World Journal of Surgical Oncology volume 23, Article number: 261 (2025) Cite this article
Patient activation, a critical indicator of patients' engagement in their healthcare management and treatment decision-making, has gained increasing attention in surgical settings. This review delves into the current applications, effectiveness evaluations, influencing factors, and intervention strategies of patient activation among surgical patients. It aims to comprehensively analyze its role in enhancing postoperative recovery quality, reducing complications, improving quality of life, and provide theoretical foundations for clinical practice and research.
Surgical interventions represent a critical treatment modality for diverse pathologies, yet their success hinges not only on surgical expertise but also on patients' self-management capabilities [1]. Patient activation—which underscores proactive engagement and participation in healthcare management—has emerged as a pivotal determinant of surgical outcomes. In surgical settings, optimal levels of patient activation correlate with smoother perioperative processes, enhanced postoperative recovery, efficient utilization of healthcare resources, and improved patient satisfaction [2]. Recognizing these multidimensional benefits, this review systematically examines the latest domestic and international advancements in patient activation applications among surgical patients, aiming to provide evidence-based insights for clinical practice and translational research.
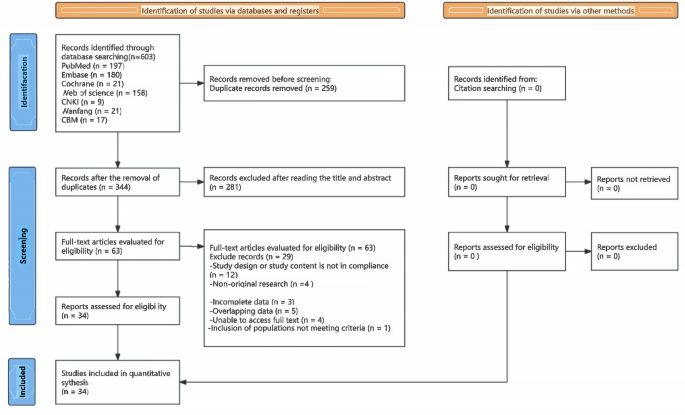
A systematic literature search was conducted across several databases, including PubMed, Cochrane Library, EMBASE, CNKI (China National Knowledge Infrastructure), Medline, Wanfang Data, CBM (China Biology Medicine disc), and Web of Science. The search aimed to identify studies published before May 2025. The following keywords were used: (patient activation[Title/Abstract]) AND (SURGERY) (Fig. 1).
Retrospective Studies: Studies focusing on the assessment of patient activation levels among surgical patients.Interventional Studies: Research that explores interventions aimed at improving patient activation in surgical patients.Clinical Innovations and AI Applications: Studies that investigate cutting-edge measures to enhance patient activation levels and the application of artificial intelligence in this context.
Non-Original Research: Review articles, case reports, editorials, commentaries, and conference abstracts were excluded.Non-Human Studies: Research involving non-human subjects was not considered.Insufficient Statistical Analysis: Studies lacking necessary statistical analysis data were omitted from the review.
This methodology ensures a comprehensive and rigorous approach to identifying relevant studies that contribute to our understanding of patient activation in surgical settings.
In the context of the transition towards a "patient-centered" healthcare model, patient activation is of paramount importance for enhancing the quality of medical services and improving health outcomes. It pertains to patients' proactive engagement and self-initiative in disease management.The Patient Activation Measure (PAM) is a multidimensional assessment tool derived from the disease self-management model,Hibbard's [3] Patient Activation Measure (PAM), grounded in social cognitive theory and self-efficacy theory, categorizes patient activation into four stages. It utilizes a questionnaire to assess patients' cognition, confidence, and capabilities in healthcare management, thereby providing a quantitative tool for clinicians to formulate personalized interventions and for researchers to evaluate patient engagement and the effectiveness of such interventions. The self-management theory emphasizes that patients, as the primary agents in health management, need to possess disease-related knowledge, skills, confidence, and social support to proactively address the physiological, psychological, and social challenges posed by chronic diseases. Patient activation serves as the foundation for self-management, while self-management represents its concrete implementation. These two concepts mutually reinforce each other, jointly contributing to effective patient health management.with three versions: PAM-22 [3], PAM-13 [4], and PAM-10 [5]. Among these, PAM-13 is the most widely utilized in clinical practice and research due to its moderate item length and excellent psychometric properties. The scale employs a five-point Likert scale (ranging from 0—"Not applicable" to 1—"Strongly disagree," etc.). The raw scores are standardized and converted into an index ranging from 0 to 100, with higher scores indicating greater capacity for autonomous health management.
Based on the standardized scores, four activation stages are defined:
Currently, the abbreviated version of PAM has largely replaced the original version, with its culturally adapted translations validated in multiple languages, including German [6], Dutch [7], Italian [8], as well as in Asian countries like Singapore [9] and Korea [10]. In psychometric evaluations across diverse patient populations, such as those undergoing selective lumbar spine surgery [11] and cohorts with multiple sclerosis [12], the Cronbach's alpha values ranged from 0.77 to 0.92, demonstrating the tool's cross-disease validity and measurement stability.
Preoperative application
Preoperative patient activation levels hold significant implications for surgical preparation and postoperative recovery. Numerous studies have demonstrated that enhancing patient activation through education and interventions prior to surgery can foster active patient participation in preoperative preparations, such as smoking cessation, weight reduction, and improvement of nutritional status. This, in turn, reduces surgical risks and enhances the quality of postoperative recovery [13,14,15,16].
An early study involving 65 consecutive patients undergoing lumbar spine surgery categorized patients into low (Stage I, 15 patients), high (Stage IV, 16 patients), and intermediate (Stage II, 12 patients; Stage III, 22 patients) activation groups based on their preoperative activation levels. The findings revealed that participants in Stage IV experienced significantly greater reductions in pain (p = 0.049) and disability (p = 0.035) compared to those in Stage I, along with overall improvements in postoperative health (p < 0.05). However, only the degree of physical health improvement varied according to patients' activation status, with Stage I participants showing less improvement than those in Stage IV (p = 0.044). Physical health improvements exhibited activation-dependent differences, with the low-activation group demonstrating significantly weaker postoperative physical function recovery compared to the high-activation group [17].
Furthermore, a 2023 study following 430 patients undergoing elective spine surgery for one year found that patients with higher preoperative activation levels experienced more significant reductions in postoperative pain and functional recovery [18]. In a 2022 Chinese study [19], 202 patients with lumbar disc herniation completed preoperative paper-based questionnaires, which revealed that the majority of preoperative patients had low activation levels, inadequate self-management abilities, and lacked disease management skills and confidence.
Additionally, a study on preoperative self-preparation among patients with glioma found a significant positive correlation between preoperative self-preparation and eHealth literacy, positive mindset, and positive emotions [20]. Al Ben Ali S et al. [21] also discovered that among 286 patients undergoing colorectal surgery, 74% exhibited high preoperative activation levels. High activation levels were associated with increased adherence to enhanced recovery program interventions, which in turn shortened hospital stays and reduced the risk of complications and readmissions.Concurrent research has also demonstrated the clinical utility of screening preoperative activation levels among patients. A study involving 4,708 adult patients diagnosed with gallbladder disease and undergoing laparoscopic cholecystectomy revealed that screening preoperative activation levels could identify patients unsuitable for early discharge. The findings indicated that patients with low activation levels had a 1.47-fold higher risk of delayed discharge compared to those with high activation levels. Moreover, the risk of postoperative symptom occurrence nearly doubled, and the risk of unplanned utilization of hospital services was 1.85 times higher among low-activation patients. Preoperative screening of patient activation levels can thus assist healthcare providers in formulating personalized intervention plans [22].Another study, which included 125 patients undergoing total joint replacement surgery, showed that higher preoperative patient activation rates were associated with better postoperative pain relief, symptom reduction, improved mental health, and higher satisfaction levels [23]. These findings underscore the significant clinical predictive value of routine preoperative assessment of patient activation levels.The impact of preoperative patient activation rates on surgical and postoperative outcomes is notable. When activation rates are high, patients tend to exhibit better cooperation during surgery, facilitating its smooth execution. Postoperatively, they demonstrate stronger self-management abilities, adhering more closely to medical advice to promote physical recovery, reducing reliance on medical services, and lowering emergency department visits, hospitalization rates, and healthcare costs. Conversely, when activation rates are low, patients may face increased surgical risks due to poor health status and inadequate understanding of the procedure. The risk of postoperative symptoms and complications rises, and self-management deficiencies lead to prolonged hospital stays, increased readmission rates, and greater consumption of medical resources.By quantifying patient self-management efficacy, this assessment effectively identifies high-risk populations with insufficient postoperative rehabilitation potential. The evaluation system focuses on core dimensions such as patient participation in health decision-making, disease management knowledge mastery, and behavioral change confidence, helping medical teams accurately screen vulnerable patient groups who may face complications, delayed recovery, or reduced quality of life due to low activation levels during the preoperative stage. This proactive assessment provides a scientific basis for formulating individualized intervention plans, enabling medical resources to be more targeted toward at-risk populations, thereby optimizing perioperative management strategies and improving overall prognosis quality.
Postoperative application
Postoperative patient activation is equally crucial for preventing complications, promoting wound healing, and accelerating functional recovery. In a study on patient activation after total knee arthroplasty, 241 surgical patients were divided into an intervention group (104 cases) and a control group (137 cases). The results showed that the intervention group experienced less postoperative pain, shorter hospital stays, higher activation rates, greater satisfaction with care, and were more willing to recommend the service [24]. By providing personalized rehabilitation plans and self-management support, patients can better cope with postoperative challenges. In the study by Wennerberg C et al. [25], 170 male patients from 2018–2019 were included. Among the intervention group, 64% (53/83) utilized the ePATH tool. The linear mixed model indicated no significant difference in patient activation between the groups (β = −2.32, P = 0.39; 95% CI: −7.64—3.00). However, baseline patient activation (β = 0.65, P < 0.001; 95% CI: 0.40—0.91) and depression levels (β = −0.86, P = 0.03; 95% CI: −1.64—−0.07) had statistically significant impacts on patient activation scores over the course of one year.Baseline patient activation status and depression scores significantly influenced rehabilitation engagement among the patients. This suggests the importance of prioritizing psychological assessments in the rehabilitation process following prostate cancer surgery. Skolasky RL et al. [26] found that, although differences between groups among spinal surgery patients were similar at the 3-month postoperative mark, the most significant differences in mental health were observed in the low-activation group at the 12-month postoperative stage. This indicates that patient activation plays a crucial guiding role in long-term rehabilitation. Focusing on and enhancing patient activation can provide direction for long-term rehabilitation and assist in formulating targeted strategies. In a 2024 study on hip fracture patients [27], assessments of patients' mobility, function, and daily activities at discharge, 12 weeks, and 24 weeks confirmed that patient activation levels were correlated with hip fracture rehabilitation outcomes, with higher activation levels leading to better functional recovery and mobility. Additionally, e-health supports such as smartphone apps and online platforms provide convenient rehabilitation pathways for patients, enhancing their activation levels.This underscores the need for hospital staff to strengthen postoperative education for patients. Specifically, they should provide detailed rehabilitation knowledge and conduct training courses to equip patients with the necessary information. Additionally, psychological support should be offered, including assessing and intervening in negative emotions, sharing success stories to encourage a positive mindset.Optimizing doctor-patient communication is also crucial. Building a good rapport with patients and regularly providing feedback on their rehabilitation progress can enhance trust and engagement. Leveraging technological tools, such as recommending mobile health applications and telemedicine platforms, can facilitate continuous care and support beyond the hospital setting.Moreover, creating a supportive environment is essential. Encouraging family involvement in the patient's rehabilitation, organizing patient exchange activities, and garnering social support can foster a sense of community and motivation, ultimately contributing to a smoother and more successful postoperative recovery.
Healthcare resource utilization
Patient activation levels significantly influence the efficiency of healthcare resource utilization. Research shows [22] that compared to highly activated patients, low-activation patients face a 47% increased risk of delayed discharge, a doubled risk of postoperative symptom occurrence, and an 85% higher risk of unplanned medical visits. Patients in the high-activation group have shorter hospital stays and can utilize rehabilitation resources more effectively, while low-activation patients may experience prolonged hospitalizations, frequent follow-ups, and excessive reliance on medical interventions due to insufficient self-management efficacy, thereby increasing healthcare resource consumption. A study on thoracoabdominal surgery patients also revealed [28] that low patient activation levels were significantly associated with higher rates of unplanned medical utilization, emergency department visits, complications, and prolonged hospital stays compared to high-activation patients. Many sickle cell disease (SCD) patients have low activation levels and self-efficacy, and improving these factors can help reduce pain-related medical needs [29]. Among total laryngectomy (TL) cancer patients, increased patient activation may be linked to reduced overall treatment costs, a trend with positive implications from both healthcare system and socioeconomic perspectives [30]. Enhancing patient activation levels can optimize resource allocation and improve the cost-effectiveness of medical services [31]. Identifying such patients facilitates targeted interventions, enhances health literacy, and optimizes post-discharge self-management.
Telemedicine and ehealth support
Advances in telemedicine and eHealth technologies have further expanded the application of patient activation among surgical patients. In an early study on surgery for degenerative lumbar spinal stenosis [32], the authors evaluated patient activation before and after health behavior change counseling, confirming its impact on rehabilitation engagement, although one-third of the patients still exhibited low participation levels.In the study by Melissant HC et al. [33], a web-based self-management application called Oncokompas was used to assess differences in patient activation and doctor-patient interactions. After using Oncokompas, breast cancer survivors showed a significant improvement in patient activation scores (p = 0.007), though no significant change was observed in doctor-patient interaction scores (p = 0.75).In 2019, Ekstedt M et al. [34] developed an eHealth intervention tool, the electronic Patient Home Therapy Activation System (ePATH), based on motivational behavioral theory and specifically designed for prostate cancer patients. A randomized controlled trial involving patients after radical prostatectomy found that eHealth support significantly enhanced patient activation levels [25], indicating high clinical applicability and effectiveness of the system.Meanwhile, research has also shown [35] that tele-rehabilitation is comparable to hospital-based cardiac rehabilitation in terms of improving patient engagement and health knowledge. Another study adopted an evidence-based web-based self-management program (SMP) combined with motivational interviewing, evaluating participants using patient activation measures at baseline, 12 weeks, and 26 weeks. The results indicated that the intervention significantly improved health outcomes at 26 weeks [36].These findings reveal the intertwined impact of digital technologies and patients' own states in postoperative rehabilitation. On one hand, digital tools such as smartphone applications and online platforms demonstrate significant potential. With their convenience and comprehensiveness, they transcend temporal and spatial limitations, enabling patients to access professional and rich health information anytime, anywhere. This information covers various aspects of postoperative rehabilitation, including diet, exercise, and medication during different stages. Additionally, these tools assist patients in real-time monitoring of their physical indicators, such as body temperature and wound recovery, and facilitate efficient communication with healthcare providers. Patients can promptly report issues encountered during rehabilitation, and doctors can provide precise guidance accordingly, thereby effectively enhancing patient activation and improving their self-management awareness and capabilities.On the other hand, recent studies have sounded the alarm. Regardless of whether digital health applications are used for remote follow-up, low patient activation levels remain a key predictor of postoperative outcomes after elective colorectal surgery. These patients often lack the initiative to actively participate in rehabilitation and struggle to fully utilize advanced tools, leading to slow postoperative recovery and an increased risk of complications [37]. This underscores the importance of enhancing patient activation levels for improving postoperative recovery outcomes. Only by fundamentally stimulating patients' intrinsic motivation can digital tools truly exert their effects and assist patients in achieving better rehabilitation.Meanwhile, we also acknowledge the limitations of e-health technologies, such as the weak digital skills among the elderly and the digital divide in rural areas. To address these issues for these specific groups, we can tailor digital skills training courses for them, employing intuitive teaching methods. In rural regions, we should strengthen network infrastructure development by collaborating with enterprises to expand network coverage. Additionally, we can promote digital literacy through widespread campaigns, dispatch volunteers to provide guidance, and distribute user manuals to facilitate the adoption and effective use of e-health technologies.
Demographic characteristics
Patient characteristics such as age, gender, education level, and income level can all influence patient activation levels. Studies have shown that patients with higher incomes and education levels tend to have higher patient activation levels [7], while older patients and those with lower education levels often have lower patient activation levels [27]. In a 2021 study of 1018 patients undergoing spinal surgery [38], the average patient activation score was 70 ± 17 points, with female and higher-income patients having higher activation levels. Patient proactivity is significantly influenced by gender and economic factors. Female patients generally exhibit stronger psychological resilience or adaptability when facing illness, have a stronger desire for rehabilitation, and often pay more attention to health management and preventive care. On the other hand, low-income patients have lower treatment adherence and health management enthusiasm due to economic pressures and psychological burdens. Research has shown that Latino American patients have lower activation levels than non-Latino and African American groups, while Hispanic and Black patients are weaker than White groups in terms of self-control ability and activation levels [39, 40].
Psychological factors
The psychological state of patients, such as depression and anxiety, can also affect their activation levels. Psychological distress significantly exacerbates patient pain and impairs quality of life (HRQoL), while higher patient activation levels help alleviate physical functional decline. Clinical practice should prioritize screening for psychological distress and patient activation, and strengthen support measures to improve pain management and maintain quality of life in high-risk patients [41]. In patients undergoing spinal surgery, low activation scores are significantly associated with depression, fatigue, increased pain, and decreased social satisfaction [38]. The Patient Activation Measure (PAM) is an important tool for assessing the degree of patient engagement in healthcare, not only related to improved prognosis after spinal surgery but also widely applicable in various healthcare scenarios, and associated with better outcomes [42]. Negative emotions such as depression can weaken patients' confidence in treatment, trigger passive coping behaviors, and thereby reduce their rehabilitation motivation [43].In a study conducted in 2023 involving 618 thyroid cancer patients from two hospitals in Hunan Province, China, it was demonstrated that intervention strategies could be formulated targeting the avenues for health-promoting behaviors among thyroid cancer patients. These strategies aim to enhance social support and patient activation, thereby promoting healthier behaviors and ultimately alleviating the burden on medical and nursing care [44].Therefore, in clinical practice, personalized intervention measures should be developed based on patients' individual characteristics, comprehensively assessing their individual characteristics and needs, and forming a multidisciplinary team including doctors, nurses, psychologists, and social workers to develop personalized intervention plans.
Disease-related factors
Different diseases and types of surgery impose varying activation demands on patients. For instance, complex surgeries like spinal operations and joint replacements often necessitate higher activation levels from patients to manage postoperative challenges [23, 38]. Concurrently, the severity of the disease and the presence of complications also impact the patient's activation level [45, 46]. Consequently, a thorough preoperative evaluation of the patient's disease status and surgical risks is essential to devise targeted intervention strategies.
Despite demonstrating some effectiveness, patient activation intervention strategies still face several limitations. Educational interventions, while enhancing patients' understanding of their condition and treatment, struggle to address psychosocial barriers to activation. Mobile applications and telemedicine platforms, although providing convenient educational support tools, face varying levels of user acceptance and engagement, particularly among the elderly and technologically disadvantaged groups. Furthermore, most interventions focus solely on knowledge acquisition, overlooking the multidimensional nature of activation, which encompasses integrated improvements in behavior, emotion, and cognition. To overcome these limitations, this study proposes the following intervention strategies to comprehensively optimize surgical patients' activation levels, thereby improving postoperative outcomes and enhancing healthcare system efficiency.
Preoperative education program
Structured preoperative education represents a systematic intervention model that integrates multidisciplinary knowledge to provide patients with personalized preoperative preparation. This educational model comprises three main pillars: health education, nutritional intervention, and exercise training. Health education aims to build a cognitive framework for patients by accurately conveying surgery-related information. Nutritional intervention involves developing individualized dietary plans to optimize preoperative metabolic status. Exercise training enhances surgical tolerance through physical conditioning. As a technology-enabled approach, video-assisted education offers significant advantages over traditional paper-based materials, as its multidimensional information presentation can enhance patients' depth of understanding and retention of memory. By integrating multidisciplinary approaches with technology empowerment, this model effectively improves patient activation levels, and its scientific mechanisms provide a theoretical framework for subsequent research. In the future, further exploration can be conducted on the adaptability and mechanisms of action of this model in different surgical scenarios, providing evidence-based support for optimizing perioperative management.
Digital health interventions
Mobile health applications and remote monitoring have significantly enhanced patient activation levels through innovative interaction models. An APP-based management platform integrates personalized health plans and real-time doctor-patient communication functions, combined with dynamic physiological parameter monitoring via wearable devices, to establish a closed-loop management system driven by "data-behavior feedback." The specific scientific mechanisms are as follows: (1) information accessibility that transcends spatiotemporal limitations strengthens patients' self-management capabilities; (2) personalized decision support systems improve self-efficacy; and (3) immediate doctor-patient interaction enhances treatment adherence.In the latest study focusing on breast cancer patients [47], an Artificial Intelligence (AI)-based Survivorship Care Plan (SCP) service significantly improved patient activation among post-treatment breast cancer survivors (p = 0.051, effect size = 0.29). The utilization of EHealth solutions has been shown to enhance patients' activation capabilities [48]. Digital solutions can streamline the collection and management of health-related needs during surgical procedures, addressing unmet needs and increasing patient activation rates. This is crucial for ensuring positive health outcomes, particularly for patients undergoing complex surgeries [49].Future research can further explore the application effects of this technology in different surgical types and patient populations, as well as its correlation mechanism with long-term rehabilitation outcomes, thereby providing a scientific basis for promoting the application of digital healthcare in perioperative management.
Shared Decision Making (SDM) model
Integrating the concept of patient activation into the shared decision-making process and optimizing the quality of medical decisions through dual interventions of decision support tools and doctor-patient communication training. The decision support tools, centered on structured information presentation and visual risk communication, enhance the surgical knowledge mastery of low-activation patients. The activation-oriented doctor-patient communication training strengthens doctors' patient-centered communication skills, reducing the incidence of decision-making conflicts. The innovation of this mechanism lies in: (1) cognitive empowerment—decision tools compensate for information processing deficits in low-activation patients; (2) behavioral guidance—communication training optimizes doctor-patient interaction patterns. The synergistic effect of the two not only improves decision rationality but also enhances decision acceptance. This provides technical pathway support for a patient-centered decision-making system.
Based on the above research, preliminary results have been achieved in the study of patient activation among surgical patients, but there are significant limitations. Most research focuses on short-term postoperative outcomes (such as length of hospital stay and complication rates), while exploration of its long-term rehabilitation effectiveness (encompassing quality of life, psychological resilience, and functional recovery) is still insufficient. At the methodological level, existing studies are mostly single-center, small-sample observational designs, lacking strong evidence support from multi-center randomized controlled trials (RCTs), and the generalizability and robustness of the conclusions need to be verified. In terms of intervention strategies, despite proposing various activation enhancement programs, there is a lack of head-to-head comparative studies, and the optimal intervention model has not yet been identified. Future research needs to deepen and expand from three dimensions: first, expand research horizons to long-term postoperative prognosis, focusing on core indicators such as quality of life, psychological adaptation, and social function reconstruction, and build a multidimensional evaluation system; second, promote multi-center large-sample RCTs to strengthen the external validity and reliability of research conclusions; third, carry out comparative studies on the effectiveness of interventions to clarify the advantageous scenarios and optimal combinations of different strategies. In addition, the innovative application of digital health technologies (such as AI-driven personalized management apps) in enhancing patient activation should be explored, reshaping patient self-management paradigms through real-time interaction, intelligent feedback, and behavioral interventions. In summary, research on patient activation in the field of surgery is currently in a critical transition period, requiring the integration of evidence-based medicine and digital technology innovation to promote the transformation of research paradigms from short-term outcome observation to life-cycle management, providing higher-quality evidence support for clinical decision-making.
Meanwhile, we recognize that due to differences in health system structures (e.g., the decentralized private healthcare system in Western countries versus the centralized public healthcare system in China), cultural roles (e.g., the emphasis on individual decision-making in the West versus the importance of family involvement in China), and health literacy levels (higher overall in the West but with disparities in China), there exist variations in approaches to patient activation between China and Western countries. Subsequent research will delve into the implications of these differences, exploring commonalities and specificities through cross-cultural comparative analysis to enhance the international relevance of the study and provide references for medical practices across different cultures.
No datasets were generated or analysed during the current study.
We greatly appreciate the assistance of the staff of the Department of Thoracic Surgery, West-China Hospital, Sichuan University, and thank them for their efforts.
This paper was supported by the Natural Science Foundation of Sichuan Province (No.2024NSFSC1924) (to Cheng SHEN).
Approval of the research protocol by an Institutional Reviewer Board: N/A.
- Informed Consent: N/A.
- Registry and the Registration No. of the study/trial: N/A.
- Animal Studies: N/A.
Not applicable.
The authors declare no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Yin, Y., Zhang, J., Long, X. et al. Application and advances of patient activation in surgical patients. World J Surg Onc 23, 261 (2025). https://doi.org/10.1186/s12957-025-03911-1