project informed the implementation of the DCR.
A mixed methods design was applied in the following phases: desk review, research before and after the launch of the mobile DCR, and routine monitoring of programme performance. Two cross-sectional questionnaire surveys among PWUDs (n = 131 and 135), ethnographic observation, focus group (n = 19), interviews with PWUDs (n = 26 and 19), with personnel of addiction services and local officials (n = 16 and 12), and residents (n = 7 and 6) were performed prior to and after the launch of the DCR. Thematic analysis of qualitative data, descriptive and regression analyses of quantitative data were performed.
There was a need and high willingness to use the DCR among potential clients. The significant predictors were opioid use (adjusted odds ratio, AOR = 3.4 in survey 1 and 3.9 in survey 2), drug injection in the last 30 days (AOR 4.3 in survey 1), being in the probationary period during the previous 30 days (AOR 10.0 in survey 1), witnessing an overdose in the past 30 days (AOR 8.5 in survey 2), HCV positivity ever in life (AOR 2.9 in survey 2), living in SEA (AOR 2.7 in survey 2) and Roma ethnicity (AOR 2.8 in survey 2). The beginnings of the DCR were relatively slow with low initial number of clients and drug administrations. However, with time, and programme adjustments following research results, the attendance at the facility has grown.
Research was instrumental in shaping the DCR in Brno before and during its implementation. The DCR showed a potential to attract the most vulnerable PWUDs from SEA. Despite a slow start, the DCR has become an integral part of low-threshold services for PWUDs in Brno and has proven its feasibility in the Czech settings.
Drug Consumption Rooms (or Safer Injecting Sites, Supervised Injection Facilities) are services where people can use their dose under the supervision of staff in safer and hygienic conditions and where they receive counselling and other services to prevent overdose and drug-related risks [1]. The Drug Consumption Rooms (DCRs) belong to strategies and activities aimed at reducing the risks and harms of substance use, which are referred to as harm reduction, such as needle and syringe programs, opioid agonist treatment, testing and linkage to care, drug checking programmes etc. [2, 3].
The target population of the DCR service are people who use drugs (PWUDs), particularly those who use them by injection (PWIDs) and those who smoke or inhale them; especially those marginalized with high-risk behaviours who use drugs in public and/or in unsafe and risky conditions. The main objective is to reduce mortality and morbidity through safer and more hygienic drug administration. Furthermore, these facilities aim to minimize drug-related public nuisance and to facilitate the clients’ access to other health, social, and addiction treatment services and to support their social functioning and integration [4]. DCRs are, along with take-home naloxone programmes, among the harm reduction interventions recommended particularly to avert fatal overdose [5], but they are also in the context of other harm reduction interventions recommended as one of the core interventions in reducing risky injecting behaviour and, as a consequence, the risk of transmission of blood-borne infectious diseases [6].
The available evidence shows that injection rooms significantly reduce the risk of injection-related skin lesions, emergency health issues and overdoses [7], including fatal overdoses [8], lead to a reduction in risk behaviours such as sharing needles and syringes when injecting drugs [9], and thus contribute to reducing the risk of blood-borne infections. They increase rates of individual’s engagement in addiction treatment and other treatment and care [8, 10], reduce crime [11], in particular petty crime such as car break-ins and thefts [12], reduce rates of public injection, and increase safe disposal of used syringes [13]. Conversely, when the injection room lacks capacity, such as if its hours are limited, or if it is located far from the drug scene, the effect on reducing consumption in public seems limited [14]. DCRs appear to be inexpensive and cost-effective [15, 16]; in particular, there are savings through reduced healthcare costs associated with reducing overdose and other comorbidity [17]. In addition, research to date has not indicated any increase of risk or harm related to DCR use. [1, 14].
DCRs have been operating in Europe for three decades, with approximately 100 DCRs currently operating in 13 European countries [18, 19]. In addition, DCRs are operated in Australia, Mexico, the USA or Canada [20], where, as of 2019, DCR also operate in prison settings [21, 22]. There are different models of DCRs ranging from integrated services where supervised consumption is one of several harm reduction interventions offered, to specialized services offering supervised consumption only. They can have a mobile form in vans or ambulances that provide flexible deployment of services in different locations but have limited capacity [1, 4]. Typically, there are rules laid out, which are similar across various DCRs such as prohibition of dealing drugs in DCR and near it, prohibition of aggression towards staff or other clients, of administration of the drug anywhere else than in designated places and prohibition of assisted injection or helping each other with administration [23].
In September 2023, a mobile DCR in Brno has opened, which is the first official DCR in Czechia ever. However, attempts to introduce DCRs in the Czech Republic began in the late 1990s, when the Prague 1 municipal district commissioned a report on DCRs [24] and started discussing their establishment in light of a series of fatal heroin overdoses. However, the proposal was rejected in 2001 [25, 26]. The debate on the DCRs was again stirred up in 2009 and 2010, when strategy to address open drug scenes in the centre of Prague was discussed [27, 28]. And finally, there was another unsuccessful attempt to establish DCRs in Prague in 2013 and 2014, when the DCR establishment plan became part of the municipal strategy for development of social services and of the Prague’s drug policy strategy [29,30,31].
The concept of the DCR in Brno has been drawn up by NGO Společnost Podané Ruce in cooperation with the Brno City Council and the Brno-North Municipality since autumn of 2021. In 2022, after consultation with the local authorities, Podané Ruce started the preparation of the DCR in the form of a mobile unit [32]. The project implementation team established a working group composed of representatives of the local and state government, including the police and the municipal police, social, health and addiction services and representatives of people who use drugs. The working group held regular meetings between June 2023 and June 2024 with a meeting frequency of once per 1–3 months. This working group was instrumental in fine-tuning the details of the programme. The DCR in Brno was launched on the 19th September 2023 [33]. It is implemented in a mobile form in a former ambulance. Initially, due to limited budget, it was opened only 2 h every working day. The site, where mobile unit operates, is the same site every day located in the centre of Brno, where there is an open drug scene in a socially excluded area (SEA) called “Cejl”. DCR cooperates with other two mobile units of the outreach programme which are in its vicinity and provide other services, such as basic medical treatment, first aid in the event of an overdose, infectious diseases testing, naloxone distribution, addiction counselling and referrals to other social and health services where necessary [34].
At least two staff members are present in the DCR during each shift. The DCR is composed as a low-threshold service, i.e. the anonymity of the clients is secured. As a condition for a client to enter the DCR, he/she must sign an informed consent acknowledging the basic rules of the DCR, which are: to be aged over 18 years, to be a client of the Podané ruce’s outreach programme and to have previous injecting experience ever in life. As a precautionary principle, during the first four months of the project only one client was allowed to use the service at a time. Since January 2024, 2 clients can use the DCR at the same time since there are 2 permanent places in the mobile unit. Trafficking (distribution) of substances between clients is not allowed in the premises of the DCR or in its immediate surroundings and so is exhibiting verbal or brachial aggression towards the staff, other clients or oneself or endangering others in any way. It is forbidden for staff to help with the application itself, and help with the application is also forbidden between clients. It is also strongly recommended to enter the DCR with only one dose of the drug intended for single use. Sterile syringes and other paraphernalia are made available to the client and safely disposed of after administration. Clients are allowed to chill out post-drug administration and leave when they are fully conscious [34]. These rules were set by the programme itself since so far there are no nationally binding guidelines.
The introduction of the DCR in Brno was subject to formative research performed prior to and during its inception phase. This paper describes design, process and results of this research and feeding these results back including their implementation in practice.
An evaluation project to assess the needs and implementation of the DCR was designed [35]. The main objective of the project was to evaluate its process and impact and to map the factors decisive for setting up the DCR programme in Brno. The original protocol comprised the following phases: (1) desk review, (2) cross-sectional research prior to the introduction of the mobile DCR, (3) follow-up study on a sample of clients of the DCR, and (4) routine monitoring of performance of the programme. However, in contrast to the original protocol, the follow-up study was abandoned so as not to pose further obstacles for the clients exacerbating DCR's slow start (see more in the Discussion section), but instead another cross-sectional questionnaire survey was conducted.
So finally, project was organised as follows: (1) desk review, (2) cross-sectional research prior to- and (3) after the launch of the mobile DCR, and (4) analysis of the routine programmatic data. In the two cross-sectional studies, a mixed methods design was used, combining several quantitative and qualitative methods [36, 37]. The qualitative element consisted of ethnographic observations at the location, a focus group, and structured interviews with clients, professionals (including four co-authors of this paper who work directly with clients) and residents of the DCR location. Team of qualitative research consisted of the senior researcher and two interviewers, all of them participated in data collection and analysis. Quantitative research consisted of two cross-sectional questionnaire surveys (pre- and after the launch of the DCR) among PWUDs and processing of the routine records of the programme. Research tools were prepared in consultation with broad group of interviewers with participation of collaborating peers.
Published and grey literature from 2022 and 2023 on the prevalence and patterns of drug use in Brno, on the characteristics of PWUDs and clients of the drug services and on the services provided in city of Brno was reviewed between May and September 2023.
The pre-implementation research was conducted between July and September 2023 and included a cross-sectional survey (survey 1), a focus group, a set of qualitative interviews and an ethnographic observation.
The survey was carried out on a sample of 131 PWUDs. The sample was obtained by means of convenience sampling, among clients of collaborating low threshold services, with elements of snowball sampling and using recruitment by collaborating peers. The questionnaire covered the following areas: socio-demographic data, client's social situation (housing, work, financial situation, family), drug use patterns, risk behaviour including risky injecting practices, health, service utilization, social functioning and legal problems, and opinions and attitudes towards the DCR such as perceived need, or rating of importance of various elements of the programme. The questionnaire consisted of approximately 80 items and was administered by interviewer using the paper-and-pencil method (PAPI). No incentive was provided to respondents. The administration of the questionnaire took approx. 30–60 min. In total, 6 interviewers participated in the data collection.
The qualitative part consisted of a focus group (19 participants—members of the DCR working group), interviews with personnel of social and addiction services and local officials (16 participants), interviews with clients (26 participants), interviews with residents of the planned location of DCR (7 participants) and ethnographic observations of the location, organised around the timing of the interviews. The interviews were not recorded, the interviewers took notes during the interview and a transcript was created after the interview. The ethnographic observation consisted of two visits of the area, observations on the streets, in public spaces such as bars, restaurants, shops, and informal interactions with locals and traders. A short report was produced of each visit.
A cross-sectional survey (survey 2), series of qualitative interviews and ethnographic observation were carried out after the launch of the DCR.
The survey was conducted in February and March 2024 on a sample of 135 respondents – clients of harm reduction services in the city (of them, 46 clients of two methadone centres, 68 of a drop-in centre, and 21 of an outreach programme). Participation in the survey 1 was not an exclusion criterion, however repeated participation was not documented. The questionnaire consisted of 30 items administered by PAPI and included the following sections: socio-demographic data (gender, age), drug use, injecting use, risk behaviour and health incidents in the last month, HIV and HCV testing and treatment, relationship to the location, self-reported belonging to the Roma community, awareness of the existence of the DCR, willingness to use the DCR and reasons for possible non-use. A small incentive (a chocolate bar) was provided to the respondents. The administration of the questionnaire took approx. 15–30 min. Two interviewers participated in the data collection.
The qualitative part was conducted from October 2023 to April 2024 and consisted of ethnographic observation of the DCR location, interviews with clients (19 participants), personnel of social and addiction services, local officials (12 participants) and residents of the location (6 participants). The interviews were not recorded, the interviewers took notes during the interview and a transcript was created after the interview. The ethnographic observation consisted of two visits of the area, observations on the streets, in public spaces such as bars, restaurants, shops, and informal interactions with locals and traders. A short report was produced of each visit.
The analysed period spans from 19 September 2023 to 30 June 2024, which is approximately 9.5 months. The data was collected using the Podané ruce’s established monitoring system of clients and services and consisted of client intake records and daily reports of provided services. Number and characteristics of clients and their drug administrations at the DCR (gender, age, substances used, method of administration) were aggregated by months.
Thematic analysis was used in analysing the collected qualitative data, all three researchers collecting qualitative data were involved. The production of an analytical report from both waves of qualitative research was an iterative process with participation of an additional member of the core coordination team. In case of quantitative data, descriptive statistics were applied, bivariate associations were explored between the intention to use the DCR and the predictors by means of Chi-Square for categorical variables and t-test for quantitative variables. Finally, adjusted ORs were calculated in logistic regression models predicting the intended DCR utilisation, while adjusting for basic demographic variables (sex and age).
There were 2200 people who inject drugs (PWIDs) estimated in Brno in 2018, of which 1900 used methamphetamine and 400 opioids as their primary drug(s). Over 1500 of PWUDs were estimated to be in an unstable housing situation, and 500 were estimated to live with chronic hepatitis C [38, 39].
Altogether, there were recently estimated up to 5,000 people with high-risk use of drugs or alcohol to live in socially excluded areas of the city of Brno, where open drug scenes are also present [38, 40]. The spatial distribution of high-risk drug use, including drug use in public, is specific in Brno. It is concentrated in the immediate vicinity of the historical city centre in a socially excluded area (SEA) called “Cejl” (Bratislavská, Cejl, Francouzská, Tkalcovská and adjacent streets), where there is also a high representation of Roma community members among the inhabitants. In 2022, 9820 used syringes were collected in public spaces only in this area [34].
Low-threshold services for PWUDs/PWIDs operating in Brno include two drop-in centres, one of which is run by the Roma centre DROM (located in Cejl), and the other by the NGO Podané ruce (located outside of Cejl). Outreach programme for PWUDs/PWIDs is run by Podané ruce in Cejl. It provides harm reduction services such as needle and syringe programme, distribution of condoms, overdose prevention including take-home naloxone, infectious diseases testing and linkage to care, social and health counselling, basic medical interventions, referral to other health and social services, provision of food, hygiene, and clothing. Approximately 2500 clients are in contact with various low-threshold programmes annually (however, individual clients of different programmes are overlapping). They are typically aged between 18 and 45, on average 35 years old, and approximately one-third of them are women [38, 40]. In addition, 2 opioid agonist treatment programmes are present in Brno operated by Podané ruce (one of them in Cejl) with a total of 250 clients annually [41]. The peer group Street Support organized within Podané ruce is involved in harm reduction services such as secondary needle exchange, distribution of naloxone (nasal spray is used in Czechia) and in linkage to (HCV) treatment. Moreover, it operates a fixed container for disposal of used syringes installed in 2019 in Cejl [38, 40]. The main primary drug of PWUDs in Brno is methamphetamine (historically called “pervitin”), which is predominantly injected, and often used within a polydrug-use pattern together with alcohol, cannabis, benzodiazepines and other psychoactive substances including opioids. Opioid use is largely concentrated in Cejl among the Roma community. The outreach programme operating in this location reports a higher proportion of heroin and other opioid users (such as fentanyl or morphine from medical preparations) and a higher proportion of Roma clients for whom opioid use is typical. In 2021 and 2022, the outreach program had over 850 clients annually. Drug injecting in public and signs of drug injecting (such as dropped needles and syringes) in Cejl are noted by the police and local inhabitants [32].
Between October 2022 and March 2023, a field survey with 60 clients of harm reduction programmes in the location was conducted focusing on drug use in public places and attitudes of clients toward a (future) DCR. The survey confirmed high prevalence of injecting in public places including the public toilets located within the premises of a local supermarket. Clients living in Cejl confirmed an interest in using the DCR, ideally combined with counselling, distribution of syringes and injecting paraphernalia, basic medical treatment, food and refreshments, and a safe place to rest [32].
Questionnaire surveys
Both survey samples (the first one finished in the calendar month when DCR was launched with n = 131, the second one started 5 months after the launch with n = 135) consisted of demographically similar populations: 2/3 men, average age around 37 years (36.5 in the first sample and 37.5 in the second one). In the second sample, there were more persons considering themselves to be of Roma ethnicity (50.7% versus 20.3%) and more persons whose primary drug were opioids (39.7% versus 27.5%). See Tables 1 and 2 for detailed results.
Both samples displayed characteristics of social exclusion and a range of risk behaviours. In the first sample, collected before the launch of the DCR programme, additional data were available, showing that only about one third of the respondents had a stable housing situation, one third did not own a health insurance card (necessary to obtain health care beyond first aid in Czechia) and 20.8% did not own an ID card. Most injected drugs in their lifetime (89.2%) and approximately three quarters injected them in the last 30 days. One third (31.9%) reported sharing needles or drug injecting paraphernalia in the last 30 days (additional 6.4% did not remember whether they shared or not). Majority (73.3%) did not use a condom during their last sexual intercourse. As many as 14% overdosed and 28.2% witnessed an overdose in the last month. Vast majority of the respondents of the first survey ever injected in public, and 77.8% did so in the last 30 days, 13.4 times on average.
In the second survey, 72.5% injected drugs, 6.0% shared needle or paraphernalia, 3.0% overdosed, 7.5% witnessed overdose, 10.4% called emergency ambulance, and 45.9% injected in public in the last 30 days (of those who injected in the last 30 days, two thirds used in a public place).
Regarding specific questions on DCRs, two thirds (67.5%) of the sample before the programme introduction were aware of what a DCR is and what services it offers. Majority (75–89%) would consider important the following factors when using a DCR (in descending order): cleanliness, discreetness, safety, staff’s attitude, geographical accessibility, temporal accessibility, and equipment provided. In both surveys, approximately half of the respondents expressed willingness to utilize services of a DCR. After the programme introduction, 61.5% were aware of its operation, but only 3.0% (4 respondents) used it. The most commonly reported reasons for lack of interest in using the DCR were having another preferred place of injection, finding it unpleasant to be supervised during drug injecting by a stranger and unsuitable location for the respondent.
Variables associated in bivariate analyses with the expressed interest in using the DCR across the two samples were similar: injecting in the last 30 days, using opioids, lifetime HCV positivity, having received an HCV test in the last 12 months, being in a probationary period in the last 30 days and considering oneself of Roma ethnicity (p < 0.01) and not owning an ID, being tested for HIV in the last 12 months, not using any services in the last 12 months, living near the DCR location and having witnessed an overdose in the last 30 days (p < 0.05). In the first survey, using methamphetamine was also a predictor of interest in DCR utilization at the p < 0.05 level, however, in the second wave after DCR implementation, this was not the case and methamphetamine users were in fact less likely to be interested in utilizing the DCR.
After adjustment for sex and age in multivariate logistic regression models, the remaining significant predictors of DCR utilisation were, in the survey which preceded DCR launch: opioid or methamphetamine use in the last 12 months (AOR 3.42 and 5.00, respectively), drug injection in the last 30 days (AOR 4.25) and being in a probationary period during the last 30 days (AOR 10.00). In the survey conducted after the DCR launch, opioid use remained a significant predictor (AOR 3.87), while methamphetamine use negatively predicted the willingness of DCR use (AOR 0.29). Other significant predictors were having witnessed an overdose in the past 30 days (AOR 8.53), HCV positivity ever in life (AOR 2.93), living near the DCR location (AOR 2.66) and considering oneself to be a member of the Roma community (AOR 2.80). See Table 3 for detailed results.
Qualitative research
The neighbourhood of Cejl, historically inhabited largely by the Roma community members, has been recently going through a transformation and gentrification including developments of new housings and office facilities. Life takes place on the streets – people are engaged in walks, chats, groups, music productions, there are children around – this is a distinctive characteristic of the area. Sex work scene is also present in the area, connected to the drug scene and taking place mostly in cars.
There is a dominant heroin (opioid) scene in the area, which is linked to the Roma community. Methamphetamine, which is the most often injected drug in Czechia including the rest of Brno, is only marginally associated with the area. Typical methamphetamine user from Brno avoids the neighbourhood, unless they have a good reason to be present.
Heroin of low purity is most commonly purchased and used in small single doses immediately after the transaction. Frequent administration and craving are among the reasons why public drug injecting is common here. Frequency of injecting during the day can be relatively high. The reported number of drug administrations per day vary widely—from a few to 20; the main reason for the unusually frequent administration is the extremely low purity of heroin distributed in the location. The reported drug administration time was from 1 to 30 min depending on the condition of the veins but also on the skills of the user. Scattered injection kits are found in the streets, parks and other places throughout the neighbourhood.
Particularly during the summer months, open drug scene is present in the local brownfield. This outdoor space often harbours several people who inject at the same time. It has multiple hideouts due to the presence of wild vegetation. Drug dealing also takes place here and there is limited access to hygiene.
Another specific place for drug injecting are public toilets in the local supermarket. This “unofficial DCR” provides a semi-public place, it is relatively spacious and clean, has optimal lighting and access to hygiene (water, soap), offering privacy and anonymity and high accessibility from 7 am to 10 pm. Access to it is largely unregulated, it is used by supermarket clients and PWIDs alike. Beside drug injecting, commercial sex and drug dealing takes place here as well, mostly inside lockable cubicles. There have not been observed or reported any conflicts between the supermarket customers and PWUDs/PWIDs. No emergency or fatal incident was reported in association to drug administration in the supermarket’s toilets.
The sample of interviewed PWUDs before the introduction of the DCR consisted of 26 clients of low threshold services (56.3% men, average age 32.9 years, 56.3% used methamphetamine and 43.8% used opioids, and all used drugs by injection in their lifetime). The majority of opioid (mainly heroin) users from Cejl expressed an interest in utilizing the DCR services. A mobile unit was deemed acceptable, and the ideal opening hours were stated as from 12 noon to 12 midnight, although some users have expressed interest in morning opening hours. Key DCR-related preferences included the need for privacy during drug administration, advice during administration (e.g. from peer workers) such as help finding a vein (it should be noted here, that an advice on locating the vein is allowed, while physical assistance with the application is not), the presence of professionals, a space to rest post-administration, testing for infectious diseases, availability of water to drink, and basic medical care (e.g., ointment for injection sites). Concerns about police interventions were also noted.
PWUDs interviewed after the introduction of the DCR consisted of 19 PWIDs who were clients of low threshold services in the area, eight of them were females. The respondents expressed correct understanding of the DCR role and services in general. However, the majority was not aware that such service was already in operation in their area, or reported incorrect information, such as the possibility of being injected by the DCR staff or the necessity to register for the service with the provision of personal data. Approximately half of the respondents were not interested in using the services of the DCR. Reasons given for the lack of interest included discomfort associated with being supervised while injecting, other preferred places used to inject oneself, while some respondents preferred injecting in public in social contact with peers. Some respondents didn’t like the placement of the mobile DCR due to its, according to them, high visibility. Concerns about insufficient anonymity and privacy were expressed. In addition, movement of the personnel inside the van causes certain rocking of the facility, which was perceived as disturbing during drug administration. Other negative factors mentioned were limited opening hours and location of the mobile DCR, which was far away from places where they usually obtained their drugs. Furthermore, some respondents felt they were experienced and well informed and thus not in need of the DCR service, which they considered suitable rather for beginner injectors.
Those interested in the mobile DCR utilization after its launch were primarily motivated by the provision of assistance and counselling in relation to drug injecting and the possibility to inject in a private, quiet and hygienic environment. However, most respondents said that they would use the service only if they would find themselves near the facility during the opening hours when planning to use their substance.
Interviews with professionals highlighted the need for collaboration within the on-site multidisciplinary team, the balance between using the DCR as a space for counselling while maintaining it as a private space for clients, and the impact of DCR on both client health and the broader community. The importance of a proactive approach in informing clients and promoting DCR among drug users in Brno was emphasized.
There were no major complains from the public against the DCR, the principle of injecting behind the door in context of harm reduction service was well tolerated by the local inhabitants.
Programmatic data
During the first 9.5 months of operation from 19 September 2023 to 30 June 2024, the DCR served 134 clients (79 males and 55 females). Of them, 68 used it for the administration of a drug (40 males and 27 females, 1 unknown). The remaining clients visited the DCR without actually using a drug inside to familiarise themselves with the place and staff and/or to use other services.
Clients self-administered the substance a total of 120 times in the DCR. Of these, 118 administrations were by injecting. Of these 120 self-administrations, 45 were in clients using the DCR just once, while remaining 75 (60.8%) were in 23 clients using DCR repeatedly. Of them 11 administered twice, 8 three times, 2 five times and 1 client used DCR 13 times. In 2 cases, an alternative administration was performed – in one case the drug was sniffed and in another case, it was administered in a gelatine capsule as a peroral alternative to injecting – see more details in Mravčík, Škařupová [42]. Opioids were used in more than half of the cases (64 heroin, 4 buprenorphine, and 4 methadone administrations). Methamphetamine was used in 48 cases (see Table 4). The sources of drugs are not determined, but it can be assumed that they all come from illicit sources, or in the case of buprenorphine and methadone, diversion from formal treatment. In 9 cases (7.6%) the injection was unsuccessful, i.e. the client was unable to inject the substance. There were no cases of intervention or need for assistance in case of overdose.
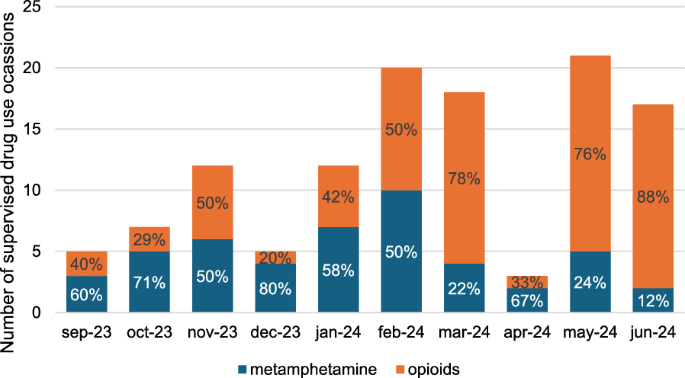
The number of administrations was gradually growing over time since the introduction of the service on 19 September 2023 and the proportion of heroin and opioid administrations has increased (see Fig. 1). The DCR service had to close for a total of 49 days (the major breaks were 3 days in September 2023, one week in November 2023 and then 3 weeks in April 2024) due to holidays and also due to technical problems related to the ambulance car and its refurbishment.
Number of drug self-administrations in the mobile DCR in Brno over time. The longest DCR service interruptions were 3 days in September 2023, 1 week in November 2023 and 3 weeks in April 2024. From 15 January 2024, opening hours were extended from 2 to 4 h every working day
The mobile DCR in Brno, launched in September 2023, is the first DCR in Czechia ever. From its beginning as a concept and project proposal, it represents a coordinated local action with involvement of all stakeholders. Formative research, reported in this paper, was an integral part of the introduction and the process of designing the DCR programme. It allowed step-by-step establishment and implementation of the programme and provided continuous feedback to the DCR project team. Findings from the different stages of the research project served as inputs for adjustment of the functioning of the DCR. On the other hand, the design of the formative evaluation research was gradually updated according to the changing reality and challenges faced during the DCR implementation.
The first important finding of our research prior the DCR launch was the existence of the need for the programme by the potential clients as well as the local community stakeholders and harm reduction services. Results indicated a high prevalence of drug injecting in public and a high frequency of injecting among PWIDs who lived in the socially excluded area in Cejl. Data has also shown a high prevalence of having experienced drug overdose and/or having witnessed one among clients of low-threshold services. This finding confirms previous findings of studies that have repeatedly demonstrated the need for DCRs among PWUDs in Czechia and their potential willingness to use DCRs’ services if they were established [30, 43, 44].
Secondly, PWUDs in Brno and especially those living in the Cejl area, largely expressed their interest and willingness to use the DCR when established. Identified predictors of the interest in DCR use, in line with its objectives and planned focus, have suggested that frequent injecting drug use, having witnessed an overdose, living in the problematic area, indicators of social exclusion, belonging to the Roma community, involvement with the criminal justice system, HCV positivity (which can be seen also as a proxy of the intensity of drug use and risk behaviours in lifetime) increase the probability of being interested in utilizing the DCR. In short, the DCR seems to attract the intended target population.
There is a substantial body of research focusing on correlates and predictors related to DCR use and on predictors of potential service use. The need to understand the demand for DCRs among PWUDs is closely related to the challenges associated with their implementation. Main predictors found to be significantly associated with willingness to use the DCR are adverse social situation manifesting in unstable housing or homelessness [45,46,47,48,49], legal problems [46, 50], health problems including infectious diseases and mental health comorbidity [45, 46, 50, 51], overdose history [49, 52], risky drug use patterns such as daily injecting or binge injecting [47], sharing needles and paraphernalia [48], public drug use and public drug injecting [45, 47, 49, 51], heroin use [48, 49, 51], belonging to a non-majority ethnic group [48, 51] and living in the vicinity of the DCR [45, 49]. In this respect, there is a fair level of similarity with the predictors found in our study.
Interestingly, opioid use was also a strong predictor of the interest in DCR utilization, while methamphetamine use was negatively associated with intended DCR use after its launch. There are two interpretations and possible implications of this finding. Opioid use is typical (though within a polydrug use pattern) for the Roma community in Brno as well as elsewhere in Czechia [53]; thus this finding may suggest that the DCR in Brno attracts the local PWUD community in the problematic area in Cejl. On the other hand, people who use methamphetamine and do not live in the problematic area might be hesitant to attend the DCR there, which is in line with the reports about two distinct drug scenes in Brno – the one in the socially excluded area in Cejl with high rate of opioid use in the Roma community and another one in the rest of Brno with predominance of injecting of methamphetamine (pervitin). This finding also suggests that if DCR in Brno city targeted the most prevalent methamphetamine injecting, it would be better suited elsewhere than in the neighbourhood of Cejl. In other words, the shift between pre-DCR introduction survey results where methamphetamine use was a predictor of interest in the DCR use and post-DCR introduction survey where it was a negative predictor, suggests a theoretical interest in this type of service among methamphetamine users but also a certain process of their expectations becoming adjusted to the reality of the introduction of the DCR in the socially excluded neighborhood of Cejl, which they do not prefer to frequent. This finding is also highly relevant for the rest of Czechia, where methamphetamine represents the predominant primary substance among PWUDs.
The above correlates of potential use of the DCR may partly explain why only 50% and 47% respondents of the first and the second survey, respectively, expressed an interest in using the DCR. Other explanations may be that DCR is a new program for PWUD in Brno, which the users have not encountered before (there were 30% of the respondents who were not sure if they will use the DCR in the survey 1), or that a significant proportion of PWUD who took part in the survey were in treatment and are currently not actively using drugs from the illicit market (see the 47% of those not willing to use the DCR in the survey 2).
Cleanliness, hygiene, privacy and safety were among the most frequent reasons mentioned by the clients as the most important factors motivating the use of the DCR in the future. Extended opening hours and the availability of the DCR at multiple locations were frequently cited factors that would lead to an increased use of the service by the clients. This is in line with other formative research studies on mobile DCR focusing on designing the programme to serve the needs of the most vulnerable PWIDs with low access to health services and in difficult housing situation [49, 54].
The third interesting finding is the fact that after its launch, the DCR has had to compete with the previously established settings known to be involved in public or semi-public injecting drug use in the area: outdoor brownfield and public toilets in a local supermarket. From the perspective of the user, the van of the mobile unit may offer low level of autonomy and privacy with the close presence of personnel and other clients. Moreover, movement of persons inside of the van causes rocking of the facility, which can be disturbing during the administration of the drug. Also, the opening hours are limited for the DCR to 4 h per day (14.00–18.00) in comparison to those in the supermarket public toilet (07.00–22.00). All in all, awareness about the DCR programme among users and its attractiveness is crucial for the utilisation of the DCR. This was reflected during the implementation of the programme in 2024, when a series of adjustments were implemented.
After the DCR was launched, the start of the programme was quite slow and the number of clients was relatively low, far below the published performance of physical premises-based DCRs with tens or hundreds of clients a day, though capacity and opening hours of DCRs on average are much higher [55]. Also, studies focusing on indicators and predictors of potential DCR use appear to be valid in terms of the predictive value of users' willingness to use DCR in the future – as many as 72% of respondents who expressed an intention to use DCR actually used the service later on [56].
Thus, it's not too surprising that the number of clients and administrations performed in the DCR in Brno has slightly increased over time with growing proportion of opioid administrations and repeated administrations by the same clients, which may be indicative of an increasing interest and acceptance among clients from the problematic area. The gradual improvement is evident especially from the beginning of 2024, when the programme has undergone several changes reflecting the findings of the formative research. Interestingly, gradual and relatively slow uptake is consistent with the beginnings of other similar harm reduction and therapeutic programmes for PWUDs in Brno (such as methadone programmes or outreach programmes targeting the Roma community) and probably reflects the initial mistrust, fear and low adaptability, which is even higher in the Roma community [57]. The development of the performance of the programme shows, that especially in its beginning, it is sensitive to longer interruptions and gaps in provided services.
Feedback from the research led to the adjustments of the programme in 2024 aiming at increasing interest in the DCR programme. Namely, the DCR has extended opening hours from 14.00–16.00 to 14.00–18.00 every working day and has undergone interior refurbishment with an increase in the number of places for drug administration from one client to 2–3 clients at a time. In addition, the acceptable routes of drug administration have diversified (sniffing and oral administration was included). There was also a change in the composition of staff and a more intensive cooperation of the DCR within the outreach programme of Podané ruce was established. Paramedics of the Red Cross, who supervised administrations in 2023, were replaced by social and outreach workers specialised in drug services with first aid training. This has led to a more sensitive and inclusive approach towards clients in general and an improved integration of the DCR service within other harm reduction and counselling services provided on the spot. Last but not least, the feedback from the clients and staff members led to the decision to interrupt the recruitment and the data collection for the originally planned follow-up part of the research project involving the clients of the DCR, which was replaced by the second questionnaire survey. The main rationale for this step was to decrease additional burden and barrier for clients of the DCR and to gather more information about awareness and interest in the use of the DCR among PWUDs in the area in general.
Formative research and practical experience with the DCR implementation also raised a number of questions and provided suggestions regarding the organisation of harm reduction and outreach services in the socially excluded area of Cejl. For example, it has revealed, that there were gaps in the communication with the local Roma community and specifically with Roma PWUDs and the awareness of their situation and needs was low. There were no Romas among professionals of the outreach programme and also no Romas among the trained peers operating in the drug scene of Brno, which was recognised as a need to be addressed in the future. Based on this finding, an immediate action was taken and the DCR team started to communicate and cooperate more with the Roma drop-in centre and methadone programme and organised special opening hours for their clients who identify predominantly with the Roma community.
At the local level, introduction of the first-ever DCR in Czechia was available thanks to the support of the city of Brno and individual municipal districts in Brno. Officials, health-care and social-care authorities as well as law enforcement agencies (the police, the municipal police) have been part of a permanent working group and participated in the DCR formation and implementation. Such support is not commonplace. On the contrary, local authorities and citizens of Czechia had a history of demanding stricter measures against 'problematic persons' and addiction services, as there is a prevalent misconception that they attract people who use drugs [58, 59], which causes addiction services to be stigmatised and pushed out of specific locations [60]. This NIMBY ("not in my backyard") phenomenon is well described also in DCRs elsewhere [61,62,63].
In addition, harm reduction services face administrative and legal barriers in the context of a relatively strict drug prohibition that hinders the emergence and development of services [64], which is also described in the case of DCRs [65, 66]. Also in Czechia, during the almost 30 years of national discussions about this type of programme, the main barriers against DCRs have been too restrictive legislative framework defining drug possession as an offence and a negative attitude of the law-enforcement authorities associating DCRs with drug use promotion. However, the DCR project team in Brno participated in the recent national initiatives on depenalisation and legal regulation in the Czech Drug policy, where the question of decriminalisation of possession of drugs within the context of treatment, harm reduction and supporting services was also raised [64]. Legal analysis was performed on the basis of the existing jurisprudence and interpretation of the legal framework [67, 68] arguing that the possession of one dose of a drug shortly prior to use (which is exactly the usual legal situation in DCR) is equivalent to drug use which is not an offence in Czechia and thus does not constitute grounds for prosecution [69]. Despite the interest from some national authorities in the DCR in Brno shortly after its opening (such as Ministry of Health, Ministry of Interior, National Police Drug Squad), no negative reactions were noted.
The implementation of the research project deviated from its original plan. The planned number of 500 participants of a questionnaire survey prior to the implementation of the DCR could not be reached (n = 131) and thus the subsequent small sample size limited statistical power and some statistical analyses could not be performed (especially the multinomial logistic regression with more covariates which would have been desirable to improve the understanding of the data). Respondents reported that the questionnaire in the first survey was too long and that they did not have enough time and willingness to complete it and no incentives were provided. This changed in the second survey after the launch of the DCR, when the questionnaire was shorter and an incentive was provided (a chocolate bar) – nevertheless, a similarly low sample size was reached (n = 135). Reporting bias is inherent in questionnaire surveys. Some respondents, especially from the Roma community, found some of the questions sensitive, which may have led to refusing to answer some parts of the questionnaire or result in an evasive answer bias. In the quantitative part of the study after the introduction of the DCR, the planned longitudinal study with the follow-up of the clients of DCR was not yet implemented, since the data collection was stopped after recruitment of 9 clients to avoid creating an additional access barrier for the clients. A more comprehensive data collection and analysis of the project outcomes was postponed until the number of clients increase and clients became more engaged and comfortable with the service.
The two cross-sectional surveys should not be seen as longitudinal research on the same cohort of respondents, though some respondents might have participated in both surveys. Therefore, the differences between the two surveys shouldn’t be (with a few exceptions) interpreted as a trend. In the survey 2, for example, there was a significantly lower proportion of persons with risky injecting behaviour, reported overdoses, use of emergency ambulance services, or injecting in a public space. The likely reason for this is the higher proportion of respondents who were recruited from the methadone maintenance programme in the survey 2, i.e. respondents with more stable substance use and more stable life in general. In the same way, the finding that there were more people who use opioids (39.7% versus 27.5%) and also more people from the Roma community (50.7% versus 20.3%) in survey 2 can also be explained, as the clients of methadone programmes in Brno are predominantly of Roma nationality. Also, the higher testing rate or prevalence of HCV in the second study may be attributed to the differences in recruitment and composition of the two samples.
The DCR was launched in a form of a mobile unit in Brno in September 2023. The presented research helped to form its design and services provided. On the other hand, the research design and implementation had to be adjusted based on the development of the local situation and the DCR programme itself. This mutual relationship provided additional opportunities and challenges for the research team as well as for the DRC project team, but substantially facilitated the implementation of the DCR in Brno in its initial phase.
This first-ever DCR in Czechia was introduced without public protests, without conflicts with the law-enforcement authorities and in consent and cooperation with the local administration. It has been shaped, as far as possible, while keeping in mind and respecting the needs of the clients and of the local community. The relationship between clients and the new service has been established and the DCR has been increasingly attracting the most vulnerable PWUDs in Brno. The design of the DCR programme should continually develop and improve in order to increase access and awareness of clients about the service. Further research should focus on the effect of the DCR on the health and social situation of clients and its impact on the local community.
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Authors would like to acknowledge The Office of the Government of the Czech Republic and Gilead Sciences s.r.o. for the support of the implementation of the DCR itself and Gilead Sciences s.r.o. for financial contribution to the publication fee of this article. Authors also thank local authorities (particularly Brno-north district) for their cooperation.
The Western-Eastern European Partnership Initiative on HIV, viral hepatitis and tuberculosis (WEEPI) Foundation (project ID 201) and Cooperatio Programme, the HEAS research area supported the research project. Funding sources had no influence to the design, process and results of the research.
The research protocol was reviewed by the Ethical Board of the National Monitoring Centre for Drugs and Addictions on 21 July 2023. An approval was issued on 27 July 2023 under reference number EKNMS-3/2023.
The authors declare that they have no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Mravčík, V., Janíková, B., Thanki, D. et al. Informed implementation practice – formative research of a mobile drug consumption room in Brno, Czech Republic. Harm Reduct J 22, 106 (2025). https://doi.org/10.1186/s12954-025-01246-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12954-025-01246-4