Neurological Manifestations Of Long COVID: Fog, Fatigue And Forgotten Words
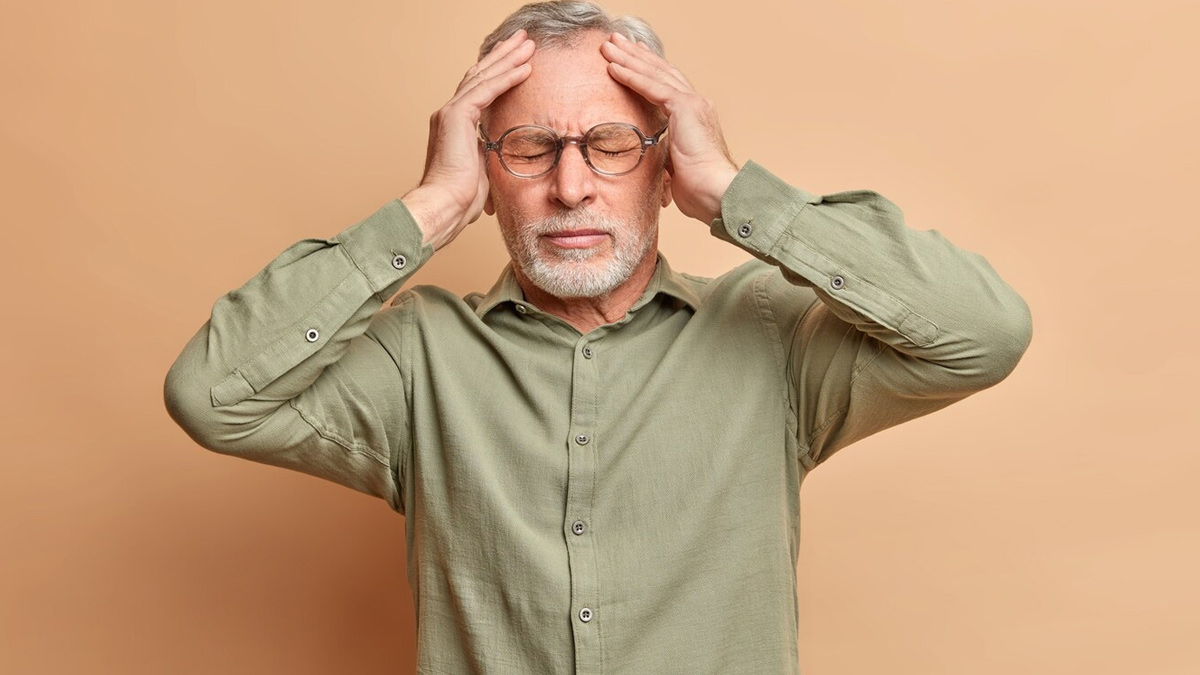
“One of the most reported symptoms is 'brain fog.' But that term doesn't do justice to the distress it causes. Many patients find themselves easily distracted or unable to focus. They might pause mid-sentence, forget familiar words, or feel overwhelmed by everyday decisions. Even simple routines, such as drafting a short email or keeping track of dates become unexpectedly difficult,” said Dr Umesh.
From a clinical standpoint, this cognitive dysfunction is measurable. Neuropsychological testing often shows deficits in attention, executive function, processing speed, and working memory. Brain imaging in some patients has even revealed subtle changes in structure and function, especially in areas, such as the frontal cortex and hippocampus, which are linked to memory and cognition.
Now, why does this mental fog happen in the first place? “We don’t have all the answers yet, but a few possibilities are emerging. One idea is that the body’s immune system, while fighting off the virus, may cause some lingering inflammation in the brain. It’s like the immune response gets stuck in a loop, even after the infection has cleared,” said Dr Umesh.
“There’s also the theory that tiny clots, far too small to show up on regular scans, might be disrupting blood flow in certain parts of the brain. And then there’s the question of viral remnants: some experts believe that bits of the virus might hang around in nerve tissues, quietly triggering symptoms even weeks or months later,” he added.
Unlike usual tiredness, post-COVID fatigue is deeply disabling. It doesn’t improve with rest, and it’s often worsened by physical or mental exertion, a phenomenon known as post-exertional malaise. Many patients say the fatigue comes in unpredictable waves, sometimes leaving them bedridden for days.
“This isn’t just physical exhaustion, it’s neurological. The brain itself may be struggling to regulate basic energy functions. Mitochondrial dysfunction, persistent low-grade inflammation, and dysregulation of the autonomic nervous system have all been suggested as possible contributors,” added Dr Umesh.
For neurologists, this fatigue echoes what is seen in conditions like Chronic Fatigue Syndrome (ME/CFS), which shares many features with long COVID. Some researchers believe that COVID-19 may act as a trigger for post-viral fatigue syndromes in predisposed individuals.
Another unsettling complaint from long COVID patients is trouble with language. These aren’t just 'senior moments' or lapses due to stress. People forget everyday words, lose their train of thought mid-sentence, or use incorrect but similar-sounding words without realising it.
“For professionals whose work depends on precise communication, including teachers, writers, and lawyers, this can be particularly debilitating. This linguistic disruption is believed to stem from the same cognitive changes linked to brain fog. Brain scans using functional MRI have picked up changes in how certain language areas connect in some people with long COVID. Regions, such as the prefrontal cortex and temporal lobes, which help with speech and memory, seem to be especially impacted,” explained Dr Umesh.
Beyond cognition, long COVID can present with a host of neurological symptoms:

Something we've noticed in clinics is that women, particularly those in their 30s to mid-50s, seem to be showing these brain-related long COVID symptoms more often than men. There’s no single reason; it could be a mix of things.
Hormones may play a role, especially since oestrogen affects the immune system. Women are also more likely to seek help when something feels off, so these symptoms get picked up more. Another theory is that, in some cases, the immune system stays a little too revved up even after the infection clears. Some women continue to show signs of immune activity months later, including elevated markers that suggest the body hasn’t quite reset itself.
According to a study published in the National Heart, Lung, and Blood Institute, researchers enrolled over 1,500 individuals from across the country who contracted COVID-19 for the first time while pregnant and evaluated their self-reported long COVID symptoms at least six months after infection. They discovered that 9.3% of those who had COVID during their pregnancy continued to experience long-term symptoms.
There’s no fixed treatment plan yet. Care usually focuses on easing symptoms, managing energy levels, and offering supportive therapies. Techniques like cognitive retraining, slow-paced physiotherapy, and calming practices are being looked into. In some cases, medicines, such as low-dose naltrexone, antihistamines, or beta blockers may help, based on what the patient is facing.
More importantly, patients need to be believed. Long COVID is real, and neurological symptoms are not imagined or exaggerated. Dismissing these concerns as anxiety or depression not only delays recovery; it also erodes trust in the healthcare system.
"“There's no fixed treatment plan yet. Treatment usually involves symptom management, energy conservation, and supportive therapies. Researchers are exploring techniques, such as cognitive retraining, gentle physiotherapy, and calming practices. In some cases, medications, such as low-dose naltrexone, antihistamines, or beta blockers may help, depending on the patient's specific needs. It's essential that patients are taken seriously and believed," added Dr Umesh.
Long COVID is a real condition, and neurological symptoms are not imagined or exaggerated. Dismissing these concerns can not only delay recovery but also undermine trust in the healthcare system.
Dr Umesh concluded, “As neurologists, we must approach long COVID with humility and openness. Science is still catching up, and while we don’t have all the answers, we must continue to listen, learn, and adapt. What long COVID teaches us is not just about the virus; it’s about the resilience and vulnerability of the human brain. For every patient who says, 'I don’t feel like myself anymore,' our job is to help them find a way back.”
[ This article contains information provided by an expert and is for informational purposes only. Hence, we advise you to consult your professional if you are dealing with any health issue to avoid complications.]