BMC Psychiatry volume 25, Article number: 276 (2025) Cite this article
Allergic rhinitis can cause symptoms to worsen after pregnancy and may cause problems such as postpartum depression. The goal of this study was to investigate the factors that influence postpartum depression in pregnant women with allergic rhinitis (AR).
We conducted a retrospective cohort study that included women with AR (based on self-reports) between June 2015 to June 2019 in Harvard University Partners Healthcare Systems (PARTNERS) in the USA. The study group was divided into postpartum depression and non-postpartum depression. Routine clinical and laboratory information was collected. Univariate and least absolute shrinkage and selection operator (LASSO, employed for predictor selection) regression analysis was used to study associations between AR during pollen seasons and adverse outcomes. Additionally, the receiver operating characteristic (ROC) curve evaluates discriminative ability by the area under the ROC curve (AUC). The calibration curve (DCA) was conducted to determine the clinical utility and benefit of the nomogram.
A total of 216 pregnant women with AR participated in this study. Univariate analysis showed that 7 indicators were significantly different (P < 0.05). LASSO and multivariable regression identified four predictors to construct a nomogram for PPD in pregnant women with AR, the four selected risk predictors are as follows: pollen season pregnancy (OR = 1.514, 95%CI: 0.771–2.973), history of preterm birth (OR = 2.723, 95%CI: 1.157–6.406), number of pregnancies (OR = 2.104, 95%CI: 1.356–3.267), anti-allergy medication during pregnancy (OR = 2.975, 95%CI: 1.521–5.819). The nomogram displayed good discrimination, with AUC of 0.732 (95% CI: 0.657–0.808). The risk of postpartum depression increased with the increasing risk score of predictive nomogram. The calibration curve and DCA present optimal predictive power.
We highlighted the comorbidity of AR and postpartum depression, and suggested that a multidisciplinary consideration between allergists and obstetricians or midwives is needed to ensure that pregnant women consult experts to reduce AR symptoms.
2018P002646.
• This study used the Harvard University Partners Healthcare Systems data for
allergic rhinitis pregnancy women research.
• Multiple logistic regression analysis was utilized to identify the risk factors associated with postpartum depression in pregnant women with rhinitis. Additionally, a nomogram was developed to forecast the occurrence of postpartum depression.
• This study suggests that fertility, a history of premature birth, and treatment for allergies during pregnancy are risk factors for postpartum depression.
• This study was a case-control study, and results need to be extrapolated more rigorously.
Allergic rhinitis (AR) is a prevalent chronic condition globally, marked by an inflammatory response triggered when inhaled particles contact the nasal mucosa, resulting in the production of immunoglobulin E (IgE) [1]. This condition affects roughly one in six people globally [2], with incidence rates varying by region: 9% in the US, 19% in Europe, 10% in Africa, 15% in Asia, and 38% in Oceania [3]. During pregnancy, increased blood volume and hormonal fluctuations can exacerbate allergic rhinitis (AR) symptoms in about one-third of women. Pregnant women with AR often experience discomfort, with rhinorrhea and recurrent sneezing being the most common symptoms [4]. Furthermore, mothers with AR in the USA are at risk of delivering babies with low birth weight and preterm birth [5]. In addition to physical symptoms, AR during pregnancy is often accompanied by psychological distress, such as anxiety and depression, further complicating maternal health. Maternal allergic conditions, including AR, have been linked to perceived maternal stress during late pregnancy [6]. These conditions are often accompanied by psychological distress, including anxiety and depression, in pregnant women [7]. Importantly, pregnant women with AR exhibit significantly lower serum vitamin E levels compared to healthy pregnant women, and additionally, the serum level of vitamin E was negatively correlated with the total nasal symptom score [8]. A population-based case cohort study of 199,470 deliveries from the National Health Insurance Research Database (NHIRD) data between 2000 and 2010 was included, Univariate and multivariable regression analyses showed that AR was significantly associated with increased odds of PPD, this deficiency is significantly associated with a roughly 50% increased risk of postpartum depression (PPD) in women who give birth while experiencing AR [9], highlighting the multifaceted impact of this condition.
PPD is a common, debilitating, but treatable condition. A history of mood or anxiety disorders, especially with active symptoms during pregnancy, is the primary risk factor [10]. It disrupts the interactions between mothers and infants, which are essential for the child’s development. The bond a mother forms with her child, her responsiveness, and her parenting approach are crucial for the healthy development of the infant’s social, cognitive, and behavioral skills. Depressed mothers often show reduced attachment, decreased sensitivity, and tend to engage in harsher or more inconsistent parenting practices. These behaviors may contribute to the documented negative outcomes in children raised by mothers with depression [11]. Previous studies indicate that individuals with allergic rhinitis (AR) frequently experience both nasal symptoms and psychological issues, including depression [12]. Depression complicates the management of AR, making it more difficult and costly. Moreover, it significantly impairs patients’ daily functioning and overall well-being, placing additional burdens on both families and society [13]. Identifying the association between AR and PPD is vital to mitigate the impact of this common childbirth complication. Early identification allows for the implementation of proactive interventions, ensuring the best possible outcomes for mothers, infants, and families [14].
While numerous studies explore the link between AR and depression [15], research specifically examining the relationship between AR and PPD is less prevalent. Given the vulnerability of pregnant women, AR may increase the risk of PPD. Various risk factors for PPD have been identified, encompassing demographic, clinical, psychosocial, marital, parity, and neonatal health aspects [9]. The use of anti-allergic medications by pregnant women with AR, along with changes in their psychological state during pregnancy, are all risk factors for PPD. Therefore, this population-based study was conducted to examine the association between AR and PPD, addressing an existing knowledge gap. This study intends to retrospectively analyze the influencing factors of postpartum depression in pregnant women with allergic rhinitis through multi-center data, and develop perinatal management strategies for pregnant women with allergic rhinitis to avoid adverse clinical outcomes.
This retrospective study analyzed data from June 2015 to June 2019 across the Harvard University Partners Healthcare System (PARTNERS), covering seven hospitals: Brigham and Women’s Hospital, Massachusetts General Hospital, Newton-Wellesley Hospital, North Shore Medical Center, Martha’s Vineyard Hospital, Cooly Dickinson Hospital and Nantucket Cottage Hospital. Cases of AR in pregnant women were identified using the EPIC system through International Classification of Diseases (ICD) codes. AR was diagnosed based on laboratory tests, clinical symptoms, and documented allergies during pregnancy, as recorded in hospital files. Severe congenital malformations and multiple pregnancies are established risk factors for PPD [16, 17], therefore, this study excluded cases involving severe congenital malformations, such as chromosomal abnormalities or multiple anomalies, as well as all multiple pregnancies. Maternal demographics (age, parity, ethnicity, last menstrual period, BMI), obstetric and medical history, biochemical parameters (leukocyte, red blood cell, platelet counts), treatment, and pregnancy outcomes (birthweight, sex, delivery mode, Apgar score, pain score, PPD) were collected from hospital records for all AR cases.
The study received ethical approval from Harvard University Partners Healthcare Systems under approval number 2018P002646.
A history of AR was considered positive if the woman had experienced the disease in any prior pregnancy. Pollen season is defined from May to August. Adverse pregnancy outcomes included delivery mode, preterm births (< 37 weeks, spontaneous or induced), and postpartum hemorrhage (> 1000 mL), small-for-gestational-age infants (birth weight below the 10th percentile), neonatal asphyxia (pHa < 7.05 with base deficit > 12 mmol/L or pHa < 7.00) [18], low Apgar scores (< 7 at 5 min), admissions to medium and neonatal intensive care units, and perinatal deaths from 24 weeks of gestation to 7 days post-delivery.
Additionally, late preterm births were specifically defined as those occurring between 34 weeks 0 days and 36 weeks 6 days of gestation. The outcome measures were based on extensive prior research on adverse reproductive outcomes and aligned with national guidelines. The Depression Screener Questionaire, a nine-item screening tool based on DSM-V criteria for depression, was used to assess PPD. A score of 10 or higher indicated major depression.
After conducting the Shapiro-Wilk test, all the continuous variables exhibited abnormal distribution. Therefore, continuous data were expressed as the median [25th percentile, 75th percentile]. Categorical variables were expressed as counts (percentages). Clinical characteristics were compared using the Mann-Whitney U test (continuous variables) and chi-square test (categorical variables). LASSO regression was selected for its ability to handle multicollinearity and identify the most predictive variables (P < 0.1), enhancing the nomogram’s reliability. The nomogram was developed using a binary logistic regression model with five-fold cross-validation. The factors included in the nomogram were selected based on multivariable analysis. To verify the positioning of the points on the “Total Points” axis, predictor lines were extended upwards, and then projected downwards onto the lower scales, which helped determine the likelihood of puerperal infection. To evaluate the accuracy of the predictive model, a calibration curve was utilized, and the Hosmer-Lemeshow test was used to assess the difference between the predicted values and actual values to evaluate the model fit. Additionally, the receiver operating characteristic (ROC) curve evaluates discriminative ability by the area under the ROC curve (AUC). Calibration curve analysis (DCA) were used to assess the nomogram’s accuracy and clinical applicability.
Statistical analyses were performed using R software version 4.4.1 (http://www.rproject.org), specifically employing the “rms” and “glmnet” packages. Lasso regression was performed using the “glmnet” package in R version 4.4.1. The “rms” package was used to construct binary logistic regression models and generate calibration curves. ROC curves were plotted using the “pROC” package. A p-value of < 0.05 was considered statistically significant.
The total number of pregnant women with AR was 216, including 65 diagnosed with PPD and 151 without PPD. Maternal characteristics are detailed in Tables 1 and 2, categorized by various data classifications. The median age of mothers was 34 years (IQR: 31.00–37.25), with those experiencing PPD having a median age of 35 years (IQR: 31.00–38.00) and those without having a median age of 34 years (IQR: 31.00–36.00). The Mann-Whitney U test revealed statistically significant differences in gravidity, parity, and gestational weight gain (P < 0.05). The chi-square test revealed significance (P < 0.05) for categorical variables including pregnancy during pollen season, history of preterm birth, history of spontaneous abortion, and use of anti-allergy medication during pregnancy.
We conducted a LASSO regression analysis, selecting the predictive factors from the univariate analysis (P < 0.1), including age, maternal weight, gravidity, parity, gestational weight gain, Apgar 1 min score, pollen season pregnancy, history of preterm birth, history of spontaneous abortion and anti-allergy medication during pregnancy. LASSO regression analysis indicated that pregnancy during the pollen season, history of preterm birth, number of pregnancies, and use of anti-allergy medication during pregnancy were more significant in predicting PPD in pregnant women with AR (Table 3).
We developed a binary logistic regression model based on factors selected from the LASSO regression analysis, including pregnancy during the pollen season (OR = 1.514, 95% CI: 0.771–2.973), history of preterm birth (OR = 2.723, 95% CI: 1.157–6.406), number of pregnancies (OR = 2.104, 95% CI: 1.356–3.267), and use of anti-allergy medication during pregnancy (OR = 2.975, 95% CI: 1.521–5.819) (Table 4).
Figure 1 illustrates a nomogram constructed from the four aforementioned clinical features to assess the risk of PPD in pregnant women with AR. Among the predictive factors identified, the number of pregnancies exhibited the strongest association with postpartum depression risk, followed by anti-allergy medication use during pregnancy, history of preterm birth, and pregnancy occurring during the pollen season.
A nomogram using four available clinical features to predict the risk of PPD in pregnant women with AR
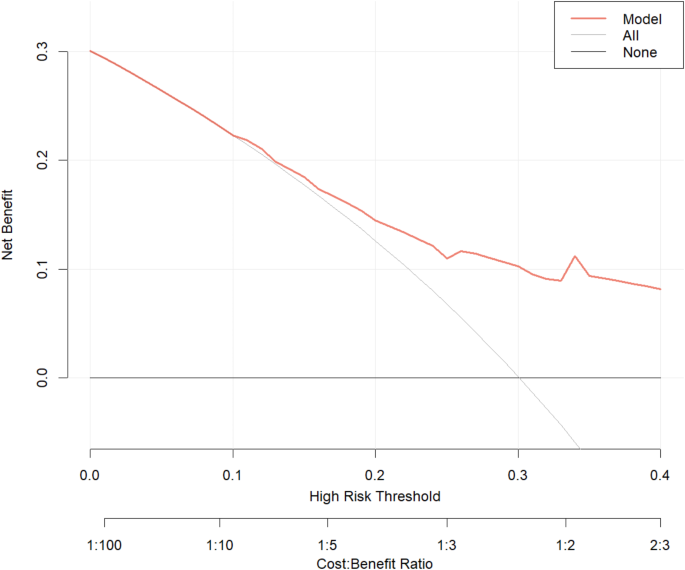
We evaluated the model’s discriminative ability using the receiver operating characteristic (ROC) curve and assessed its fit with the Hosmer-Lemeshow test (Fig. 2). The ROC curve’s area (AUC) was 0.732 (95% CI: 0.657–0.808), demonstrating good predictive value (Fig. 3). Furthermore, decision curve analysis (DCA) demonstrated that the predictive model provided considerable net benefits across most threshold probabilities (Fig. 4).
The calibration curve of four available clinical features to predict the risk of PPD in pregnant women with AR
In summary, our analysis highlights key predictive factors for postpartum depression in women with AR, including the number of pregnancies, anti-allergy medication use during pregnancy, and history of preterm birth. The predictive model demonstrated robust performance with an AUC of 0.732, supporting its potential utility in clinical settings.
This study investigated the risk factors for PPD among patients with allergic rhinitis (AR) using data from the Harvard University Partners Healthcare Systems. We found that the incidence of PPD in patients with AR is approximately 30%. Multivariable regression analysis revealed that multiparity, a maternal history of preterm delivery, and allergy treatments during pregnancy were significant risk factors for PPD. Univariate analysis revealed that pregnancy during pollen season, reduced gestational weight gain, and a maternal history of spontaneous abortion were linked to a heightened risk of PPD.
Studies suggest that the global incidence of allergic rhinitis (AR) varies between 10% and 40%, with 36% of women frequently affected [19, 20]. Characteristics of pregnant women with AR include older age, higher education levels, living in urban areas, and an increased likelihood of physical and pregnancy-related complications [21]. Research indicates a potential link between allergic rhinitis (AR) and heightened risk of adverse pregnancy outcomes. In the general adult population, there is a recognized link between atopic symptoms and depression, with allergic diseases in females being associated with mental disorders. Yu et al. reported that patients with AR experienced a 37% higher risk of PPD [22]. However, Brunner et al. found that the association between allergic diseases and PPD has been inconsistent [23]. A systematic review of six studies found a correlation between AR and PPD in women [24]. Similarly, Lu et al. confirmed that AR was closely related to perinatal mental disorders [25]. Our study’s findings align with existing reports, indicating an association between PPD and AR.
Tai et al. demonstrated that both primiparous and multiparous women exhibited similar rates of PPD [26]. Our study identified multiparity as a risk factor for PPD, contrasting with previous findings. This discrepancy might be attributed to shifts in circumstances, including family or work situations. A workplace that allows breaks is preferred, as social interaction during these times reduces stress more effectively than prolonged period at home [27]. Additionally, household chores, particularly kitchen work, may exacerbate AR symptoms.
Allergic symptoms are exacerbated during pregnancy, but in fear of adverse events and birth defects, only a small percentage of women take anti-allergy medications during this period, which do not effectively control the disease [28]. In our study, allergy treatment during pregnancy was found to be a high risk factor for PPD. Usually, women stop using allergy treatment medications during pregnancy. However, if their symptoms worsen, they may need to continue allergy treatments throughout pregnancy. We hypothesized that heightened allergic inflammation and worsening allergic rhinitis (AR) may elevate the risk of PPD.
Gestational weight gain has been associated with numerous adverse pregnancy outcomes. In this report, we found that insufficient gestational weight gain increases the risk of PPD. Weight gain during pregnancy is significantly affected by physical activity. This important lifestyle factor affects maternal well-being, as physically active women have a lower risk of PPD [29]. Notably, 80% of women diagnosed with allergic rhinitis (AR) limited their physical activity, which contributed to a higher incidence of PPD. A history of premature delivery and spontaneous abortion is linked to a higher risk of PPD in patients with allergic rhinitis (AR). A possible explanation for this could be a poor intrauterine environment and a dysregulated inflammatory response [30]. Surprisingly, being pregnant during pollen season may increase the risk of PPD. Our findings align with earlier research indicating a stronger association in women giving birth in spring (HR = 1.49; 95% CI 1.27–1.75), which diminishes for those giving birth in summer [31]. In patients with allergic rhinitis, symptom exacerbation was linked to the period from December to February and the second trimester of pregnancy. A possible explanation for this finding could be a dysregulated inflammatory response during the pollen season.
Pregnancy can intensify depressive symptoms, potentially affecting child-rearing and leading to PPD and parenting challenges. Pregnant women with allergic diseases, including allergic rhinitis, face a higher risk of depression and reduced quality of life. The postpartum period is a critical phase of neuroplasticity in women, influenced by immune molecules and hormonal changes, increasing susceptibility to psychiatric disorders. Postpartum mental disorders are associated with immune-related conditions like gestational diabetes mellitus, pre-eclampsia, and inflammatory bowel disease, though the exact mechanisms remain unclear [32]. Inflammatory dysregulation may contribute to the development of PPD. AR involves an abnormal inflammatory response that could initiate PPD. Therefore, the potential association between AR and PPD should receive greater attention from society.
During pregnancy, cytokine production differs between allergic and non-allergic women, with allergic individuals exhibiting an enhanced Th2 response [33]. Perinatal women undergo systemic immune changes, and during pregnancy, adherence to medication treatments is often poor. These factors make allergic diseases difficult to control during the perinatal period. Severe allergic symptoms can cause sleep disturbances due to severe breathing difficulties, which in turn increase psychological stress [34]. Furthermore, allergic reactions may cause immune system dysregulation, which may trigger subsequent mental disorders. In addition, an allergic reaction may cause dysregulation of the immune system, which in turn may trigger subsequent psychiatric disorders. Peripheral inflammation from the nasal cavity first leads to dysregulation of factors such as interleukin-6 and interleukin-1β, and the dysregulated inflammatory cytokines in turn affect the brain [35]. These mechanisms potentially explain our findings and further substantiate the increased risk of postpartum psychiatric disorders in women with AR.
Our study has both strengths and limitations. Initially, we concentrated on identifying risk factors for PPD in patients with AR. We analyzed data from Harvard University Partners Healthcare Systems, which covering seven hospitals with population diversity, using multiple logistic regression to identify risk factors for PPD in pregnant women with rhinitis. However, the study may be influenced by analytical methods, confounding factors, sample size and data quality. And the potential biases included demographic representativeness, missing data, socioeconomic status, and regional variability in pollen exposure. Besides, as this was a case-control study, the findings should be interpreted with caution. Further research with expanded sample sizes and extended follow-up durations, particularly in non-Western or rural settings, is necessary to confirm these findings. Finally, an analysis of the potential mechanisms was not performed. Therefore, we will also propose experimental designs or future studies to validate these hypotheses.
In summary, this study suggests that multiparity, a maternal history of premature delivery, and allergy treatments during pregnancy are high-risk factors for PPD. Additionally, being pregnant during the pollen season, insufficient gestational weight gain, and a maternal history of spontaneous abortion also increase the risk. Our study underscores the comorbidity of AR and PPD, advocating for multidisciplinary collaboration among allergists, obstetricians, and midwives to provide pregnant women with expert consultation for effective AR symptom management. Allergists focus on the diagnosis and treatment of allergic rhinitis, and obstetricians, and midwives focus on the management of perinatal period.
No datasets were generated or analysed during the current study.
- SPB:
-
Spontaneous preterm birth
- GDM:
-
Gestational weight gain
- AR:
-
Allergic rhinitis
- AUC:
-
Area under the ROC curve
- CIs:
-
Confidence intervals
- LASSO:
-
Least absolute shrinkage and selection operator
This work was supported by Chongqing Medical University Education and Teaching Research Project (grant number: JY190211) and the Teaching and Research Project of Chongqing Pharmaceutical Vocational Education Group (grant number: CQZJ202015) and Chongqing Science and Health Joint Medical Research Program (grant number: 2024QNXM029).
Ethical approval for the trial was obtained from the Harvard University Partners Healthcare Systems in the USA on November 15, 2018 under approval number 2018P002646.
Not applicable.
Not required.
The authors declare no competing interests.
not applicable.
Not commissioned; externally peer reviewed.
This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Li, F., Liao, Y., Lei, C. et al. Risk factors for postpartum depression in pregnant women with allergic rhinitis: a retrospective study. BMC Psychiatry 25, 276 (2025). https://doi.org/10.1186/s12888-025-06702-w