BMC Geriatrics volume 25, Article number: 447 (2025) Cite this article
Population ageing is a global phenomenon that resulted from the demographic transition. Senescence leads to increasing dependency on carrying out Activities of Daily Living (ADL). Limitations in ADL impact not only the individual but also the society through higher demand for social and health care services. Thus, this study aims to describe the prevalence of ADL limitation and determine factors associated with transition from independence to ADL limitation among community-dwelling older adults in Malaysia.
A prospective cohort study using data from 2275 adults aged 60 and above from the Malaysia Ageing and Retirement Survey, was conducted. Respondents were categorised into independent and with ADL limitation, defined as the inability to carry out at least one ADL item, measured using items adapted from the Barthel’s index. Those who were independent at baseline were followed up three years later to determine their ADL limitation status. Logistic regression analysis was conducted to assess whether sociodemographic and health factors such as age, sex, education attainment, multimorbidity, cognition, level of physical activity, health status, and body mass index (BMI) predicted the transition from independence to ADL limitation.
The baseline prevalence of ADL limitation was 15.7%. Among those who were independent at baseline, 8.2% developed ADL limitation at follow-up. Increasing age, female sex, poor health status, lower levels of physical activity, and abnormal BMI were predictors of transition from independence to ADL limitation at follow-up (AUC = 0.83).
The prevalence of ADL limitation among community-dwelling older adults in Malaysia was comparable to the other reported figures. Lower levels of physical activity and abnormal BMI were two modifiable predictors of transition to ADL limitation among independent older adults. As such, policy strategies to further enhance active lifestyles and maintain normal BMI levels, especially among independent older adults, should be explored.
Economic and technological advancements have led to the demographic transition observed today, with improved living conditions allowing individuals to live longer. Globally, the average life expectancy is 73 years, ranging from 58 years in Lesotho to 84 years in Japan [1]. Given the longer lifespan and the epidemiologic transition that follows, there is increasing demand for maintaining well-being among the aged population. Malaysia is not spared from this global phenomenon, where it is postulated that it will become an aged society by 2044 [2], with the life expectancy at birth of 75 years [3]. Accelerated population ageing creates continual challenges for maintaining good health.
The functional capacity of older adults is measured by the ability to carry out basic activities of daily living (ADL). Many studies have been conducted to assess the level of limitation in carrying out ADL among older adults, with various indices used to measure the level of functional capacity [4]. Using the Barthel’s Index, a meta-analysis of studies from the Association of Southeast Asian Nations (ASEAN) region reported that 21.5% of those aged 60 and above had functional limitation [5]. In 2018, 17% of Malaysians aged 60 and more reported having functional limitations, with observed gender and socioeconomic disparities [6]. This prevalence is expected to increase by more than 50% between 2020 and 2040 [2]. Compared to those without functional limitations, those with functional limitations have higher lifetime healthcare spending in terms of hospitalisation [7]. Moreover, a 30-year projection of long-term care costs among the Chinese older adults found an 8-fold increase in per capita healthcare cost between 2020 and 2050 [8].
As functional capacity is dynamic, some studies have attempted to describe the transitions between levels of ADL limitation. ADL changes among community-dwelling older adults are complex, as the population is skewed towards those who are free from ADL limitation, displaying a lesser degree of functional decline in comparison. Among sixty-year-old or older Mexicans without ADL limitation, 10.6% developed mild limitation at follow-up 11 years later [9]. Elsheemy reported more improvement than deterioration across five waves of the English Longitudinal Study of Ageing (ELSA) for those with at least one ADL limitation at baseline [10].
Comparison across six middle-income countries found varied determinants of ADL limitation [11]. Associations have been found between social factors such as gender [9, 12,13,14,15], education [9, 12, 15, 16] living arrangement [12, 13]); and health factors included presence of chronic diseases [11, 12, 14, 16,17,18,19], self-perceived health [15], BMI [12], physical activity [12], depression [11, 12, 18, 20], cognitive impairment [14, 18] and functional limitation. Evidence investigating cross-country comparisons in factors associated with ADL limitation found varying determinants between countries, suggesting that country-specific contextual factors may have an influence on the ADL limitation level of older adults.
While some level of functional decline is expected with increasing age, it is vital to preserve as many functional capacities as possible to maintain quality of life and well-being. Additionally, after controlling for age, gender, socioeconomic status, social participation, and social support, older adults with functional limitations have 1.07 times higher care needs compared to those without [21]. A local study in a high-income Malaysian state found that older adults with mild ADL limitation were five times more likely to require assistance than independent older adults [22]. Care for older adults often falls on family members, particularly in Asian communities where culture revolves around filial duty. However, rapid changes in the economic scene, movement away from multigenerational households, and increasing participation in the labour market put a burden on family caregivers, both physically, mentally, and financially [23].
A study has modelled the transition probability of older adults in Malaysia [24], and several investigations have been conducted to explore the factors associated with functional limitations in older adults [20, 22, 25, 26]. However, to the best of our knowledge, the transition of ADL over time and determinants of transition from independence to ADL limitation among a nationally-representative cohort in Malaysia have not been investigated. Moreover, identifying determinants of transition to ADL limitation allows targeted policies to provide better care for older adults in Malaysia. Therefore, this study aims to describe the prevalence of ADL limitation (measured using the inability to carry out any ADL item independently), ADL transition at 3-year follow up and determine factors associated with the transition from independence to ADL limitation among community-dwelling older adults in Malaysia.
The Malaysia Ageing and Retirement Survey (MARS) is a prospective cohort study among individuals aged 40 and above. A two-stage cluster sampling method was employed based on the 2010 Population and Housing Census from the Department of Statistics, Malaysia (DoSM). Each state was stratified according to urban/rural strata. The DoSM systematically sampled 900 out of the existing 75,000 enumeration blocks (EB), followed by a random selection of 10–12 households per EB using a computer-generated list. From the 900 EBs, 9542 households were approached. The three oldest eligible members were identified as possible respondents. Respondents answer a questionnaire that covers six sections: (i) background information, (ii) family support and transfer, (iii) health, (iv) work, employment and retirement, (v) income and expenditure, and (vi) savings and assets, designed to be comparable to other ageing longitudinal studies, through Computer Assisted Personal Interviewing (CAPI) [27]. Information regarding the questionnaire is provided in the survey description published elsewhere [28], and the MARS reports [27, 29]. The questionnaire used for each wave is available for download on the MARS website [30].
To date, two waves of MARS have been completed, where Wave 1 data collection was from August 2018 to May 2019, and Wave 2 was from October 2020 to April 2022 (prolonged due to the COVID-19 pandemic). A total of 5,613 respondents completed the survey in Wave 1, with an overall response rate of 84% [27]; while 4821 respondents completed the survey in Wave 2 (2842 out of 4497 sampled households, where 75% were panel respondents [29]. Attrition was due to loss to follow-up and death. Information on death was obtained from the Registration Department on 30 June 2022. Detailed information on MARS is described elsewhere [28], and descriptive findings have previously been published [27, 29].
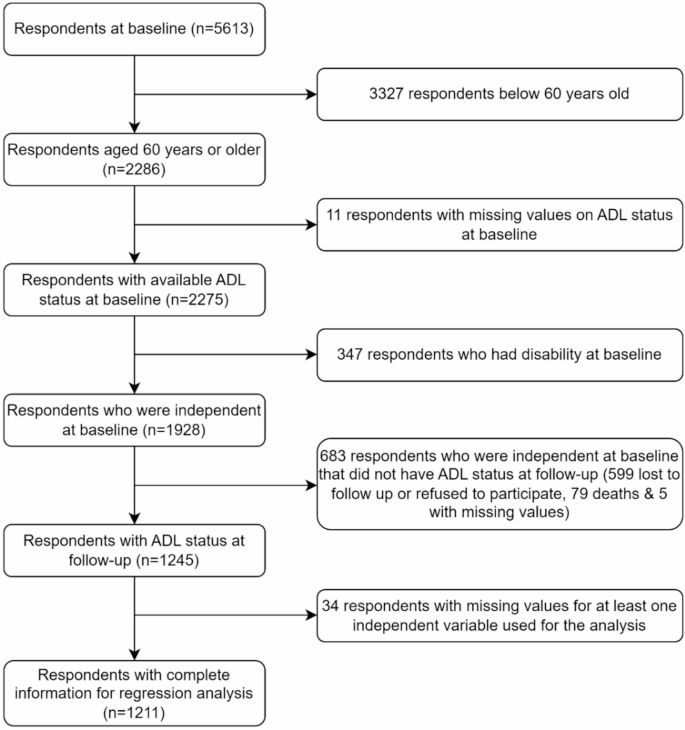
Of the total survey respondents at Wave 1 (baseline), 2286 were aged 60 and above. Figure 1 presents the flow diagram of respondents. Those without baseline data on ability to carry out ADL (n = 11) were excluded. ADL transition between baseline and follow-up was described among 2275 participants. Those with ADL status at baseline and follow-up, were independent at baseline with complete information on all variables (n = 1211) were included in the investigation on determinants of transition from independence to ADL limitation.
A common measurement tool for ADL is the Barthel’s index [31]. MARS is part of the Gateway to Global Ageing Data which aims to facilitate inter-country comparisons through harmonised data [32]. The questionnaire used was developed in consultation with content experts from the Japanese Study of Ageing and Retirement (JSTAR) and Survey of Health, Ageing and Retirement in Europe (SHARE) [27, 28]. Survey items were reviewed for integration into the local context. In MARS, ADL limitation was measured using nine items: bathing, dressing, grooming, mouth care, toileting, transferring to bed/chair, walking around the house, climbing stairs and eating. Mouth care was added while incontinence was excluded, in contrast to the original Barthel’s index. A study validating functional ability measurement in Malaysia found that incontinence was infrequent [33], while a national survey among older adults reported low prevalence of incontinence [34], supporting the omission of the item in the MARS survey. Mouth care is instrumental in maintaining oral health, a prevalent health issue in Malaysia [35]. Washing teeth is one of the items measuring functional ability in The Korean Longitudinal Study of Aging (KLoSA) [36]. Respondents for MARS opt to answer either: (i) able to do it all by myself; (ii) sometimes need some help; (iii) always need some help; and (iv) always need help to each ADL item [37]. The last three responses indicate inability to carry out the activity. The adapted questionnaire was pilot tested prior to data collection [27].
In the descriptive analysis, we categorised ADL limitation into six categories, (i) independent (able to carry out all ADL items without help), (ii) 1–2 ADL limitations, (iii) 3 or more ADL limitations, (iv) deceased, and (v) lost to follow-up or refused to participate, and (vi) missing. To further explore the predictors of transition from independence to ADL transition through a logistic regression model, those with inability to carry out any ADL item at follow-up (Wave 2) were aggregated into one category, has ADL limitation, coded as [1]; and independent, able to carry out all ADL items without help, coded as (0). Although a nuanced approach by looking at different levels of ADL limitations as the outcome would provide richer information, the data does not support a good model fit due to the small number of observations in some groups [38].
The independent variables were selected based on evidence from existing literature [9, 11, 12, 14,15,16,17,18, 39, 40]. They were measured across waves to assess their impact on follow-up outcomes. The independent variables encompass sociodemographic (age, sex, and highest education attainment), health status (multimorbidity, self-rated health, and cognitive index) as well as health risk factor variables (physical inactivity and BMI).
Age was treated as a continuous variable. Sex was coded into male (0) and female [1]. Responses for highest education attainment were re-categorised into three groups, (i) no formal education (no schooling, kindergarten/nursery, and religious school), (ii) primary, and (iii) secondary/tertiary (lower secondary, upper secondary, vocational/technical, pre-university/diploma/form 6, first degree, and postgraduate).
Respondents were asked if they had a list of doctor-diagnosed illnesses (Additional file 1). Those who answered yes to any illness in the list were coded as 1, and the total number of doctor-diagnosed illnesses was calculated. Multimorbidity, defined as the existence of two or more doctor-diagnosed illnesses [41], was dichotomised into yes [1] or no (0). Self-rated health was operationalised through the question “Which of the following best describes your current health status?”. Respondents chose their answer from a five-point Likert scale: “Very good / good / moderate / poor / very poor”. Responses for self-rated health were re-categorised into good (very good / good), fair, and poor (poor / very poor). To assess cognitive function, MARS adopted a similar measure to HRS, a nationwide longitudinal study in the United States, which includes seven tests: (i) 10-word immediate recall; (ii) delayed recall; (iii) serial 7s subtraction; (iv) counting backward; (v) object naming; (vi) date recall, and; (vii) Prime Minister naming [42]. The maximum possible score for each test is 100. The cognitive index is derived by calculating a composite by averaging the scores for all the tests.
Health risk factors included in the analysis are BMI and physical inactivity. Respondents’ BMI was calculated as weight in kilogrammes divided by height in metres squared, categorised into underweight, normal weight, overweight and obese, based on the World Health Organization (WHO) classification for Asian populations [43]. Physical activity was assessed by asking the frequency of taking part in vigorous, moderately vigorous and light exercises/activities, with five possible responses: (i) every day; (ii) more than once a week; (iii) once a week; (iv) one to three times a month, and; (v) rarely/never. These questions were developed to enable global harmonisation variables across longitudinal surveys in the older population, Health and Retirement Study (HRS), English Longitudinal Study of Ageing (ELSA) and Survey of Health, Ageing and Retirement Europe (SHARE). These responses were further categorised into four groups, as previously defined in other studies using similar measures for physical activity among older adults [44, 45], namely: (i) inactive (no activity in a week); (ii) only light activity at least once a week; (iii) moderate activity at least once a week but no vigorous activity), and; (iv) vigorous activity at least once a week. The categorisation of physical activity was chosen based on its consistent use in the analysis of data from the ELSA [46,47,48].
The data were analysed using STATA software version 16 [49]. First, we used counts and proportions to describe the prevalence of ADL limitation at baseline (Wave 1) and ADL transition at follow-up. Next, we focused our investigation on respondents who were independent at baseline who were alive at follow-up. Descriptive statistics based on the ADL limitation status at follow-up were reported. Differences between groups were assessed using chi-square test and Analysis of Variance (ANOVA).
We used a logistic regression model to investigate the effects of predictors at baseline on transition from independence to ADL limitation at 3-year follow up. The analysis was carried out using the enter method, where all predictors were entered into the model simultaneously to assess their individual contributions. We conducted a complete case analysis, supported by Little’s test indicating that data were missing completely at random [50]. Multicollinearity was evaluated using the Variance Inflation Factor (VIF) [39], and model goodness-of-fit was assessed through the Archer-Lemeshow test [51]. To evaluate the predictive performance of the final model, we used classification tables and the area under the ROC curve (AUC). All analyses applied survey weights to account for the complex sampling design.
Due to the high missingness of data in the analytic sample for logistic regression, sensitivity analysis using imputed datasets were carried out. Missing data were handled using multiple imputation by chained equations using STATA (version 16) [52]. Variables with incomplete data (ADL limitation status at follow-up, cognitive index score, multimorbidity, self-rated health and BMI category) were imputed with fully observed variables and complex survey design variables as predictors in the imputation models. Imputation diagnostics, available in Additional file 2, were inspected using the “midiagplots” command [53]. All models included the same set of covariates to inform the imputation process. Ten imputed datasets were created with a fixed random seed. Imputed datasets were subsequently used for the logistic regression model, where estimates were combined across the imputed sets using Rubin’s Rules. Predictors of transition to ADL limitation remained the same except for BMI category where the magnitude and strength of association between underweight BMI and ADL limitation was attenuated in the imputed model (Additional file 3). This suggests that the regression model using complete case analysis may have overestimated the association.
Overall, 2275 adults aged 60 and older, representing 3.36 million older adults in Malaysia were included. The population characteristics are presented in Table 1. At baseline, 84.3% (95%CI 82.0-86.4) of older adults were independent, and 15.7% (95%CI 13.6–18.0) had at least one ADL limitation. The demographic characteristics of the respondents and the available characteristics of the general population aged 60 and above showed comparable proportions (Additional file 4).
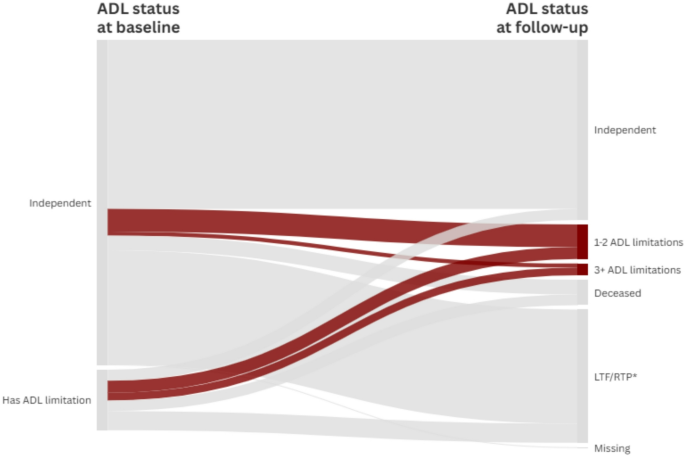
The ADL status at follow-up was unknown for 30.7% (n = 700) of the study population, who either refused to participate or were lost to follow-up. The characteristics of these respondents are available in the supplementary table (Additional file 5). There were no significant differences between the characteristics of known and unknown ADL status respondents at follow-up. Figure 2 provides a visualisation of the ADL transition among older adults aged 60 and above in Malaysia. A notable proportion (52.0%) of those who were independent at baseline maintained their independence. Those with existing ADL limitations at baseline mostly remained at the same level (1–2 ADL limitations: 15.0%, 3 or more ADL limitations: 25.6%). Additional file 6 compares the transition to ADL limitation between complete case dataset and multiple imputation datasets. Death was higher among those with ADL limitation at baseline (1–2 ADL limitations: 15.0%, 3 or more ADL limitations: 25.6%). Additional file 6 compares the transition to ADL limitation between complete case dataset and multiple imputation datasets.
ADL transition between baseline (Wave 1) and follow-up (Wave 2). Created with flourish.studio. *LTF/RTP: Lost to follow-up or refused to participate in the follow-up survey. ADL: Activities of Daily Living
Among independent respondents at baseline, 1211 had complete data for the investigation. Table 2 presents their characteristics. The mean age of older adults in the ADL limitation group was higher compared to the independent group (71 years old versus 67 years old). There were sex differences in the proportion of ADL limitation at follow-up, with a higher proportion seen among females (19.1%, 95%CI:15.1–23.9). ADL limitation at follow-up was more prevalent among those who had no formal schooling (23.2%, 95%CI:15.2–23.9), had poor self-rated health (30.2%, 95%CI:20.1–42.8), did only light activities at least once a week (21.3%, 95%CI:15.5–28.6), and were underweight (25.6%, 95%CI:14.0–42.0).
In the univariate analysis (Table 3), increasing age, female sex, presence of multimorbidity, lower level of physical activity, poor self-rated health, and abnormal BMI increased the likelihood of having ADL limitation at follow-up. At the same time, higher education attainment and higher cognitive index scores were protective against transition to ADL limitation.
Holding other variables constant, increasing age was associated with a higher likelihood of transition to ADL limitation at follow-up (aOR:1.12, 95%CI:1.08–1.16). Additionally, female sex (aOR:2.99, 95%CI:1.82–4.91), lower level of physical activity (inactive versus vigorous activities at least once a week aOR:1.98, 95%CI:1.03–3.81; only light activities versus vigorous activities at least once a week aOR:2.07, 95%CI:1.10–3.88), being underweight (aOR:4.20, 95%CI:1.65–10.69) and obese (aOR:3.06, 95%CI:1.56-6.00), and poor self-rated health (aOR:3.33, 95%CI:1.71–6.50) increased the likelihood of transition to ADL limitation. The protective effect of increasing cognitive function on the transition to ADL limitation was no longer significant after adjusting for age, sex, education, presence of multimorbidity, level of physical activity, health status, and BMI.
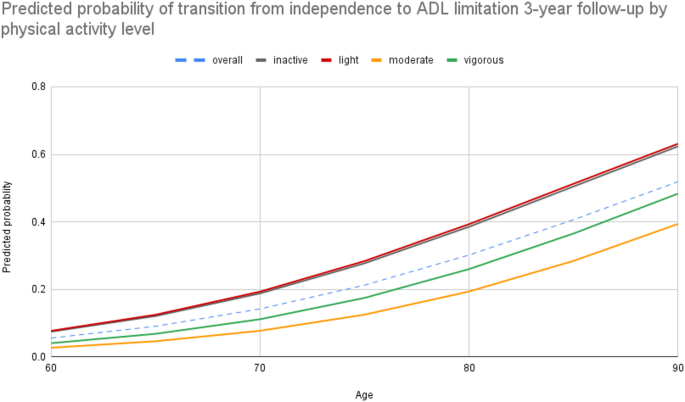
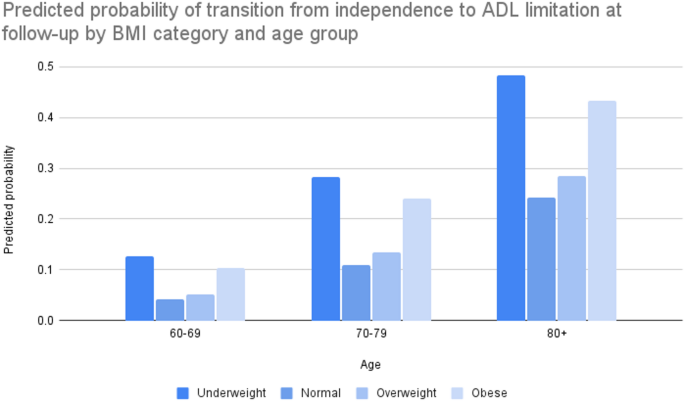
The probability of having at least one ADL limitation at follow-up increased at a faster rate beyond the age of 70 (Fig. 3). Older adults engaging in moderate physical activity had the lowest probability of transitioning to ADL limitation, and the rate of increase with age was slower. Figure 4 demonstrates the U-shaped predicted probability of transitioning to ADL limitation by BMI category, which remained consistent across age groups.
Predicted probability of transitioning to ADL limitation with increasing age, by physical activity level
This study found that most older adults in a community-dwelling cohort were independent. The investigation revealed that a small proportion developed ADL limitation after three years. Despite having 1–2 ADL limitations at baseline, some older adults improved in their ability to carry out ADLs, suggesting the possibility of improvement in their physical functioning. Among those who were independent at baseline, age, sex, health status, level of physical activity, and BMI were determinants of the transition to ADL limitation at follow-up.
The prevalence of ADL limitation in adults aged 60 and above ranged between 13.6 and 18.0%, in keeping with the figure reported in the National Health and Morbidity Survey (NHMS) 2018 (17%) [6]. In contrast, the range of ADL limitation prevalence across several ASEAN countries was 16.2–27.3% [5]. Compared to other surveys among the older population, the prevalence found in this study seems to be consistent with its few other health and retirement sister studies globally, including the SHARE in Europe (13.8%) [54]; and is higher compared to the Mexican Health and Aging Study (12.7%) [9]. Apart from China, data from the Study on Global AGEing and Adult Health (SAGE) found a much higher prevalence of ADL limitation among older adults in Ghana, India, Mexico, Russia, and South Africa, ranging between 38.6 and 55.7% [11]. However, each survey measured ADL using various tools, making a direct comparison of nationally representative ADL limitation prevalence challenging.
Further investigation into transition to ADL limitation among adults aged 60 and above showed that half of those who were independent at baseline maintained independence. In contrast, 40.3% of the Mexican older population [9] and 64.3% of the older Chinese population [40] maintained independence. The levels of deterioration among those independent at baseline in this investigation are lower compared to those reported in the Mexican cohort (8.18% versus 13.9% developed ADL limitation, and 4.54% versus 35.8% died). One possible reason is the much more extended follow-up period for the Mexican cohort, where the youngest in the cohort would have approached the life expectancy at birth at the end of the follow-up period [55]. Despite having the same follow-up period of 3 years as this study, findings from the Chinese Longitudinal Health Longevity Study (CLHLS) uncovered similar proportions to that reported for Mexico (12.1% developed ADL limitation and 23.7% died). However, the sample selection method for CLHLS might have implicated the results as the original cohort started with a much older cohort of 100 years and above, with the addition of respondents from wave three onwards.
The predictors of transition to ADL limitation found in this study agree with those previously described in the literature. Similar to findings from longitudinal surveys among older adults in Mexico [9] and Europe [15]; as well as cross-sectional studies in India, Korea, China, and Ghana, females had a higher risk of ADL limitation compared to men [11, 12, 14]. The sex differences observed could possibly be explained by the higher proportion of females who were underweight and obese in the study population, similar to reported sex differences in obesity among the older adult population in the NHMS survey [56]. Older adults with perceived poor health compared to good health in our investigation were more likely to transition to ADL limitation at follow-up. This result corroborates the finding that perceived better health was protective of transition to ADL limitation among the older population in Europe [15]. Furthermore, baseline self-rated health was found to be a strong predictor of transition to ADL limitation, where the risk increases with decreasing health in a 10-year prospective cohort study among Japanese adults aged 65 and above Our finding that cognitive function was not significantly associated with the transition ADL limitation after adjustment contrasts with previous studies [14, 18]. A possible reason for this difference is the influence of confounding variables. Earlier research may not have fully accounted for factors such as physical activity and BMI, which can affect both cognition and ADL limitation. In our study, we adjusted for a broader set of covariates including age, sex, education, multimorbidity, subjective health status, physical activity, and BMI which may have reduced the observed effect. Similarly, our findings differed from previous evidence that multimorbidity increases the risk of developing ADL limitation [11, 12, 14, 16,17,18,19]. The association between multimorbidity and ADL limitation may have been overestimated in prior studies that did not adjust for cognitive status or subjective health. By including these and other covariates in our models, the association was attenuated, suggesting that earlier findings might reflect residual confounding rather than a direct causal relationship. Future studies should consider using causal modelling approaches to better explore these complex relationships and assess whether these associations reflect direct effects or are mediated by other factors.
Findings from this study point towards a higher risk of transitioning to ADL limitation among those who were physically inactive and low levels of physical activity; however, as the data lacked the duration of physical activities based on various intensities, the investigation was not able to operationalise physical inactivity based on non-compliance to current guidelines for physical activity among older adults [57]. As physical inactivity in the older population can be measured in various ways [58], we used the definition of physical activity employed by Smith (2015), whose study utilised data from ELSA, which measures physical activity using similar questions to the MARS survey. A national cross-sectional study in Malaysia that defines physical inactivity using the WHO guidelines found that the risk of ADL limitation was 1.94 times higher in those who were physically inactive compared to those who were active [59]. A more recent study found increasing physical activity resulted in physical function improvements among older adults with ADL limitations [60]. As such, interventions aimed at maintaining an active lifestyle to promote healthy ageing have the combined benefit of possibly reducing social care demand and maintaining well-being. Malaysia puts integrated programmes for life-course health promotion at the forefront of the strategies listed in the National Health Policy for Older Persons [61]. In 2021, a 10-year national agenda for wellness (Agenda National Malaysia Sihat) was launched to improve health and well-being in Malaysia [62]. On top of strengthening health promotion, three new wellness services were introduced, namely the Wellness Hub, the I Fit and Eat Right (IFitEr) Intervention, and Wellness on Wheels (WoW). Among others, these services aimed to reduce the prevalence of physical inactivity among the population.
Another significant modifiable predictor of transition to ADL limitation in the study is BMI. Similar U-shaped associations have been reported in other cohorts in Japan, where those who were underweight have the highest magnitude of ADL limitation risk, followed by those who were obese [63, 64]. In contrast, being obese was a protective factor for developing ADL limitation among Chinese octogenarians [65], suggesting interventions should be tailored to age categories among the aged population to achieve different targets. The association between being underweight and poor health outcomes has been well-established; however, the association between obesity and poor health outcomes remains inconsistent [66]. Despite this, maintaining a healthy BMI among the older population should be a focus of health ageing policies to ensure that they can live independently and have a good quality of life. Further, lifestyle changes for maintaining a healthy BMI are the mainstay of management of chronic diseases that are more prevalent at older age. The National Plan of Action for Nutrition in Malaysia III (2016–2025) has age-specific indicators, where targets were set in monitoring the prevalence of overweight and obesity among those aged 60 and older [67]. One of the strategies to achieve this was the development of materials specifically targeting the older population. In 2023, the second edition of the Clinical Practice Guidelines for the Management of Obesity was released, providing comprehensive management across the life course [68].
The model that was built to predict determinants of transition from independence to ADL limitation had AUC of 0.83 which indicates that the model has excellent discriminatory ability in distinguishing between individuals with and without ADL limitation [69]. This suggests that the model could be used as a screening tool, particularly in community or primary care settings where early identification of at-risk individuals has the potential to improve population outcomes. In Malaysia, the Health Status Screening Form for Older Adults (Borang Saringan Status Kesihatan Warga Emas) is widely used in the primary care setting, where it collects information similar to the variables used in the model [70]. As such, those who are ADL independent with risk factors of transitioning to ADL limitation can be identified for early intervention of the modifiable risk factors.
While the strength of this study lies in the use of nationally representative longitudinal survey data, it is not without its limitations. The survey was only recently initiated, hence only data from two waves were available. Moreover, data collection for the second time-point was during the COVID-19 pandemic, which may have resulted in the high proportion of loss to follow-up observed. Sensitivity analysis using imputed data showed similar predictors except for one BMI category, suggesting potential bias due to attrition and limited generalisability of the estimates from the complete case analysis, particularly if the data is not missing at random. The use of self-reported measures introduces bias. Further, the results on ADL limitation may be underestimated as the survey did not include institutionalised older adults. Specifically for physical activity, the available data lacked the duration of carrying out activities by various intensities, which did not allow for the more appropriate measurement of physical activity against the guidelines recommended by WHO. The use of BMI as a predictor variable may not extensively reflect the nutritional status of older adults and does not account for muscle mass, which can influence functional capacity in older adults. Further studies should consider a more extended follow-up period to enable comparison with other cohorts, examine long-term changes in ADL limitation, and investigate the consistency of the current findings. Additionally, investigation into possible reversal of ADL limitation by increasing physical activity and maintaining a normal BMI can be explored. Nevertheless, evidence generated from this study adds to current knowledge from the perspective of a multicultural population in a non-Western society. The results from this study can guide implementation of sustainable and accessible community-based and home-supported interventions targeting the modifiable risk factors, which has the potential to improve the health outcomes and wellbeing of older adults by maintaining their ADL independence or improving their ADL status.
The prevalence of ADL limitation among community-dwelling older adults in Malaysia was comparable to the other reported figures. Investigation into ADL transitions confirm the possibility of improvement toward independence for a small percentage of older adults. Maintaining ADL independence is essential in preserving the overall well-being and quality of life of older adults while reducing healthcare costs for both individuals and health systems. As the study findings indicate the higher likelihood of transitioning to ADL limitation with lower physical activity levels, being underweight and obese, policy strategies to enhance active lifestyle and maintain normal BMI levels, especially among community-dwelling independent older adults, should be further explored.
The data that support the findings of this study are available from the Social Wellbeing Research Centre, Universiti Malaya but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the Social Wellbeing Research Centre and request can be made via https://swrc.um.edu.my/mars-data.
- ADL:
-
Activities of Daily Living
- ANOVA:
-
Analysis of Variance
- ASEAN:
-
Association of Southeast Asian Nations
- aOR:
-
Adjusted Odds Ratio
- AUC:
-
Area Under the ROC Curve
- BMI:
-
Body Mass Index
- CLHLS:
-
Chinese Longitudinal Health Longevity Study
- CI:
-
Confidence Interval
- DoSM:
-
Department of Statistics Malaysia
- EB:
-
Enumeration Blocks
- ELSA:
-
English Longitudinal Study of Ageing
- HRS:
-
Health and Retirement Survey
- IFitEr:
-
Wellness Hub, the I Fit and Eat Right
- JSTAR:
-
Japanese Study of Aging and Retirement
- KLoSA:
-
Korean Longitudinal Study of Aging
- MARS:
-
Malaysia Ageing and Retirement Survey
- NHMS:
-
National Health and Morbidity Survey
- OR:
-
Odds Ratio
- SAGE:
-
Study on Global AGEing and Adult Health
- SD:
-
Standard Deviation
- SHARE:
-
Survey of Health, Ageing and Retirement Europe
- VIF:
-
Variance Inflation Factor
- WHO:
-
World Health Organization
- WoW:
-
Wellness on Wheels
The authors would like to thank the Director-General of Health for permission to publish this paper. Our sincerest gratitude to the Malaysia Ageing and Retirement Survey research team for their hard work in collecting the data. We would like to thank Tan Lih Yoong for her assistance in providing further information related to the MARS datasets.
The Simulation of Long-term Care for Elderly in Malaysia (MyLTC) project was funded by the Ministry of Health (MOH) Research Grant (MRG). The MARS study was funded by the Old Age Financial Protection (OAFPC), now known as the Social Wellbeing Chair (SWC) of the Social Wellbeing Research Centre, Universiti Malaya, Asian Development Bank (ADB) and Social Security Organisation (SOCSO). The funders had no role in the conceptualisation, design, data collection, analysis, decision to publish or preparation of the manuscript.
This study is a secondary data analysis for the Simulation of Long-term Care for Elderly in Malaysia (MyLTC), approved by the Medical Research Ethics Committee (Malaysia) (Reference No: KKM/NIHSEC/P21-992(4)). The MARS survey was approved by the Universiti Malaya Research Ethics Committee (UMREC) (Reference No: UM.TNC2/UMREC–341). The study was conducted in accordance to the standards set forth of the Declaration of Helsinki. In MARS, both verbal and written informed consent were obtained from the respondents during fieldwork prior to the survey interview.
Not applicable.
The authors declare no competing interests.
Not applicable.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Below is the link to the electronic supplementary material.
Supplementary Material 1: Additional file 1. List of doctor-diagnosed illnesses asked in the survey. The list of diagnoses for respondents to choose from when asked about doctor-diagnosed illnesses. Additional file 2: Imputation diagnostics of multiple imputation dataset for logistic regression. Diagnostic plots of imputed values against observed values. Additional file 3: Predictors of transition from independence to ADL limitation at follow-up. Comparison between the multivariate logistic regression results of complete case dataset and multiple imputation dataset. Additional file 4: Comparison between study population and population data. Comparison of the study population characteristics with population data from the Department of Statistics Malaysia to confirm that the findings are representative of the general population. Additional file 5: Characteristics of respondents with unknown ADL at follow-up (Wave 2). Characteristics of the respondents that were removed from the analysis. There was no difference between the characteristics of the analysed population and the ones that were dropped for the regression analysis. Additional file 6: ADL transition between baseline (Wave 1) and three-year follow-up (wave 2). This file presents two tables – Table 1 presents the proportion and estimated population for the transition between ADL groups independent, 1–2 ADL limitation and 3 + ADL limitations using the observed dataset, while Table 2 presents the comparison of the ADL transition results between the observed dataset and multiple imputation dataset
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Md. Sharif, S., Jawahir, S., Fun, W.H. et al. Predictors of transition from independence to limitations in activities of daily living (ADL) among independent community-dwelling older adults: longitudinal evidence from the Malaysia ageing and retirement survey (MARS). BMC Geriatr 25, 447 (2025). https://doi.org/10.1186/s12877-025-06076-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-025-06076-4