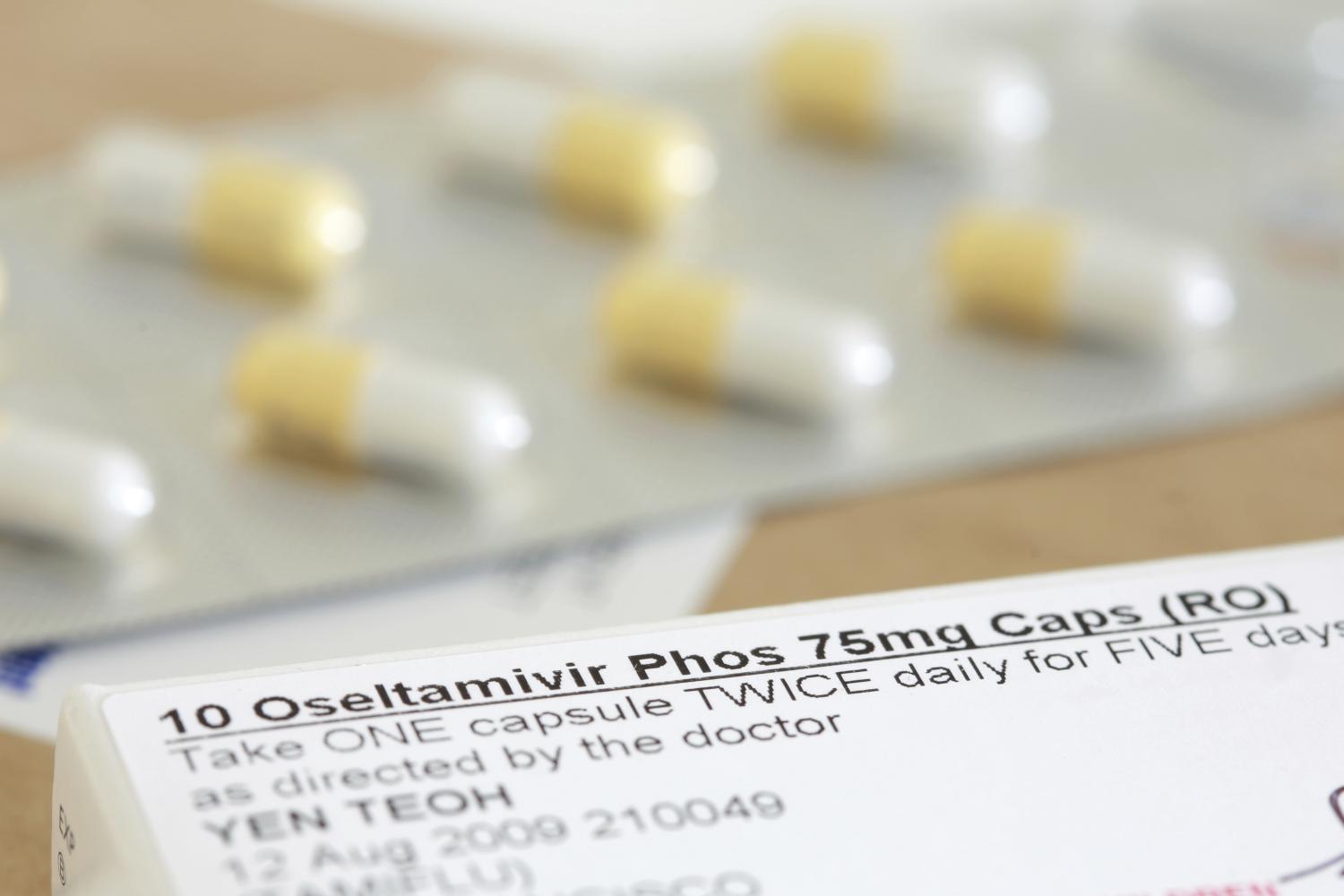
A new survey of pediatricians shows less than half adhere to national recommendations for oseltamivir (Tamiflu) prescribing for children hospitalized with flu, and suggests randomized control trials of the antiviral drug in the pediatric population would help increase uptake.
The study was published late last week in Pediatrics, and is based on survey results from 787 physicians from five specialties working at seven US children's hospitals from March to June 2024.
All US children hospitalized for influenza are recommended, per the American Academy of Pediatrics (AAP), to receive oseltamivir during their hospital stay, but inpatient use of the drug is inconsistent the authors said.
In the survey, clinicians were presented with four case description of patients and asked how likely they were to prescribe oseltamivir. All four case descriptions would meet the recommendations for oseltamivir use under current guidelines.
Overall, oseltamivir was recommended less than half the time (49.5%). Among clinicians with knowledge of guidelines, 62.0% recommended use, compared with 42.4% of clinicians who did not have accurate knowledge of guidelines.
Clinicians were less likely to prescribe the drug to patients with long illnesses or non-respiratory symptoms. Infectious disease specialists were most likely to recommend oseltamivir, while hospitalists were least likely to.
Most respondents (87.4%) believed a randomized trial of oseltamivir in hospitalized children was moderately to extremely important,
"Most respondents (87.4%) believed a randomized trial of oseltamivir in hospitalized children was moderately to extremely important," the authors concluded. They wrote that hospital length of stay was the most pressing primary outcome to assess.

A study at a Minnesota healthcare system finds that limiting the use of the antiviral drug remdesivir (Veklury) in hospitalized COVID-19 patients didn't result in a greater risk of death.
"There is limited data to support routine remdesivir use in the contemporary era of SARS-CoV-2 with widespread seropositivity [evidence of previous infection or vaccination]," the HealthPartners researchers wrote.
The team compared COVID-19 patients' 14-day risk of death 12 months before and after implementation of remdesivir restrictions at the system's eight hospitals (June 2022 to May 2023 and July 2023 to June 2024, respectively). Of the 4,774 patients with healthy immune systems included in the analysis, 3,323 and 1,451 participated before and after the intervention, respectively.
The findings were published late last week in Clinical Infectious Diseases.
Significantly fewer patients in the post-implementation group were given remdesivir (37.7% pre-intervention vs 4.1% post-intervention). Models of medium-risk covariates found no difference in 14-day all-cause death rates between the two groups (odds ratio, 1.8; 95% confidence interval, 0.54 to 5.8) or in 28-day all-cause death rates, 30-day readmissions, or length of hospital stay.
Remdesivir use was associated with an unexpected increased risk of ICU admission and MV within the post-intervention group only, which is likely explained by the higher-risk patient population that received remdesivir.
But remdesivir use was linked to a lower risk of intensive care unit (ICU) admission and need for mechanical ventilation (MV) before the intervention and a higher risk of these outcomes after.
"Remdesivir use was associated with an unexpected increased risk of ICU admission and MV within the post-intervention group only, which is likely explained by the higher-risk patient population that received remdesivir," the study authors wrote. "Prospective studies would be needed to definitively determine if highly vaccinated, immunocompetent patients benefit from remdesivir."
.jpg)
A coalition of food safety, public health, and consumer advocacy groups are urging Department of Health and Human Services Secretary Robert F. Kennedy Jr. to curb the use of antibiotics in the meat industry.
In a letter sent last week, the Food Animal Concerns Trust and 36 other organizations called on Kennedy to take four actions to reduce the amount of medically important antibiotics used by US farmers for food-animal production, which accounts for nearly two thirds of all medically important antibiotics sold in the United States. The groups have been warning for several years that widespread use of these antibiotics—which are also used in human medicine—in cows, pigs, and poultry is accelerating the antibiotic-resistance threat.
"The spread of superbugs, and the threat it represents, cannot be slowed without curbing the overuse of antibiotics," they wrote.
The groups note that while sales of antibiotics for human medicine have declined in recent years with better antibiotic stewardship, US sales for animal use rose by more than 10% from 2017 to 2023. They contrast that with Europe, where use of antibiotics in food-animal production has steadily declined since 2010.
The letter calls on Kennedy to prohibit the use of medically important antibiotics to prevent disease in food-animals in the absence of a diagnosed illness, a use that stewardship advocates have long argued is inappropriate and driven by unhealthy conditions on industrial farms. It also urges him to set national targets for reducing antibiotic use both in agriculture and human medicine, finalize guidance that limits durations of antibiotic use in food animals, and create a national monitoring system to track antibiotic use in food-animal production.
"As Secretary, you have the opportunity using existing authorities to make our food system much safer by implementing these steps to stop the overuse of antibiotics by the meat industry that is leading to the spread of deadly antibiotic-resistant pathogens," the letter states.

A summary of chronic wasting disease (CWD) sampling results from the 2024 Wisconsin deer-hunting seasons reveals that 10% of the state's deer had the fatal neurologic disease.
In a news release today, the Wisconsin Department of Natural Resources (DNR) said that 89% of the positive cases were found in the Southern Farmland Zone, which had 21% positivity (1,583 of 7,680). The Southern Farmland Zone includes counties close to the border with Illinois and Iowa.
Of the 17,399 deer sampled throughout the state, 1,786 (10.3%) tested positive for CWD.
The 2024 efforts focused on sample collection in areas near recent wild and/or captive CWD-positive cases, primarily in central and northern Wisconsin. Two counties in these areas, Pierce and Menominee, had first-time detections in wild deer.
Outside of the priority sampling and endemic areas, Chippewa and Manitowoc saw their first positive detections in wild deer.
"Although we have detected CWD in new areas of the state in recent years, many of these areas are at a low prevalence rate, and opportunities still remain to slow the spread and growth of the disease statewide," Erin Larson, DNR deer herd health specialist, said in the release.
The 242 sampling locations included 166 self-sampling kiosks and 76 staffed sites, and the 154 carcass-disposal sites included dumpsters, landfills, and transfer stations. The average time from sample drop-off to hunter result notification was 8.4 days.












