BMC Medical Education volume 25, Article number: 126 (2025) Cite this article
The involvement of undergraduate medical students in research is pivotal for the advancement of evidence-based clinical practice. This study aimed to assess the extent of research involvement and the factors influencing it among undergraduate medical students in Bangladesh.
A multi-center cross-sectional study involving 2864 medical students from both public and private medical colleges was conducted between June and December 2023. Data on demographics, research involvement, participation in research training, future career aspirations in research, and obstacles encountered by students were collected. Statistical analyses were performed using SPSS 25.
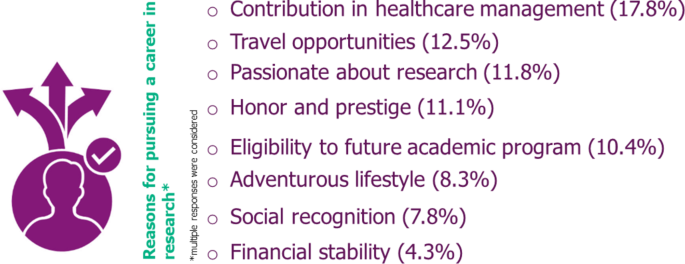
The mean age of the students was 21.8 ± 1.8 (SD) years, with the majority being female (61.8%). Overall, 21.5% (n = 617) were actively participating in research beyond academic activities. Approximately 7% (n = 205) had undergone formal research training, and 6.5% (n = 187) had experience in publications in peer-reviewed journals as first authors or coauthors. A total of 45.5% of the students faced multiple challenges during participating in research, with the two most difficult tasks being designing a study (26.7%) and data collection and recruitment of study participants (19.6%). Almost half of the students (47.2%, n = 1352) showed an interest in pursuing a research career in the near future. The primary barriers preventing students from choosing a future research career were insufficient mentorship (16.3%), the perception of a lengthy career path (17.2%), and limited funding opportunities (15.9%). Factors that significantly encouraged research involvement included being male (adjusted odds ratio [aOR] 1.5, 95% CI: 1.2–1.8), studying in the senior academic phase (aOR 3.9, 95% CI: 2.7–5.6), previous education from an English-medium educational institute (aOR 1.8, 95% CI: 1.2–2.2), and encouragement from faculty (aOR 1.4, 95% CI: 1.1–1.7).
The proportion of research participation among the students was relatively low. To promote research engagement among undergraduate medical students in Bangladesh, comprehensive policy formulation and strong commitment at the highest levels are essential. Integrating national research policy into the curriculum could serve as a strategic measure for achieving this objective.
Integrating research training in medical education equips medical students with up-to-date knowledge, enhances their critical and analytical thinking and lays the foundation for evidence-based clinical practice [1, 2]. Early research exposure significantly influences the career paths of medical graduates, it increases the likelihood of cultivating physician-scientists over purely clinical practitioners, greater scientific productivity through publications, citations, and grant success, while promoting translational medicine practices that bridges gaps between scientific research and patient care, ultimately driving healthcare advancements [3, 4].
Despite the recognized importance of health research, research training during undergraduate medical education in developing countries continues to be inadequate, poorly organized, constrained and fraught with challenges, contributing to a decreased volume and quality of research being conducted and published [5,6,7,8,9]. This inequality can stem from various factors, including curriculum differences, funding availability, infrastructure, access to resources, and institutional support for research [9,10,11].
In Bangladesh, students begin their undergraduate medical education, known as the Bachelor of Medicine and Bachelor of Surgery (MBBS), immediately after high school (after 12 years of schooling) [12, 13]. This is typically their first opportunity to engage in and gain exposure to research activities, which is similar to other South Asian countries such as Pakistan and India [14, 15]Whereas, in developed countries such as the USA and Canada, many students enter medical school with prior research experience, as they often engage in research during their undergraduate studies before commencing medical education [16, 17]. This early exposure provides them with a strong foundation in research methods and processes, leading to greater proficiency and involvement in research during their medical training compared to medical students in developing countries [18].
Despite the students’ eagerness to engage in research activities, they frequently encounter numerous barriers that can diminish their interest in pursuing a career in research [19,20,21]. Ferdoush et al. reported that Bangladeshi undergraduate medical students exhibited a positive attitude toward research but faced significant challenges, such as limited time due to academic pressures, inadequate guidance, unfamiliarity with research methods, and difficulty with statistical analysis [19]. Additionally, a minority of postgraduate medical students in Bangladesh demonstrated satisfactory biomedical research practices, with even fewer publishing their findings in journals [20]. The barriers to research among clinicians include conflicting roles as clinicians and scientists, insufficient research exposure and support, lack of recognition and financial rewards for research efforts, and pursuing research topics lacking scientific significance [21]. These challenges collectively inhibit scientific productivity among medical students and clinicians in Bangladesh.
To encourage research culture and foster the development of inquiry and research-based learning among medical students, understanding the level of research engagement, associated factors, perceived obstacles, and aspirations for future research careers among undergraduate medical students in Bangladesh is crucial. While existing studies [19,20,21] have explored attitudes towards and barriers to research among medical students, postgraduate trainees and clinicians, there is a lack of detailed, context-specific analysis in Bangladesh. Our study fills this gap by exploring the specific factors that are responsible for research involvement among undergraduate medical students in Bangladesh.
The primary goal of this study was to explore the level of research engagement and the factors influencing involvement among medical students in Bangladesh. The findings from this study will provide medical education governing bodies and councils with insights into the current research culture among medical students. This will facilitate the implementation of essential curriculum changes to foster a more research-oriented and student-centered approach within undergraduate medical education.
In terms of structure, curriculum, and training programs, the Bangladesh medical education system aligns with a problem-based learning and examination-focused approach. The MBBS program typically spans five years and is structured into four academic phases that are assessed by professional examinations. The first phase (one and a half years) includes Anatomy, Physiology, and Biochemistry. The second phase (one year) encompasses Pharmacology and Forensic Medicine & Toxicology. The third phase (one year) involves Community Medicine, Pathology, and Microbiology. The fourth/final phase (one and a half years) includes Medicine, Surgery, and Obstetrics & Gynecology [12]. Lectures across all phases of the curriculum tend to prioritize textbook-based knowledge, emphasizing well-established information rather than current research findings, epidemiological data, and methodological advancements. Therefore, the integration of new research approaches and findings into practical contexts is often limited. Only in the third phase of the curriculum, students learn and acquire essential research skills through the mandatory “Community Medicine” course. This course includes modules on research, epidemiology, and public health, with two key modules: ‘Research Methodology & Biostatistics’ and ‘Principles of Epidemiology’, specifically designed to develop research skills. Combined, these modules offer about 53 h of instruction, with approximately 23 h devoted to research methodology and biostatistics. Additionally, students must participate in a residential field site training (RFST) program and submit a survey report to fulfill the requirements of the Community Medicine coursework [22]. The RFST option is incorporated into the curriculum to familiarize students with the practical aspects of the research process. However, there is currently no mechanism in place to verify whether students achieve the expected competencies and outcomes in real-life settings (Fig. 1).
Study settings and population
This country-wide multi-center cross-sectional study was conducted among medical students who were enrolled in the Bachelor of Medicine, Bachelor of Surgery (MBBS) program in different locations of Bangladesh, irrespective of whether the students were from private or public entities. Study sites were selected for their accessibility, with a preference for medical universities that also had teaching hospitals to provide a wide range of academic and clinical perspectives. We also considered the timeframe available for data collection when selecting the centers. The study included undergraduate medical students from all academic phases, but excluded those who had completed their final professional examination and were currently in the internship program.
An estimated sample size of 2214 participants was calculated using the Cochran (1977) [n = z2pq/d2] formula [17], with a prevalence of 50%, a margin of error of 5% at the 95% confidence interval, an intraclass correlation coefficient = 0.2, a design effect = 5 and a 15% non-response rate. The participants were obtained by convenience sampling, and a total of 2942 students participated in this study. After excluding 78 students due to missing or incomplete data, 2864 students were included in the final analysis. The details of the participant selection process are shown in the Supplementary file (Figure S1).
Method of data collection
We utilized a self-administered semi-structured questionnaire via both physical and online methods (Google Forms) to collect our data. Both the online and physical questionnaires were carefully crafted to maintain consistent structures, question wording, and response options, ensuring that participants received uniform information and instructions regardless of their chosen format. In both versions of the questionnaire, participants were asked to provide their email addresses. To prevent duplication, the research team cross-checked these email addresses. If an email address appeared in both formats, only one response was considered to avoid counting duplicate data from the same individual. Additionally, responses from online questionnaires were excluded if they originated from medical colleges where the data had already been collected through physical visits. This step ensured that each participant’s responses were unique to one method of data collection, thereby safeguarding the integrity of the data.
The questionnaire consisted of items about demographic characteristics along with four major themes: (i) voluntary research involvement, (ii) self-perceived research competence, (iii) research barriers and challenges and (iv) future aspirations in research career. Questions pertaining to voluntary research involvement and self-perceived research competence required a yes/no response, whereas items relating to research barriers and challenges and future aspiration in research career were evaluated based on statements/short answers, checkboxes, yes/no responses and a 5-point Likert scale. The components/themes of the questionnaire are provided in Supplementary Table S1. Certain sections of the questionnaire were adapted from previously published studies [8, 9, 11] and additional items were added to further characterize the demographic profile and research perspective of our study population. Prior to data collection, we pretested the questionnaire on a convenient sample of 20 respondents. The majority (17 out of 20) reported no difficulties with question clarity, comprehension, or appropriateness, and their responses were excluded from the final analysis. We collected the data via two methods: utilizing online social media platforms through a Google questionnaire and visiting medical schools (termed medical colleges in Bangladesh) and distributing the questionnaire to students.
Data management and analysis
The data were entered, and any inconsistencies were cross-checked against the original data to ensure accuracy and reliability. Questionnaires with more than 50% of their questions left unanswered were considered invalid due to inconsistencies in responses and were excluded from the analysis (n = 36). For statistical analysis, we utilized the Statistical Package for Social Sciences version 25.0 (IBM Co., Armonk, NY, USA). Categorical variables were expressed as counts (percentages), and continuous variables were expressed as the means (± standard deviations [SDs]). We used a binary logistic regression model to assess the factors associated with research involvement (the dependent variable). Based on previous literature and study country’s context, we included explanatory variables such as age, gender, type of medical school, medium of instruction, study phase, faculty encouragement, pursuing a research career in future and challenges faced. In the unadjusted analysis, we examined each variable individually to identify significant associations. For the final adjusted model, we included only variables with at least one statistically significant category (p-value ≤ 0.05) in the unadjusted analysis. This approach allowed us to account for potential confounders while keeping the model focused and interpretable.
Ethical consideration
The study protocol was approved by the Ethics Committee of Public Health Foundation Bangladesh (PHF-NG-1003) and followed the principles of the Declaration of Helsinki. Prior to data collection, we obtained informed written consent from all participants. We employed a secure and encrypted survey platform to maintain confidentiality and data security for online responses. Additionally, participants were thoroughly informed about the utilization of their data, emphasizing its confidentiality and exclusive application for research purposes. This information was clearly conveyed on both the physical questionnaires and the online survey landing page.
The mean age of the participants was 21.8 ± 1.8 (SD) years. Two-thirds of the participants were females (61.8%) and were studying in government/public medical schools (65.1%), and half of the participants were either in the third (23.7%) or fourth phase (23.4%) of the study. Most of the participants (86.7%) had Bangla as the medium of instruction in primary and high school (Table 1).
Although most of the respondents (92.6%) indicated that they had heard about health research, less than one-third (21.5%) of the respondents volunteered to participate in research projects outside of the academic curriculum. Approximately 7% of the students published their research in peer-reviewed journals, of which 2.3% were the first author of the research paper. Regarding self-perceived research competency, only 7.2% of respondents received formal research training. A total of 38.7% of respondents reported that they regularly read medical journals (in addition to textbooks) (Table 2).
Almost half of the respondents (45.5%) stated that they faced obstacles or challenges during their research activities, with females experiencing more challenges (57.8%,p < 0.001) compared to their male counterparts (42.2%), irrespective of their prior participation in research activities or volunteeri (Fig. 2). Also, the most challenging research procedure was framing the study design (26.7%), followed by data collection and recruitment of the study participants (19.6%). Moreover, two-thirds (63.8%) mentioned receiving encouragement from their faculty members, however lack of mentors and advisors was the most common reason (16.3%) for them to be skeptical about pursuing a career in health research in the future (Table 3).
Gender differences in encountering obstacles/challenges during research activities (n = 1304). * chi-square test revealed significant difference in encountering obstacles/challenges based on gender (p < 0.001)
Almost half of the respondents (47.2%) expressed their intention to pursue career in research in the near future and 70.8% expressed their interest to volunteer in research activities to acquire more research experience during their undergraduate studies. The top reasons behind their intentions to pursue a research career were contributing to healthcare management (17.8%), travel opportunities (12.5%), passion for research (11.8%), and honor & prestige (11.1%) (Fig. 3). Most of them (82.3%) recommended greater emphasis on practical-oriented research courses during their undergraduate studies (Tables 2 and 3).Please note that the figures are renumbered to maintain sequential order. Please check and confirm the change.Thank you for the reminder. We have checked and have made amendments to the figures. Please change figure 2 as 'figure 3' and figure 3 as 'figure 2'.
Among the medical students with previous research experience (n = 617), most students were female (54.3%, n = 335), were in their senior year of medical school (65.5%, n = 404) and received encouragement from institution faculty members (70.7%, n = 436). One-third (65%, n = 401) of the students involved in the research faced barriers and obstacles during the research activity and more than half of the students expressed an intention to pursue a research career in the future (52.2%, n = 436).
The results of both unadjusted and adjusted odds ratios for research involvement are presented in Table 4. The multivariate adjusted odds ratios revealed that, compared with their female peers, male students demonstrated a greater inclination toward research involvement (adjusted odds ratio [aOR] 1.5, 95% CI: 1.2–1.8). Moreover, enrollment in the senior year of medical school (aOR 3.9, 95% CI: 2.7–5.6), previous education from an English-medium educational institute (aOR 1.8, 95% CI: 1.2–2.2) and receiving encouragement from faculty members (aOR 1.4, 95% CI: 1.1–1.7) collectively contributed to influencing medical students to be involved in research activities (Table 4).
Our study revealed a notable gap between the interest (70.8%) and actual participation (21.5%) of medical students in research during their undergraduate years in Bangladesh. This gap may arise from the way students are taught throughout their medical education. The curriculum relies heavily on textbooks and focuses more on memorizing facts than on encouraging critical thinking. Additionally, there is not much emphasis on current research, epidemiological evidence, or the methods needed for conducting research [12, 22]. As a result, students are not encouraged or informed about the importance of becoming involved in research, which leads to a lack of interest and participation in research.
In the present study, research engagement was found to be greater among male students and those in more advanced academic phases (3rd and 4th phases) than among their peers. Previous studies conducted in Bangladesh have indicated that male medical students are more inclined toward careers in research-related fields such as public health rather than clinical practice [23]. The reasons behind this gender disparity in research involvement are multifaceted in our context. Factors such as a lack of female mentorship figures, persistent sexism within research environments (including assumptions that females may face challenges such as travel restrictions for fieldwork), concepts of traditional gender roles, and differing career preferences (such as a preference for clinical practice over academia) contribute to this imbalance [24,25,26], as evident in this study with females experiencing more challenges in during research activities compared to male counterparts. Additionally, students with more years of education often engage more in research activities because they are exposed to subjects such as community medicine, which provides foundational research skills and fosters enthusiasm for research participation. Furthermore, interactions with academic physicians in these later years may enhance opportunities for students to establish relationships with academic mentors, further encouraging their involvement in research [27].
Most of the students in this study noted that their research methodology, including study design, sampling techniques, study procedures, and data collection, were quite challenging. This observation is consistent with findings from other studies [19, 28, 29]. In the MBBS curriculum in Bangladesh, academic training on research methodology and biostatistics is limited to a single module within the Community Medicine course, covering approximately 23 teaching hours [30]. This limited exposure is insufficient for thoroughly covering all necessary topics, making it difficult for medical students to acquire a comprehensive understanding of research methodology. The compressed nature of this training means that students often struggle to grasp the complexities of research, leaving them demotivated to engage in research. Another significant challenge identified in the study is the lack of proficiency in the English language, as evidenced by the fact that students with previous education in English were more likely to engage in research activities. This trend aligns with findings from other studies [31, 32]. Proficiency in English is essential for comprehending research terminology, writing grant proposals and composing research papers. Medical students, particularly those from suburban and rural areas with less exposure to English, often lack the confidence needed for scientific writing and effective communication with professors and faculty members, which eventually discourages them from participating in research activities.
Numerous studies have emphasized the crucial role of school support for students, with teachers serving as primary guides to ignite their interest and commitment to research right from the outset of their academic journey to combat the absence of research students [19,20,21,22,23,24,25]. Although our study revealed that students responded positively to encouragement from faculty members, there appears to be a significant shortage of mentors and advisors available to guide students through the research process. This shortage can largely be attributed to a lack of funds for research, which is a common challenge faced by mentors and faculty. Without adequate financial support, faculty members may find it difficult to dedicate time and resources to mentoring students, as they often struggle to secure funding for research projects themselves. This financial constraint limits their capacity to effectively guide students, contributing to the overall shortage of available mentors and advisors in the academic setting [19, 27,28,29, 33,34,35]. One approach to encouraging faculty to support students in conducting research is to not only provide verbal encouragement but also to offer tangible incentives to those who conduct research and mentor students. By recognizing and rewarding the efforts of faculty members who invest their time and expertise in guiding students, we can create a more supportive environment for research activities. This could help address the current gap in mentorship and ultimately lead to an increase in student participation in research.
This study highlighted the urgent need for stakeholders and educational authorities to reform and revise the medical curriculum to encourage greater student involvement in research. To develop future physicians who practice evidence-based medicine, it is recommended that research methods be introduced early in the curriculum, starting from the first academic phase. This approach allows students to progressively develop their research skills rather than trying to cover research methodology and biostatistics in a rushed, single module. Implementing comprehensive and mandatory research courses throughout the program would promote deeper understanding and continuous learning. Moreover, providing diverse research training opportunities such as workshops, internships, and placements, both locally and internationally, will enhance students’ practical research abilities. Addressing the shortage of mentors through incentives and improving research infrastructure are crucial steps to effectively guide students and encourage active participation in research activities. Furthermore, random and covert inspections, along with surprise visits by medical education governing bodies such as the Bangladesh Medical and Dental Council (BMDC) and the Ministry of Health and Family Welfare (MoHFW), are recommended. These inspections assess the teaching environment in medical colleges, ensuring adherence to standards and identifying areas for improvement to ensure that research skills are effectively integrated into the medical curriculum and that policies are aligned with current needs and standards. Medical colleges can host career fairs where international and national NGOs and research organizations are invited. These events could serve to educate students about career opportunities in research-related fields and encourage them to consider pursuing careers in research.
Our study identified a significant disparity between medical students’ interest in research and their actual participation during their undergraduate years in Bangladesh. Reforming the medical curriculum to integrate early research methods, ensuring continuous learning throughout the academic phases, and providing diverse research training opportunities are therefore crucial.
This study was limited to cross-sectional observation, and respondents were not able to express their opinions in depth. Moreover, the online data collection method may have led to some data duplication, despite our efforts to eliminate this by rechecking entries and removing individuals with the same email address or medical college. Since only face validity was conducted on the questionnaire, there’s a possibility of less accurate responses, which could affect the interpretation of the findings. Additionally, we used a convenience sampling method, which might introduce some selection bias and restrict the generalizability of our findings to medical students from various institutions and regions across Bangladesh. However, a significant strength of our study is that we included at least one medical college from each division in Bangladesh to help reduce the potential selection and geographical biases associated with convenience sampling.
The datasets used in the study will be available from the corresponding authors on reasonable request.
The authors would like to express their sincere gratitude to Pi Research & Development Centre (www.pirdc.org) for their support and assistance for this study particularly in manuscript revision and formatting.
The authors have no support or funding to report.
The study was approved by the Ethical Review Committee of Public Health Foundation Bangladesh. Informed written consent was obtained from all eligible participants who agreed to participate. The authors declare that no human subjects were harmed, and the procedures followed were in accordance with the ethical standards and regulations established by the Helsinki Declaration of the World Medical Association.
Chat-GPT 3 was used to improve the clarity of the manuscript and for language editing.
Not applicable.
The authors declare no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Hasan, M.J., Islam, S., Sujon, H. et al. Research involvement among undergraduate medical students in Bangladesh: a multicenter cross-sectional study. BMC Med Educ 25, 126 (2025). https://doi.org/10.1186/s12909-024-06566-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-024-06566-w