BMC Complementary Medicine and Therapies volume 25, Article number: 242 (2025) Cite this article
Pranayama breathing exercises may help reduce the burden of chemotherapy-induced symptoms in women with breast cancer. The aim of this study was to determine the effect of pranayama breathing exercise on symptom burden in women with breast cancer undergoing chemotherapy.
In this clinical trial, 76 participants were randomly assigned to two groups: pranayama breathing exercise plus routine care (intervention group) (n = 38) or routine care (control group) (n = 38). Patients were asked to perform pranayama breathing twice a day for 10 min for 21 days (one week before chemotherapy to 14 days after the start of chemotherapy). Symptom burden was measured through the MD Anderson Symptom Inventory (MDASI) before the intervention, on the first day of chemotherapy, on day 7 and on day 14 after chemotherapy.
A significant decrease in the total score of symptom burden and subscales of symptom severity and symptom interference with daily activities was shown in the intervention group compared with the control group at all three measurement points (η2 = 0.431, η2 = 0.311, η2 = 0.489, P < 0.001, respectively). Among the symptoms, there was no significant difference in the mean score of dry mouth (P < 0.744, η2 = 0.002) and numbness and tingling (P < 0.302, η2 = 0.02) between the intervention and control groups.
Pranayama breathing exercise was effective in reducing the symptom burden in women with breast cancer undergoing chemotherapy. It is recommended that the pranayama breathing be considered as a component of comprehensive cancer care. Nurses should teach patients pranayama breathing as an independent nursing intervention to reduce the burden of chemotherapy-induced symptoms.
This trial has been registered on the Iranian Registry of Clinical Trials (http://www.irct.ir) with the identifier (IRCT20231212060343N1). Registered date: 23/01/2023.
Breast cancer is the most common cancer in women and the second leading cause of cancer-related death worldwide [1]. Chemotherapy is one of the most common treatments for breast cancer and causes side effects such as nausea, vomiting, diarrhea, fatigue, and pain [2]. Women with breast cancer who are undergoing chemotherapy often experience multiple symptoms. These symptoms may occur simultaneously and throughout the course of chemotherapy [3, 4] and have negative effects on the quality of life and functional status of patients [5].
Most studies have examined the side effects of chemotherapy individually, while cancer patients often experience multiple symptoms at the same time, which is defined as “symptom burden” [2]. Symptom burden refers to all the symptoms at a certain time and has a negative effect on the performance and mental state of patients [6]. The severity of symptom burden can lead to delay or discontinuation of treatment and complicate recovery. Additionally, increased symptom burden is related to decreased survival of cancer patients and poor quality of life [6, 7].
The use of complementary and alternative medicine (CAM) in breast cancer patients, especially for symptom management, is more common than in other cancers [8]. The main goal of CAM is to relieve symptoms and restore physical balance. It is also used as an alternative to prevent the side effects of chemotherapy [9]. Unlike medical treatments such as chemotherapy, which may be expensive and have many side effects, behavioral interventions such as breathing exercises are inexpensive and mostly do not have side effects [10].
Yoga is one of the most common methods of the Indian complementary therapy and alternative medicine that has been used for 3000 years [11]. It includes yoga postures, breathing and meditation and helps to improve physical and mental health [12,13,14]. Yoga has a potential therapeutic role in symptomatic management of breast cancer patients, enhancing quality of life during treatment, as well as improving adherence to treatment[15]. Pranayama is one of the important parts of yoga, which, by focusing on breathing control, helps to regulate the life force (prana) and improve the connection between emotions, cognition and behavior [16, 17]. Pranayama helps to improve the oxygen supply, increase mental concentration and prevent diseases [18]. Two common types of breathing in yoga are Kapalabhati breathing (rapid abdominal breathing), which increases lung capacity and reduces negative emotions, and Nadi Shodhana breathing (alternating nostril breathing), which helps balance the nervous system and reduce stress [17, 19].
Studies on the effect of breathing exercises on the symptom burden of cancer patients undergoing chemotherapy are limited. Most studies have investigated the effect of pranayama breathing exercises on individual symptoms [10, 20,21,22]. To our knowledge, no study has investigated the effects of pranayama breathing exercise on symptom burden among women with breast cancer undergoing chemotherapy. Therefore, this study was designed based on the hypothesis that the pranayama breathing exercise can be effective for reducing symptom burden in women with breast cancer undergoing chemotherapy.
The present study was a randomized controlled trial with a pretest–posttest. The study environment was Velayat Teaching Hospital in Qazvin city. Velayat Hospital is the main specialized oncology center in Qazvin Province and is located in Qazvin city. This study adhered to the Consolidated Standards of Reporting Trials (CONSORT) guidelines for reporting.
The participants were 76 women with breast cancer, including 38 in the intervention group and 38 in the control group, who were treated in the outpatient chemotherapy unit between January and May 2024. The eligibility criteria included (i) definite diagnosis of breast cancer, (ii) age 18 years and older, (iii) receiving at least one cycle of chemotherapy after surgery, (iv) cancer stage two or three, (v) Eastern Cooperative Oncology Group (ECOG) score < 2, and (vi) willingness to participate in the study. The exclusion criteria included (i) suffering from other serious diseases at the same time (heart diseases, respiratory diseases, liver diseases, etc.), (ii) having brain or liver metastases, (iii) receiving radiotherapy at the same time, (iv) being pregnant or breastfeeding, and (v) having communication and psychological problems. The attrition criteria were as follows: unwillingness to continue participating in the study, death or change in the patient's treatment plan, and receiving a new treatment procedure during the study.
The participants were selected for convenience among women with breast cancer who were receiving chemotherapy and referred to specialized oncology clinics at Velayat Hospital. Eligible people were randomly assigned to either the intervention group with the pranayama breathing technique or the control group.
The participants were divided into two intervention and control groups via the random block allocation method. Block random allocation was performed via software (Random Allocation Software, Version 1.0.0.) in blocks of 4 and 6.
To conceal the blocked randomization process, the names of the groups were placed in envelopes, and these envelopes were numbered from 1 to 76 in the sequence provided by the software and arranged in a box. The researcher who performed the randomization was not aware of the contents of the envelopes. After ensuring the participant's recruitment for the research and obtaining written informed consent, the first envelope was taken by the researcher, and the participant was allocated to one of the study groups according to the contents of the envelope.
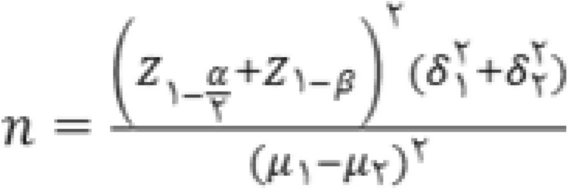
The sample size is based on a previous study [10], taking into account the mean (SD) of sleep disorders after the intervention of pranayama breathing exercise in the two intervention and control groups of 60 (SD = 21.4) and 43.5 (SD = 16.8), respectively, was estimated. Therefore, considering (95% confidence) and β = 0.1 (90% power) α = 0.05 and taking into account 20% attrition, 38 people were estimated to be needed for each group.
After official permission was obtained, one of the researchers referred to the oncology outpatient clinic. After accessing the list of patients and their phone numbers, the researcher called the patients. During the phone call, patients were given explanations about the purpose and necessity of the study. The researcher asked the eligible women to participate in the study to refer them to the outpatient oncology clinic one week before chemotherapy (baseline point) to complete the questionnaires. In addition, at baseline, the intervention group was educated on how to perform pranayama exercises. Additionally, to appreciate the patients for participating in the study, the health status of the patients was evaluated, for example, by measuring blood pressure and blood sugar. Patients were guided to a suitable and quiet room located in the oncology clinic. Written and verbal informed consent was obtained by the researcher after providing sufficient information about the purpose and benefits of the study to the patients and their caregivers (if they had a caregiver) and before randomization. The researcher reviewed the patients'medical records to confirm their eligibility. The baseline questionnaire was subsequently completed. Finally, the researcher assigned the patients to one of two intervention or control groups via sealed envelopes.
Before starting the study, the researcher referred to a specialized yoga center and was trained to perform pranayama breathing exercises by a yoga instructor and obtain a valid certificate. In the intervention group, the researcher trained pranayama breathing exercise as supplement standard care step by step during the first meeting with the patient in the oncology clinic, which was a week before the start of chemotherapy. The training was performed individually and face-to-face for 15–20 min in a quiet room to the patient and, if the caregiver was present, to her caregiver. A Pranayama breathing exercise video was played to the patients. The video was then sent to the patient's smartphone or delivered to the patient via DVD. To ensure the patient's learning, she was asked to perform the breathing exercise step by step in the presence of the researcher. Breathing exercises were performed by patients at home for 10 min twice a day for 21 days (one week before the start of chemotherapy until day 14 after the start of chemotherapy) [10, 16]. The researcher called the patients daily to ensure that they performed breathing exercises at home and followed up on their health status. In addition, the researcher recorded breathing exercises in a diary during daily phone calls with patients for 21 days.
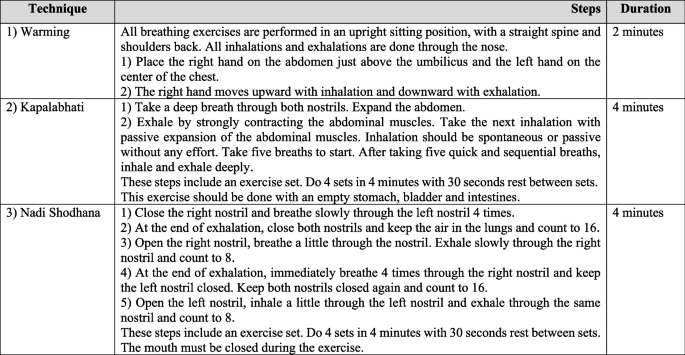
According to the literature review [10, 20, 23] and after consulting oncologists and yoga instructors, three breathing techniques of pranayama were applied: (i) warming up (2 min), (ii) Kapalabhati breathing (4 sets in 4 min), and (iii) Alternate Nostril Breathing (Nadi Shodhana) breathing (4 min). The reasons for choosing these techniques are that they are easy for the patient and that the rhythm and speed of breathing are changed simply by the patient [24]. Pranayama breathing exercise was performed for 10 min, two times within 24 h. The stages of pranayama breathing are described in detail, and the duration of each stage is shown in Fig. 1.
The present study was double-blinded. The outcome assessor and data analyst were blinded to the study groups. However, due to the nature of the intervention, the participants were not blinded to the breathing exercise.
During the study period, the control group received only routine care. At the end of the study, pranayama breathing exercise was provided to volunteer patients in the control group, and an educational video was provided to them.
Demographic and clinical information
This form included two parts of demographic information (age, education, marriage, employment status, and economic status) and clinical characteristics (duration of disease diagnosis, cancer stage, family history of breast cancer, type of breast surgery, and functional status score based on the Eastern Cooperative Oncology Group (ECOG) scale).
Eastern Cooperative Oncology Group (ECOG)
The ECOG functional status scale was used to determine the functional status of patients. This scale is composed of one item that is scored on a 5-point scale from 0 (fully active) to 4 (fully dependent on others for self-care). A higher score (≥ 2) indicates a weaker performance status. The validity of the scale is demonstrated by its strong correlation with the Karnofsky performance status scale. Because the ECOG scale is a single item, internal consistency reliability cannot be measured [24].
M. D. Anderson Symptom Inventory (MDASI)
The MD Anderson Symptom Inventory is a relatively short instrument designed by Cleeland et al. (2000) to measure symptom severity and symptom interference with functioning in cancer patients. This questionnaire includes 19 symptoms and has two subscales: symptom severity (13 items) and symptom interference with daily life activities (6 items). The MDASI assesses symptom severity in the past 24 h on a scale ranging from 0–10, where 0 represents “no symptoms or interference” and 10 represents “the greatest severity of symptoms or interference”. The score of each subscale is calculated with the total scores of its items. The total symptom burden score is obtained from the sum of the mean scores of the two subscales of symptom severity and symptom interference in daily activities. A higher score indicates a greater symptom burden [25]. The psychometric properties of the questionnaire have been confirmed in Iran among breast cancer patients, with a Cronbach's alpha of 0.9 [26].
Data collection was performed at four time points (one week before chemotherapy, the first day of chemotherapy, the first week after chemotherapy and the second week after chemotherapy). At baseline (one week before chemotherapy), questionnaires were completed via a face‒to‒face interview by the researcher. The questionnaires were completed three times (the first day of chemotherapy, the first week after chemotherapy and the second week after chemotherapy) through a phone call by a research assistant who was not aware of the allocation of patients to groups. The research assistant was a nursing master's student who was trained by the main researcher about the objectives of the study, the necessity of the study, and how to complete the questionnaires before starting the study.
Data analysis was performed via statistical software version 4.1.1. The normal distribution of variables was confirmed via the Shapiro‒Wilk test. Between-group comparisons of demographic and clinical characteristics, in addition to the chi-square test and independent t test, were performed with the method suggested by Imbens and Rubin, considering the criterion of a standardized mean difference < 0.25 for continuous quantitative variables and a < 10% risk difference index for categorical variables [27]. Intergroup comparisons of changes in the mean scores of the MDASI and its subscales (symptom severity and interference of symptoms with daily activities) as well as comparisons of changes in the mean scores of individual symptoms at the measurement time points were performed, and repeated measures analysis of variance statistics was performed. All analyses, including functional status, education, employment, economic status, cancer stage, and chemotherapy cycle, were performed while controlling for the effects of potential covariates according to the Imbens and Rubin criteria. If the default of sphericity was not confirmed, the findings were reported with Greenhouse–Geisser correction. A significance level of 0.05 was used for all analyses.
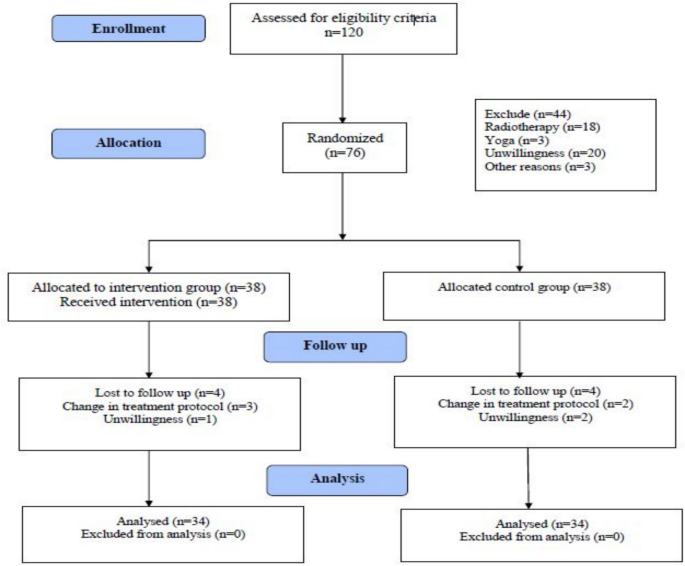
In the present study, 76 people were randomly assigned to the intervention group (pranayama breathing technique) or the control group (38 people in each group). During the sampling period, 4 people from the intervention group and 4 people from the control group withdrew from the study because of changes in the treatment protocol and an unwillingness to continue participating. Figure 2 shows the CONSORT diagram for the study process.
The mean age of the participants in the intervention group was 51.11 years (SD = 10.21), and that of those in the control group was 49.32 years (SD = 12.15). A comparison of the demographic and clinical characteristics of the participants between the intervention and control groups revealed no significant differences (Table 1).
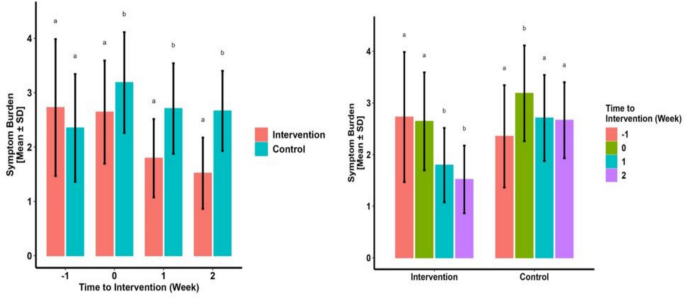
Table 2 and Fig. 3 show a significant decrease in the mean MDASI total score on days 1, 7 and 14 after chemotherapy in the intervention group compared with the control group. Additionally, the total score of symptom burden in the intervention group decreased during the measurement time points, which was significant on the 7th and 14th days compared with the baseline. In the control group, the symptom burden increased significantly on day 1 after chemotherapy compared with that at baseline and then decreased on days 7 and 14, which was not statistically significant compared with that at baseline (Table 2).
Comparison of the changes in the mean scores of symptom load between and within the study groups during measurement time points
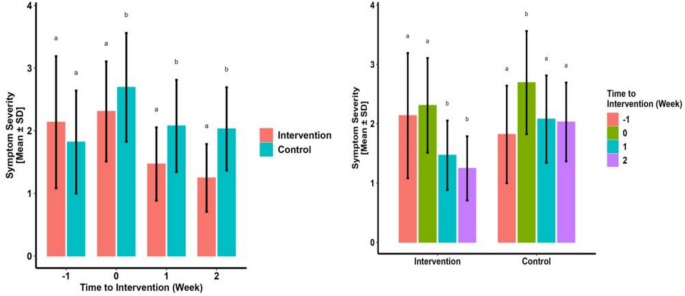
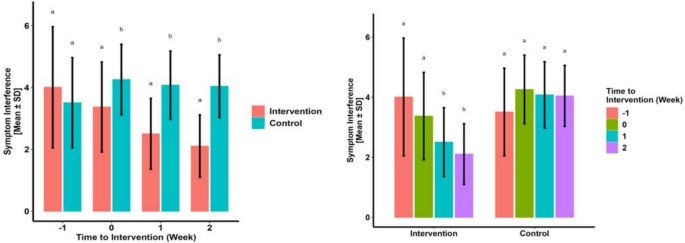
The mean symptom severity score on days 1, 7 and 14 after chemotherapy in the intervention group was significantly lower than that in the control group. Additionally, the mean score of symptom interference on days 1, 7 and 14 after chemotherapy in the intervention group was significantly lower than that in the control group. Additionally, there was a decrease in the mean score of the symptom severity subscale and the symptom interference subscale during the measurement time points in the intervention group, which was significant on the 7th and 14th days compared with the baseline. In the control group, the symptom interference scores increased significantly on day 1 after chemotherapy compared with those at baseline, and then decreased significantly on days 7 and 14 (Table 2, Figs. 4, and 5).
Comparison of changes in mean scores of symptom severity subscale between and within study groups during measurement time points
Comparison of changes in the mean scores of the subscale of interference of symptoms with daily activities between and within the study groups during measurement time points
Compared with those in the control group, the mean scores of pain, distress (upset), lack of appetite, drowsiness, sadness, general activity, mood, work, relationship with others, walking, and enjoyment of life at all measurement times were significantly lower in the intervention group. However, there was a significant decrease in the mean score of fatigue and disturbed sleep on the 7th and 14th days after chemotherapy, nausea and vomiting only on the first day of chemotherapy and problems in remembering only on the 7th day after chemotherapy in the intervention group compared with those in the control group. There was no significant difference in the mean score of dry mouth and numbness and tingling on days 1, 7 and 14 after chemotherapy between the two groups (Table 3).
During the intervention and follow-up, no side effects related to the pranayama breathing technique were reported by the participants.
The present study is the first to investigate the effects of pranayama breathing as supplement standard care on the symptom burden in women with breast cancer undergoing chemotherapy. Therefore, the findings of this study can help complete the existing body of knowledge about the use of complementary and alternative medicine methods in relieving the chemotherapy-induced symptom burden.
The findings of the present study revealed a significant difference in the mean score of symptom burden and its subscales (symptom severity and symptom interference with life activities) one week before chemotherapy, on the first day and at the end of the first and second weeks of chemotherapy between the intervention and control groups at all measurement time points. Hence, in our study, the effectiveness of pranayama breathing exercise intervention in reducing the symptom burden in women with breast cancer undergoing chemotherapy was confirmed. In line with the present study, Dhruva et al. [10] reported that increasing the frequency and duration of breathing pranayama exercise during two consecutive cycles of chemotherapy leads to improvements in symptoms and quality of life in cancer patients. However, they evaluated the effect of pranayama breathing on chemotherapy-induced side-effects such as fatigue, sleep disturbance, anxiety, depression, and stress individually and did not consider symptom burden. Moreover, their study had limitations such as small sample size and lack of blinding, which recommended confirming the efficacy of the results in a larger future study.
Additionally, a previous study provided evidence of a rapid and significant reduction in symptom burden in the intervention group compared with the control group by performing a 20-min session of mindfulness breathing [28]. Previous studies [20, 21] have shown that deep breathing exercises can lead to improved functional status (a person's ability to perform activities of daily living, self-care, and daily roles and maintain health and well-being) in breast cancer patients undergoing chemotherapy.
The findings of the present study indicated a significant decrease in the mean score of pain, distress (upset), lack of appetite, drowsiness, sadness, general activity, mood, work, relationship with others, walking, and enjoyment of life at all measurement time points in the intervention group compared with those in the control group. Previous studies [13, 29,30,31] have shown that yoga interventions, especially deep breathing exercises, are effective in reducing tension, anxiety, negative emotions, and frustration in women with cancer undergoing chemotherapy. During pranayama breathing exercise, the focus will be only on breathing, so one's thoughts will be controlled. Performing these breathing exercises repeatedly can help calm the mind [32]. Moreover, deep breathing can reduce cortisol levels and improve attention and mood [23].
Consistent with previous studies [33,34,35], the effectiveness of pranayama breathing exercise on pain intensity was confirmed in the present study. According to the fight-flight theory, uncontrolled pain can activate the sympathetic nervous system, which can cause more pain. However, breathing exercise can activate the parasympathetic nervous system, which can lead to pain relief [35]. On the other hand, on the basis of baroreflex theory, respiratory manipulation can activate the baroreflex, which leads to a decrease in pain sensitivity [36].
Another finding of the current study was the positive effect of pranayama breathing exercise on reducing fatigue and disturbed sleep in women with breast cancer undergoing chemotherapy, which was consistent with the findings of previous studies [22, 32, 37, 38]. Deep breathing techniques activate the parasympathetic nervous system by increasing the oxygen level in the lungs and help maintain relaxation. Therefore, it will reduce psychological pressure and improve sleep [39, 40]. Unlike the present study, Dhruva et al. [10] did not report positive effects of pranayama on fatigue and depression. The authors explained this finding with the small sample size and not the high level of depression in the participants.
In the present study, pranayama breathing exercise significantly reduced the severity of nausea and vomiting in the intervention group compared with the control group, which was consistent with previous studies [20, 21]. Previous studies have shown that chemotherapy-induced nausea and vomiting are associated with anxiety, depression, fatigue and sleep disorders in cancer patients [41, 42]; therefore, Pranayama breathing exercise can help reduce the severity of nausea and vomiting by relieving the risk factors mentioned. In contrast, another study [23] showed that participating in an 8-week yoga program was not effective in reducing chemotherapy-induced nausea and vomiting in women with breast cancer. This finding was justified by the mild or moderate severity of nausea and vomiting of the patients, as well as the low adherence to the yoga program in the sessions held at home.
In the present study, a significant difference in the mean score of problems with remembering was found only at the second follow-up (day 7 after chemotherapy) between the intervention and control groups. In support of our findings, a previous study revealed increased difficulties in concentrating and remembering in the fourth to eighth cycles of chemotherapy [43]. Therefore, in our work, the lack of a significant difference between the two groups in terms of problems in remembering on the first day of chemotherapy was not unexpected. Evidence from another study revealed the effectiveness of yoga programs on various aspects of cognitive function in women with breast cancer undergoing chemotherapy. Yoga affects cognitive function by reducing stress and improving mood. Furthermore, yoga programs help improve attention span and the ability to change attention and improve memory [44].
In the present study, in the comparison between groups, no significant difference was found in the mean score of dry mouth and numbness and tingling at any of the measurement times. This finding can be explained by the low severity of these side effects in our participants, who were treated with doxorubicin and cyclophosphamide regimens. Doxorubicin and cyclophosphamide regimens are significantly associated with late onset (10 days after chemotherapy) and low severity of dry mouth and mucositis [45]. Taxanes, Platinum compounds, and Vinca alkaloids often cause chemotherapy-induced peripheral neuropathy [46]. The participants in our study were treated with cyclophosphamide and doxorubicin in the first 4 cycles, which are not drug categories that cause peripheral neuropathy. In addition, the severity of numbness and tingling in our participants was low at all measurement time points, which is in line with the findings of another study [43] that showed an increase in neurological symptom scores concurrently with the progression of chemotherapy among women with breast cancer; thus, the increase in the score of the neurological symptom cluster in the fourth cycle was significant compared with that in the second and third cycles.
The strength and novelty of the present study was that it was the first to evaluate the effects of pranayama breathing exercise as a supplement standard care on chemotherapy-induced symptom burden in women with breast cancer. However, the present study had some limitations. One of the limitations of the present study was that the patients performed breathing exercises at home, which reduced the researcher's supervision of the intervention. To address this limitation, the researcher called daily with the patients and encouraged them to perform breathing exercises regularly according to the specified schedule. Additionally, completing the diary by the researcher and sending an educational video about pranayama breathing exercises helped to address this limitation. Also, owing to the relatively small sample size, it was not possible to compare the effectiveness of pranayama breathing exercise in reducing individual MDASI symptoms. Therefore, future studies should be conducted with larger sample sizes. Another limitation of the present study was the use of self-report instrument, which led to subjective assessment of the outcome.
Pranayama breathing exercise, as a method of complementary and alternative medicine, can be trained by nurses to reduce the burden on women with breast cancer undergoing chemotherapy. Nurses have an important responsibility in managing the symptoms of patients undergoing chemotherapy, and it is necessary to evaluate the symptom burden in these patients before the start of treatment, during the chemotherapy period and even after the completion of the treatment period. Oncology nurses should develop their knowledge about different methods of pranayama breathing exercises. For this purpose, it is necessary for nursing managers to hold educational workshops and provide suitable conditions for nurses to participate in these programs.
In conclusion, pranayama breathing exercise effectively helped reduce the chemotherapy-induced symptom burden in women with breast cancer. Pranayama breathing exercise, as a home-based, inexpensive, accessible, and easy-to-learn complementary and alternative medicine method, can be used as an independent nursing intervention in the effective management of the chemotherapy-induced symptom burden in women with breast cancer. It is recommended that the pranayama breathing be considered as a component of comprehensive cancer care. Studies comparing the effects of other forms of pranayama exercises with different frequencies and durations are recommended to achieve more favorable results.
Data is provided as supplementary information files upon reasonable request.
- MDASI:
-
MD Anderson Symptom Inventory
- ECOG:
-
Eastern Cooperative Oncology Group
- CAM:
-
Complementary and alternative medicine
- CONSORT:
-
The Consolidated Standards of Reporting Trials
The authors would like to acknowledge all patients who participated in the study.
The current study is taken from the nursing master’s thesis. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
The current study adhered to the guidelines of the Declaration of Helsinki and was approved by the ethics committee of Qazvin University of Medical Sciences (ethics code: IR.QUMS. REC.1402. 262). Written informed consent was obtained from the participants after the purpose of the study was explained. Moreover, their right to refuse to participate in the study without disturbing medical treatment was emphasized.
Not applicable.
The authors declare no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Momeni, M., Khatooni, M., Alizadeh, A. et al. The effects of Pranayama breathing exercise on symptom burden among women with breast cancer undergoing chemotherapy: a randomized controlled trial. BMC Complement Med Ther 25, 242 (2025). https://doi.org/10.1186/s12906-025-04981-0