Journal of Medical Case Reports volume 19, Article number: 309 (2025) Cite this article
Owing to the activation of the endogenous fibrinolytic system, spontaneous restoration of coronary blood flow in the infarcted artery may seldom occur without thrombolysis or primary coronary intervention. Spontaneous reperfusion is associated with less myocardial damage, a tremendous in-hospital outcome, and a better overall prognosis compared with patients requiring reperfusion therapy to achieve a thrombolysis in myocardial infarction grade 3 patency. We present an intriguing case of spontaneous recanalization succeeding a subtotal left anterior descending occlusion in a 46-year-old male from Tanzania with neither positive history of cardiovascular disease nor apparent coronary artery disease risk.
A 46-year-old man of African origin was referred from central Tanzania for revascularization. He had presented with a 2-day history of ongoing central chest pain, crushing in nature and radiating to the left arm. His past medical history was unremarkable and had no apparent risk factors for coronary artery disease. Cardiac markers were found to be elevated, while electrocardiographic and echocardiographic evaluation revealed features in keeping with anterior wall myocardial infarction. He was prescribed the standard precatheterization medications and subsequently underwent an urgent coronary angiography. Catheterization revealed a 99% occlusion of the proximal left anterior descending with a thrombolysis in myocardial infarction grade 1 flow. Due to an intraprocedural machine fault and a lack of technical support, percutaneous coronary intervention could not be done in the same setting, and the patient was referred to Dar es Salaam for revascularization. The patient continued to be symptomatic for 5 days postcatheterization but came to Jakaya Kikwete Cardiac Institute (JKCI) free from symptoms on the ninth day since the onset of chest pain. He had stable hemodynamics and was in Killip class I. Cardioselective enzymes, a 12-lead electrocardiogram, and two-dimensional echocardiography done at this point revealed essentially normal findings, but the patient underwent a second catheterization for revascularization of a tight proximal left anterior descending lesion. Unexpectedly, coronary angiography revealed a patent left anterior descending vessel. Based on the clinical presentation, cardiac markers, and electrocardiographic and angiographic evolution, a diagnosis of spontaneous recanalization following subtotal proximal left anterior descending occlusion was entertained.
Spontaneous recanalization in patients with significant coronary lesions may seldom occur and portend a favorable prognosis. In light of the increasing incidence of acute coronary syndrome in Sub-Saharan Africa, it is crucial for primary physicians to recognize this potentially fatal entity timely and offer or refer for appropriate reperfusion therapy promptly. Parallel to this, efforts to raise public awareness, improve health-seeking behaviors, and strengthen emergency services are of utmost importance.
Sub-Saharan Africa (SSA) is witnessing an epidemic of cardiovascular diseases (CVDs) on an insurmountable scale [1]. Among CVDs, myocardial infarction (MI) is a major contributor to the global disease burden; however, the trends in the prevalence of ischemic heart disease (IHD) in the SSA region remains largely enigmatic [1,2,3,4]. Several obstacles including lack of reliable health statistics, absence of cause-specific mortality data, nonexistence of epidemiological surveillance systems for CVDs, dearth of appropriate diagnostic capabilities (echocardiography (ECHO) and electrocardiogram (ECG)), few interventional cardiology facilities and catheterization laboratories, and shortage of qualified staff have been implicated in the poor understanding of IHD epidemiology in SSA [1,2,3,4]. Faced with these shortcomings, scarcity of data in this setting is often, but wrongly, construed to imply relative infrequency of IHD [2, 3].
The commonest pathogenetic pathway in the development of acute MI is the formation of a coronary lumen thrombus following an atherosclerotic plaque rupture [5]. Additionally, coronary spasm or dynamic obstruction may occasionally but significantly cause acute coronary syndromes (ACS) in native arteries [5]. Reperfusion is the primary goal of treatment of ST-elevation myocardial infarction (STEMI). Successful reperfusion is vital in salvaging the myocardium with resultant improved quality and longevity of life [1,2,3,4,5]. Owing to the activation of the endogenous fibrinolytic system, spontaneous restoration of coronary blood flow in the infarcted artery may seldom occur without thrombolysis or primary coronary intervention (PCI) [6, 7]. Nevertheless, the cohort of patients experiencing spontaneous reperfusion have been documented to have largely insignificant infarcts with ultimate better left ventricular (LV) function and a more promising prognosis [6]. We present an interesting case of spontaneous recanalization succeeding a subtotal left anterior descending (LAD) occlusion in a 46-year-old male of African origin.
A 46-year-old man of African origin was referred to the National Cardiac Center—Dar es Salaam, Tanzania—for revascularization. He presented to a Zonal Referral Hospital—Dodoma, Tanzania—with a 2-day history of ongoing central chest pain, crushing in nature and radiating to the left arm. His past medical history was unremarkable, and he had a negative history of cigarette smoking, illicit drug use, hyperlipidemia, diabetes mellitus, hypertension, and premature family history of CVDs. Cardiac markers were elevated at presentation (that is, troponin I 4.70 ng/ml).
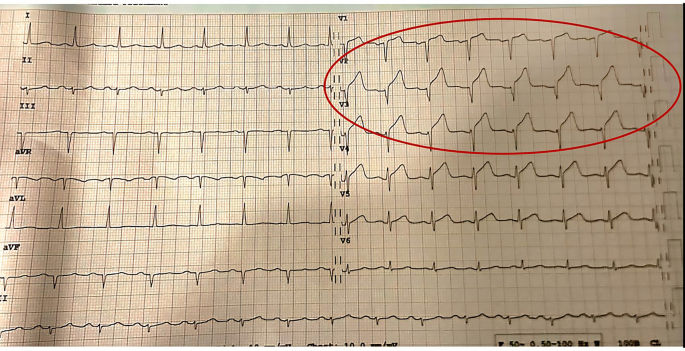
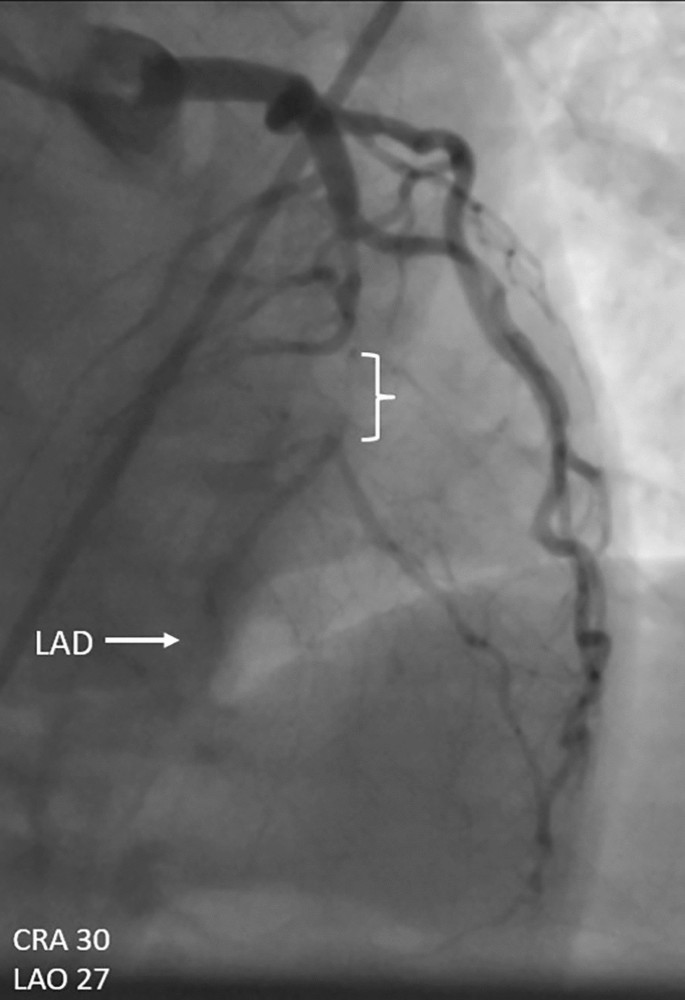
In congruence, electrocardiographic (ECG) evaluation revealed anterior STEMI (Fig. 1) while echocardiography (ECHO) was evident for dyskinesia of the anterior wall with preserved systolic functions (EF 56%). Patient was given a bolus of dual anti-platelet (clopidogrel 300 mg once daily (o.d.) and acetylsalicylic acid 300 mg o.d.) plus atorvastatin 80 mg and subsequently underwent an urgent coronary angiography (CAG) in Dodoma. Catheterization revealed a 99% abrupt proximal left anterior descending (LAD) artery occlusion with thrombolysis in myocardial infarction grade 1 (TIMI-1) flow and an intraluminal filling defect consistent with a thrombotic lesion (Fig. 2). There were no typical features of atherosclerotic disease, that is, evidence of plaque build-up, vessel remodeling, or calcification. Aspiration thrombectomy was not performed owing to the potential risk of distal embolization in the setting of a subtotal LAD occlusion. Given the absence of transient ischemic symptoms, a negative history of illicit drug use, energy drink abuse, or medication-induced vasospasm and the presence of angiographic features consistent with thrombotic occlusion, coronary vasospasm was considered unlikely.
Electrocardiogram-1 demonstrates an anterior ST-elevation myocardial infarction, evidenced by ST-segment elevation in leads V1–V4, as delineated by the surrounding oval
Coronary angiography-1 demonstrates subtotal occlusion of the proximal left anterior descending artery. The arrow indicates the affected vessel, while the bracket delineates the segment with the pathology
Due to intraprocedural machine fault and lack of technical support, PCI could not be done in the same setting, and the patient was referred to Dar es Salaam (443 km away) for revascularization. He was kept on acetylsalicylic acid 75 mg o.d., clopidogrel 75 mg o.d., isosorbide dinitrate 10 mg twice daily (b.d.), atorvastatin 40 mg o.d., ramipril 5 mg o.d., bisoprolol 5 mg o.d. plus enoxaparin sodium 70 mg o.d. and discharged on the second day of hospitalization. Due to financial constraints, he was unable to travel to Dar es Salaam in a timely manner. All potential complications of untreated STEMI were thoroughly discussed with the patient prior to his discharge against medical advice. Nevertheless, after discharge, he chose to visit a traditional healer, where he received unverifiable treatment.
Patient continued to be symptomatic for 5 days postcatheterization but came to the National Cardiac Center free from symptoms on the ninth day after the initiation of chest pain (i.e., 5 days postreferral to Jakaya Kikwete Cardiac Institute (JKCI)). He had stable hemodynamics (blood pressure (BP) 117/74 mmHg, pulse rate (PR) 87 beats/min, respiratory rate (RR) 21 breaths/minute, temperature 37.1 °C, and body mass index (BMI) 22.6 kg/m2) and was in Killip class I. Moreover, hematological and biochemical tests revealed normal findings. Cardioselective enzymes, a 12-lead ECG and two-dimensional (2D)-ECHO done at this point revealed essentially normal findings; nonetheless, the patient underwent a second catheterization for revascularization of a tight proximal LAD lesion.
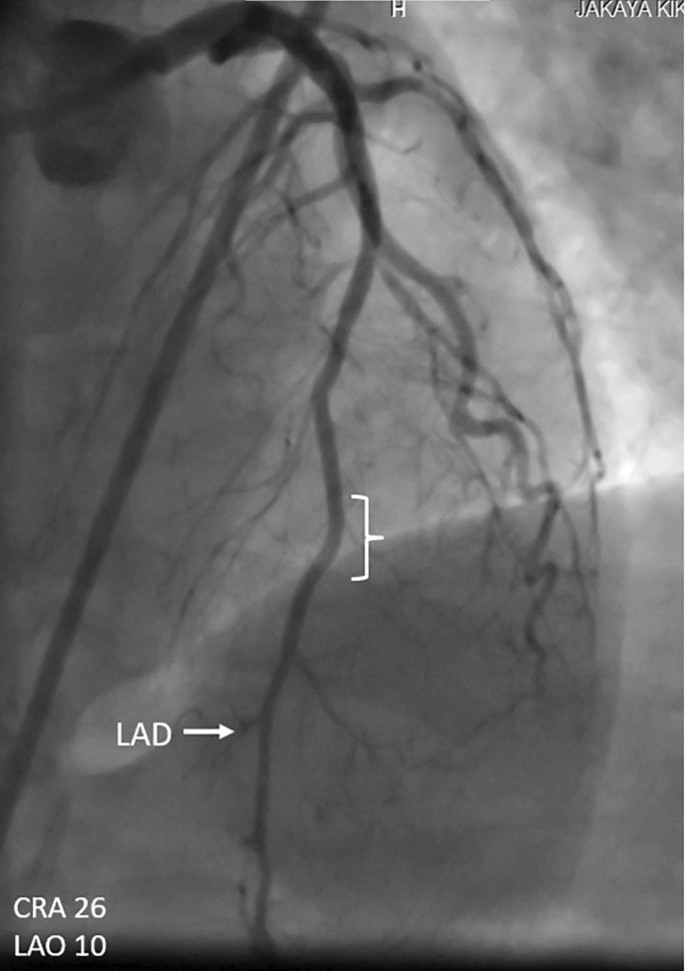
Unexpectedly, coronary catheterization revealed a patent LAD vessel (Fig. 3). Likewise, the remainder of coronary vasculature was essentially normal. Based on the clinical presentation, cardiac markers, and electrocardiographic and angiographic evolution, a diagnosis of spontaneous recanalization following subtotal proximal LAD occlusion was entertained. Prior to discharge, the patient was subjected to a stress ECG and 12-lead ECG together with ECHO, and there was neither chest pain nor signs of ischemia. We reviewed him 4 weeks later at our outpatient department, and he was in good health.
Coronary angiography-2 demonstrates a revascularized proximal left anterior descending artery. The arrow indicates the left anterior descending vessel, while the bracket highlights the reperfused segment corresponding to the prior pathology
Due to immediate reperfusion strategies and other guideline-directed treatment modalities, patients with MI exhibit better survival prospects in this era compared with their counterparts a few decades ago [8]. Regardless of this remarkable development, MI remains one of the leading causes of death and disability worldwide [9]. Be it total or partial, proximal or distal, occlusion of coronary arteries depends on the interplay between coagulation, anticoagulation, and fibrinolytic systems. To avoid chronic cardiac impairment, prompt reperfusion of the occluded artery by either pharmacologic and/or mechanical intervention has become the mainstay of therapy among patients with STEMI [10]. Irrespective of this wealth of evidence, diagnosis and optimization of the management of ACS in SSA pose a considerable challenge. [4, 11]
By contrast, spontaneous reperfusion has been reported in up to a quarter of patients experiencing acute STEMI caused by a thrombotic event [6, 7]. While the exact mechanism remains unclear, several hypotheses have been proposed to explain this phenomenon:
Although these mechanisms provide insight into spontaneous recanalization, their complex interplay likely determines the likelihood of reperfusion in individual cases. However, the unpredictability of this process and the lack of consensus on the optimal timing of intervention underscore the need for further research to identify reliable predictors and refine therapeutic strategies for patients with acute STEMI. Nevertheless, spontaneous reperfusion is associated with less myocardial damage, a tremendous in-hospital outcome, and a better overall prognosis compared with patients requiring reperfusion therapy to achieve a TIMI-3 patency. [17, 18]
In spite of the fairy-tale ending to this case report, numerous potentially life-saving lessons can be drawn. It is important to acknowledge that although plaque rupture characterizes a common unifying event for coronary thrombosis, a wide spectrum of symptomatology and outcome ranging between spontaneous recanalization and sudden death is probable. There was a delay of at least 2 days between onset of chest pain and arrival of the patient to the hospital. Furthermore, there was a 1-week delay between the diagnostic and interventional angiograms. Such delays underscore poor health-seeking behavior, a persistent challenge in SSA and many other underprivileged regions. [19]
As acute rupture of a coronary atheromatous plaque and subsequent coronary artery thrombosis is associated with the majority of sudden cardiac deaths, it is pivotal for both patients and medical staff to seek timely medical attention and observe the shortest possible medical contact-to-device time respectively. Moreover, as it is practically impossible to predict which of the MI subjects will experience a spontaneous recanalization, it is crucial to attend to this deadly medical emergency accordingly.
Additionally, with the rising burden of ischemic heart diseases (IHDs), particularly in resource-constrained settings like this one, there is an urgent need to raise public awareness about ACS, where prompt recognition and treatment are critical - after all, in such cases, “time is muscle.” Sadly, the patient in this case had to travel independently from home to the initial hospital and thereafter utilize public transport between the two hospitals, 8 hours apart. This observation underpins the worrying fact that emergency services in SSA and other resource-limited regions are largely lacking and, when present, the cost represents a formidable barrier [20, 21].
Spontaneous recanalization in patients with significant coronary lesions may seldom occur and portend a favorable prognosis. In light of the increasing incidence of ACS in SSA, it is crucial for primary physicians to recognize this potentially fatal entity timely and offer or refer for appropriate reperfusion therapy promptly. Concomitantly, efforts to raise public awareness, improve health-seeking behaviors, and strengthen emergency services are of utmost importance.
Not applicable.
- ACS:
-
Acute coronary syndrome
- BP:
-
Blood pressure
- CAG:
-
Coronary angiography
- CVD:
-
Cardiovascular diseases
- ECG:
-
Electrocardiogram
- ECHO:
-
Echocardiography
- IHD:
-
Ischemic heart disease
- LAD:
-
Left anterior descending
- LV:
-
Left ventricle
- MI:
-
Myocardial infarction
- PCI:
-
Percutaneous coronary intervention
- PR:
-
Pulse rate
- RR:
-
Respiratory rate
- SSA:
-
Sub-Saharan Africa
- STEMI:
-
ST-elevation myocardial infarction
- TIMI:
-
Thrombolysis in myocardial infarction
- tPA:
-
Tissue plasminogen activator
- uPA:
-
Urokinase-type plasminogen activator
The authors are grateful to the patient for giving us the opportunity to learn and to pass on the lessons learnt to others.
Not applicable.
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
The authors declare that they have no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Pallangyo, P., Bhalia, S.V., Longopa, G. et al. Spontaneous recanalization following subtotal proximal LAD occlusion: a case report. J Med Case Reports 19, 309 (2025). https://doi.org/10.1186/s13256-025-05369-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-025-05369-x