Lung ultrasound for the diagnosis and monitoring of pneumonia in a tuberculosis-endemic setting: a prospective study
Lung ultrasound for the diagnosis and monitoring of pneumonia in a tuberculosis-endemic setting: a prospective study
Lung ultrasound (LUS) has proven high diagnostic accuracy for community-acquired pneumonia (CAP) in developed countries. However, its diagnostic performance in resource-limited settings with high pulmonary tuberculosis (TB) incidence is less established. Additionally, the role of LUS in monitoring CAP progression remains underexplored.
To validate the diagnostic performance, monitoring and prognostic utility of LUS for CAP in a high pulmonary TB incidence setting.
Prospective single-centre cohort study.
Pulmonary department of a tertiary hospital in Vietnam.
A total of 158 patients suspected of having CAP were enrolled, with 136 (mean age 62 years, 72.8% male) included in the final analysis.
Patients underwent LUS and chest X-ray (CXR) within 24 hours of admission, with a follow-up LUS on days 5–8.
The primary outcome was the diagnostic accuracy of LUS and CXR compared with discharge diagnosis. Secondary outcomes included the accuracy compared with CT scan results, changes in LUS parameters—consolidation size, number and Lung Ultrasound Score (LUSS)—and their association with in-hospital mortality.
LUS demonstrated higher sensitivity than CXR (96.0% (95% CI 90.0% to 99.0%) vs 82.8% (95% CI 73.9% to 89.7%)). LUS specificity was 64.9% (95% CI 47.5% to 80.0%), compared with 54.1% (95% CI 36.9% to 70.5%) for CXR. The moderate specificity for LUS was due to sonographic-similar conditions, notably TB in 5.1% of patients. Consolidation size and numbers showed marginal resolution, while LUSS showed more pronounced decreases over time. The baseline LUSS showed limited discriminative ability for predicting mortality (area under the curve, AUC 0.65, 95% CI 0.55 to 0.75), while follow-up LUSS and changes in LUSS (ΔLUSS) demonstrated higher levels of discrimination (AUC 0.81 (95% CI 0.71 to 0.89) and 0.89 (95% CI 0.80 to 0.95), respectively). For each one-point increase in ΔLUSS, the odds of in-hospital mortality went up by 70% (p=0.002). An improved LUSS effectively ruled out mortality (negative predictive value 97.4%).
Although LUS is highly sensitive for diagnosing CAP, its specificity in TB-endemic regions warrants further caution. Serial LUS assessments, particularly monitoring LUSS changes, are valuable for tracking disease progression and prognostication, with increasing LUSS indicating potential clinical deterioration.
Data are available upon reasonable request.
http://creativecommons.org/licenses/by-nc/4.0/
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Community-acquired pneumonia (CAP) is the leading global infectious disease, presenting significant challenges to public health due to its high hospitalisation and mortality rates.1–3 Effective diagnosis and monitoring are crucial to improve patient outcomes and reduce the healthcare burden. Despite being frequently encountered in both outpatient and inpatient settings, pneumonia diagnosis remains complex. CAP is rarely confirmed through the gold standard of pathology. Instead, the diagnosis relies on concordant evidence of clinical symptoms, microbiological detection and compatible imaging findings, typically new infiltrates on chest radiographs (CXR).4 Despite being a staple for diagnosing CAP for years, CXR may fail to detect or correctly identify pneumonic lesions.5–7
In recent years, alternative diagnostic tools such as lung ultrasound (LUS) have emerged.8 Besides the advantages of being radiation-free, bedside-available and repeatable, studies have shown that LUS offers substantial diagnostic accuracy.9 Multiple meta-analyses revealed that the LUS sensitivity for diagnosing CAP ranges from 85% to 97%, with specificity between 80% and 96%.10–18 However, most of the evidence on LUS diagnostic accuracy for pneumonia was derived from developed countries. There is less emphasis on low-resource settings, where diseases such as tuberculosis (TB) and bronchiectasis can mimic pneumonia sonographically, potentially affecting diagnostic properties.17 Furthermore, the potential of LUS in monitoring and stratifying CAP patients at risk of clinical deterioration is not well understood. In this study, we aim to investigate the diagnostic performance of LUS in a developing country. Additionally, we seek to identify which LUS parameters can effectively monitor and prognosticate CAP.
This prospective observational study was conducted at the Pulmonary Department of Cho Ray Hospital, the largest tertiary hospital in southern Vietnam, from December 2022 to June 2023. Patients or their legally authorised representatives provided written informed consent before enrolment.
There were no patients or public involved in the study protocol.
Patients aged 18 years or older clinically suspected of having CAP according to the American Thoracic Society criteria19 were eligible. This included patient presenting with fever, dyspnoea, cough, sputum production and pleuritic chest pain. Patients were excluded if hospitalised for ≥48 hours before enrolment, pregnant or lactating, or tested positive for SARS-CoV-2 via rapid antigen or RT-PCR assays.
Eligible patients were systematically identified by a pulmonologist overseeing admissions and recruited consecutively. Enrolment occurred promptly on admission, after which data were collected and the sonographer was notified to perform the ultrasound within 24 hours of hospitalisation. Patient data collected included anthropometric measurements, clinical symptoms, medical history and laboratory findings. Information on clinical complications, including in-hospital mortality, need for invasive mechanical ventilation, admission to the respiratory intensive care unit (RICU) and discharge status was also recorded.
An initial LUS was performed by one of the two pulmonologists, each with medical sonographer certification and experience in over 50 LUSs. They were blinded to the patients’ medical records. During this period, patients also underwent CXR. A follow-up LUS was performed between days 5 and 8 by the same pulmonologist. This timeframe was chosen based on the assumption that LUS can detect pulmonary changes with sensitivity comparable to CXR and provide similar benefits.20 Additionally, Reissig et al21 demonstrated that a 5–8 day timeframe effectively detects sonographic changes in pneumonia.
LUS examinations were conducted using a 2–5 MHz curved array transducer of the DP-10 (Shenzhen Mindray Bio-Medical Electronics Co, Shenzhen, China). Patients were examined sitting when possible; otherwise, anterior regions were assessed supine and posterior regions recumbent. The procedure assessed 12 lung zones (figure 1) for pleural irregularities, size and number of consolidations, the presence of air bronchograms, number and characteristics of B-lines and pleural effusion. Consolidation size was measured in one dimension, from the pleural line to the furthest margin. Additionally, the LUSS, a semiquantitative tool for lung aeration ranging from 0 to 3, was assigned to each lung zone.22 Detailed descriptions are presented in figure 2, and the global LUSS was calculated as the sum of regional scores (range 0–36).
Figure 1
Division of 12 lung zones, with six zones allocated to each hemithorax. The zones are divided as follows: each hemithorax is segmented into anterior, lateral and posterior chest areas, demarcated by the anterior and posterior axillary lines. Each area on either side is further divided into an upper and a lower half: (A) anterior chest area: the right hemithorax is divided into an upper zone (R1) and a lower zone (R2); the left hemithorax is divided into an upper zone (L1) and a lower zone (L2). (B) Lateral chest area (right side): features an upper lateral zone (R3) and a lower lateral zone (R4). The left lateral view is not shown. (C) Posterior chest area: illustrates the right upper (R5) and lower (R6) zones, and the left upper (L5) and lower (L6) zones.
Figure 2
Lung Ultrasound Scores (LUSS) for assessing lung aeration, ranging from 0 to 3. (A) LUSS 0, characterised by the presence of A-lines, indicative of normal lung aeration. (B) LUSS 1, where there are three or more B-lines per intercostal space, accompanied by irregular or thickened pleura. (C) LUSS 2, displaying confluent B-lines, with or without subpleural consolidations. (D) LUSS 3, featuring large consolidations with a height greater than 1 cm. LUSS, Lung Ultrasound Score.
The finding of lung consolidation or focal interstitial syndrome (one or multiple zones involved unilaterally) was consistent with a pneumonia diagnosis.23 In cases where bilateral interstitial syndrome was identified, additional ultrasound features such as irregular and thickened pleura, diminished lung sliding, the non-homogeneous distribution of B-lines and subpleural consolidations were required to differentiate pneumonia from cardiogenic pulmonary oedema.24 25
To assess interobserver reliability, we recorded ultrasound procedures, randomly selected 30 recordings and sent them to an expert with registered ultrasound certification to review. We then compared the interpretations of the ultrasound videos between the sonographers and the expert.
Every patient received a posteroanterior CXR (DRX-Ascend System, Carestream, New York, USA) within 24 hours of admission. A board-certified radiologist, blinded to the patient’s clinical and LUS findings, independently reviewed these radiographs.
On discharge, the final diagnosis was confirmed by a panel of two independent pulmonologists who reviewed the patient’s clinical and laboratory findings, radiology, microbiological results and overall clinical course. The assessors were blinded to the LUS data. In case of disagreement, a third expert was consulted, with consensus from at least two experts required for the conclusion.
For patients undergoing CT scans, the result served as a secondary reference for assessing LUS diagnostic values. Scans were obtained using 128-slice Optima CT 660 (GE Healthcare, Chicago, IL, USA) and interpreted independently by a board-certified radiologist blinded to prior clinical and imaging data.
All pneumonia-suspected patients underwent acid-fast bacilli (AFB) staining of at least two sputum samples per the national guideline due to high TB prevalence, supplemented by GeneXpert MTB/RIF and TB culture when indicated. Gastric aspiration or bronchoalveolar lavage for TB workup was performed on a case-by-case basis. Active pulmonary TB diagnosis required compatible symptoms, radiographic findings and microbiological confirmation (positive AFB stain, GeneXpert MTB/RIF or Mycobacterium tuberculosis culture). Patients with a history of previous treatment for TB but no active disease were excluded.
The primary end-point was the diagnostic accuracy of LUS and CXR as index tests compared with the discharge diagnosis. Additional end-points included diagnostic accuracy compared with CT scan results, changes in three LUS parameters (consolidation size, number of consolidations and LUSS) and their association with in-hospital mortality.
A total sample size of 70 and 84 patients was needed to estimate a sensitivity of 85% and specificity of 93% (according to Alzahrani’s meta-analysis17), with a precision of 10% assuming the prevalence of CAP was 70%. Normality was assessed using histograms and the Shapiro-Wilk test. Non-normal variables were described by medians and IQR ranges, while normal variables were described by means and SD. Group differences were analysed with t-tests for normal data and Mann-Whitney U tests for non-normal data. The Wilcoxon Signed-Rank Test assessed LUS parameters over time, while the χ2 or Fisher’s Exact Test evaluated categorical variable differences.
For diagnostic properties, sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and likelihood ratios of LUS and CXR were calculated. McNemar’s test was employed to assess statistical differences in sensitivity and specificity between LUS and CXR. The optimal LUSS cut-off was established using the Youden index. Logistic regression identified associations between mortality and ultrasound parameters but was limited to univariable analysis due to the small number of events. A p-value<0.05 indicated statistical significance. Data were processed using STATA/MP V.17.0 software (StataCorp, College Station, TX, USA).
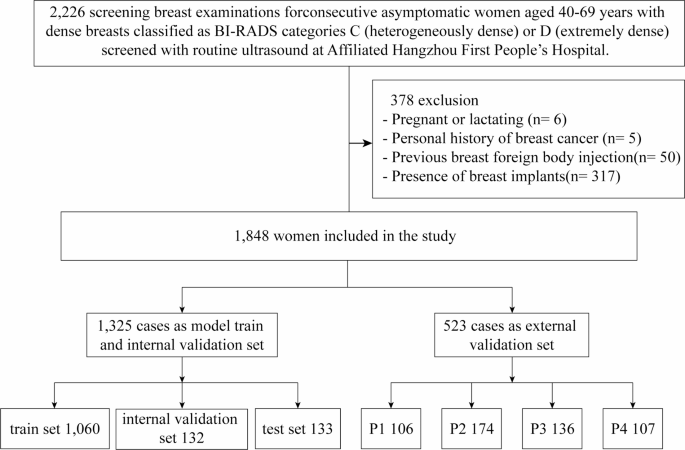
Between December 2022 and June 2023, 158 patients were enrolled (figure 3). Exclusions for hospitalisation≥48 hours prior to admission, self-discharge and hospital transfers left 136 patients for final analysis. The mean age was 62±17 years and 72.8% were male. Demographic and clinical characteristics are presented in table 1. Hospital mortality was 13.2%.
Table 1
Demographic and clinical characteristics of patients with and without pneumonia
CAP was confirmed in 99 patients (72.8%) at discharge. CT scans were conducted in 93 patients, with the median time from admission to scan of 2 (IQR 1–4) days. CAP was confirmed through CT in 72/93 cases (77.4%).
LUS showed a sensitivity of 96.0% (95% CI 90.0% to 99.0%) and specificity of 64.9% (95% CI 47.5% to 80.0%), while CXR had a sensitivity of 82.8% (95% CI 73.9% to 89.7%) and specificity of 54.1% (95% CI 36.9% to 70.5%).
CXR sensitivity was significantly lower than LUS (p=0.002), but specificities did not differ significantly (p=0.103, McNemar’s test; table 2 and online supplemental table 1). Using CT as a secondary reference standard, the performance of LUS showed a sensitivity of 95.8%, comparable to its sensitivity measured against discharge diagnosis as the reference standard. However, specificity was lower at 52.4% (95% CI 29.8% to 74.3%). Results of LUS and CXR compared with CT scan are shown in online supplemental table 2.
Table 2
Diagnostic performance of lung ultrasound and chest X-ray with reference to discharge diagnosis and CT scan
LUS missed lesions not reaching the pleura in two cases, subsequently confirmed by CT scan. In two other false negative cases without CT scans, CAP was confirmed by experts based on clinical signs, elevated inflammatory markers, CXR-detected lesions and positive responses to antibiotics. On the other hand, LUS incorrectly identified pneumonia in 13 patients due to TB (n=6), lung cancer (n=2), heart failure (n=2), bronchiectasis (n=1), chronic obstructive pulmonary disease with fibrosis (n=1) and interstitial lung disease (n=1).
Among 136 patients, M. tuberculosis was detected in respiratory specimens of seven individuals (six false positives and one true positive, as the patient had Pseudomonas aeruginosa in sputum culture, making it CAP with M. tuberculosis coinfection). The six TB cases were older adults (median age 60 (IQR 59–64) years) presenting with a short symptom duration (≤2 weeks). Laboratory tests revealed elevated inflammatory markers: white blood cell count 13.25 (9.8–15.8) 10∧9/L, neutrophil predominance (85.5% (82.5–96.4%)) and elevated CRP (134.7 (115.0–178.1) mg/L), resembling non-TB CAP. CT scans showed consolidations in all six patients, with five exhibiting abscesses or cavitation; other findings included bronchiectasis, multiple small nodules and pleural effusion. While LUS detected the consolidations, it could not visualise the cavitary lesions in these patients.
The time to perform the LUS was under 10 min (median 9 min 38 s). The inter-rater variability was low, with Cohen’s kappa value of 0.89 (p<0.001) for pneumonia diagnosis and 0.85 (p<0.001) for LUSS assessment.
Sonographic characteristics of cases where LUS detected and confirmed CAP on discharge are detailed in online supplemental table 3. In six cases with bilateral interstitial patterns, findings such as irregular and thickened pleura, reduced lung sliding and subpleural consolidations helped distinguish pneumonia from cardiogenic pulmonary oedema. Echocardiography performed in these six cases also confirmed the findings.
A follow-up LUS was performed in 98 out of 136 patients (72.1%), including 75 with pneumonia and 23 without. The median time between admission and the follow-up ultrasound was 55 6 days. At the time of the second ultrasound, 24 patients had been discharged (15 pneumonia patients and nine non-pneumonia patients), while 10 had died, including nine with pneumonia. Among those still hospitalised, two pneumonia patients required mechanical ventilation and six were in RICU (online supplemental table 4). In pneumonia patients, follow-up scans showed only a slight reduction in the size and number of consolidations after 5–8 days, whereas the LUSS demonstrated a more significant reduction (table 3).
Table 3
Comparison of ultrasound findings between initial (LUS 1) and follow-up (LUS 2) assessments
The association of LUS parameters with in-hospital mortality is detailed in table 4. Consolidation size or count was not associated with mortality risk. The global LUSS was associated with mortality (unadjusted OR=1.09, 95% CI 1.01 to 1.16, p=0.021). The baseline LUSS had an area under the curve (AUC) of 0.65 (95% CI 0.55 to 0.75), indicating modest discrimination for predicting mortality, with an optimal cut-point of 17 (52.9% sensitivity, 73.1% specificity). At the second evaluation, the LUSS demonstrated an improved discrimination, with an AUC of 0.81 (95% CI 0.71 to 0.89) and an optimal cut-point of 21 (66.7% sensitivity, 87.9% specificity) and the unadjusted OR was 1.19 (95% CI 1.06 to 1.34, p=0.004).
Table 4
Association of lung ultrasound parameters with in-hospital outcomes in patients with community-acquired pneumonia
All mortality cases had worsening LUSS. Changes in Lung Ultrasound Score (ΔLUSS) over time were also analysed. Patients whose LUSS increased from the initial to the follow-up examination were more likely to die in the hospital. Specifically, each one-point rise in LUSS between the two scans was associated with a 70% increase in the odds of in-hospital death (OR 1.70, 95% CI 1.22 to 2.38, p=0.002). ΔLUSS had a predictive AUC of 0.89 (95% CI 0.80 to 0.95) for in-hospital mortality. Patients with no improvement in monitoring LUS (ΔLUSS≥0) demonstrated a sensitivity of 88.9%, specificity of 57.6%, NPV of 97.4% and PPV of 22.2% in predicting mortality (table 5).
Table 5
Cut-off points of ΔLUS in predicting in-hospital mortality
This study confirmed that LUS has a higher sensitivity than CXR for diagnosing CAP. However, its moderate specificity may be influenced by the difficulty in differentiating pneumonia from other respiratory conditions, particularly TB. To the best of our knowledge, this is one of the first studies to incorporate LUSS for monitoring CAP. Our findings indicate that LUSS changes over time may offer preliminary prognostic insights, potentially aiding in the identification of disease progression and mortality risk stratification.
Previous studies have shown that LUS has a high sensitivity for detecting pneumonia.14–17 Our study aligns with these findings, demonstrating greater sensitivity than CXR. These results reaffirm LUS as a reliable tool for ruling out pneumonia. However, if ultrasound is negative but other pneumonia signs persist, further investigation and close monitoring after antibiotic treatment are necessary for a definitive diagnosis. Despite showing great sensitivity, LUS specificity was lower than in prior reports14–17 and varied depending on the reference standard used. The lower specificity observed with CT as the standard, compared with a clinical panel combining clinical features and CXR, reflects CT’s superior ability to detect detailed pulmonary changes. Studies have also shown that clinical features and CXR frequently lead to misdiagnosis of CAP compared with CT.5 While LUS is more sensitive than CXR in detecting interstitial abnormalities and consolidations, it shares similar limitations, such as difficulty in distinguishing acute from chronic changes and less detailed lung pattern analysis compared with CT. For example, B-lines on LUS may indicate acute infections or chronic fibrotic processes, and hypoechoic lesions may also signify various pathologies, including pneumonia, atelectasis, lung cancer, pulmonary embolism, or nodular scarring.
Our findings indicate that LUS has difficulty in differentiating pneumonia from other respiratory diseases, with TB being the most frequently misdiagnosed. In this study, we classified pulmonary TB as false positive rather than a type of CAP. This decision was based on the rationale that the diagnosis determines subsequent antibiotic strategies, which differ between the two conditions. While some sonographic findings (eg, subpleural nodules, pleural effusion and consolidation with fluid collections) may suggest TB, the modality is inherently limited in detecting cavity lesions, which are a consistent radiological feature in our TB patients, due to air within cavities preventing ultrasound penetration. This is particularly relevant in our setting, which reported the highest number of TB cases among LUS studies on CAP. In contrast, previous research, primarily conducted in low-TB-prevalence settings, found no TB cases, while studies in endemic areas such as Liu26 in China and Amatya27 in Nepal reported zero and one case, respectively. Our study’s TB prevalence of 6.7% (7/105) notably surpasses the global average of 0.86% reported by a multicentre CAP study, which included non-endemic regions such as Europe (0.97%) and North America (1.02%),28 while aligning more closely with figures from other high-burden settings, including Hong Kong29 (8.1%) and the Philippines30 (9.8%). These findings highlight the diagnostic challenges of LUS for pneumonia in TB-endemic regions, where sonographic presentations of TB and pneumonia often overlap. Clinically, when consolidations (with or without complementary features such as pleural effusion or subpleural nodules) appear alongside a clinical suspicion of TB, further evaluation with CT scans and TB-specific workup is indispensable. Larger, targeted studies are needed to better characterise ultrasound findings in TB.
Besides evaluating the diagnostic properties, our study aimed to observe sonographic changes in CAP over time and assess whether these changes could aid in monitoring and predicting clinical outcomes. We focused on three ultrasound parameters: consolidation size, number of consolidations and LUSS. Previous studies in both paediatric28–30 and adult populations21 suggest that disease remission can be observed through the resolution of lesion sizes and numbers. However, our findings indicate that changes in the size and overall number of consolidations during follow-up assessments were relatively small. These marginal changes may not be readily apparent to clinicians, making it less ideal to utilise these parameters for monitoring purposes. The difference in pneumonic lesion resolution between our study and that reported in the adult population by Reissig21 may stem from variations in measurement methods and sample selection. We used a one-dimensional measure for the largest consolidation, whereas Reissig et al employed a two-dimensional measure in square centimetres. Additionally, for comparisons of lesion size at two time points, our initial assessment only included subjects available for a follow-up ultrasound, in contrast to Reissig’s approach, which involved measuring pneumonic size in all patients, regardless of follow-up availability.21
The LUSS has recently emerged as a useful tool for assessing severity, and the baseline score is closely related to adverse outcomes in COVID-19 patients.31 Our analysis showed that the baseline score has limited predictive value for in-hospital mortality. Instead, the dynamic changes in the LUSS during follow-up may offer a more reliable indication of mortality. Hypothetically, since the LUSS incorporates both consolidation and interstitial components, and considering that changes in consolidation measurements were small, it is possible that changes in the interstitial pattern occur earlier and are more predictive of the clinical course of CAP than consolidative changes. From the clinical practice perspective, LUSS progression should alert physicians about a deteriorating clinical course. A ΔLUSS cut-off of 0 is clinically applicable as it allows for the simple categorisation of patients into groups with improved or unimproved LUSS over time. Patients with no improvement in monitoring LUS (ΔLUSS≥0) demonstrated a sensitivity of 88.9%, specificity of 57.6%, NPV of 97.4% and PPV of 22.2% in predicting mortality. The high sensitivity and NPV suggest that a ΔLUSS≥0 is effective in identifying patients at risk of mortality, the moderate specificity and PPV indicate that ΔLUSS should be used in conjunction with other clinical indicators. Utilising LUSS for stratification may lead to a more efficient allocation of medical resources, ensuring that attention and care are prioritised for patients with a higher risk of mortality. Timely interventions, such as escalating antibiotics, advanced imaging and microbiology workup may prevent progression to critical illness and ultimately reduce mortality. However, as our observations are based on a limited sample size, further studies on sonographic pneumonic lesion evolution and their impact on clinical outcomes are needed to validate these findings.
This study has several limitations. First, due to ethical reasons, a CT scan was not performed on all patients, leaving the possibility of missing or misidentifying pneumonic lesions. However, in those who did receive a CT scan, the performance of LUS was found to be comparable to both discharge diagnosis and CT imaging, indicating the former’s reliability. Second, the consolidation size was recorded in a single dimension, which does not fully capture the lesion’s three-dimensional volume. However, measurements in one dimension have been shown to effectively represent overall lesion volume.29 Third, as the study focused on inpatients, its findings may not extend to outpatients, who often have smaller, more rapidly resolving lesions. Additionally, some patients were discharged before the second ultrasound, potentially skewing follow-up data away from those with milder disease. However, similar to CXR, follow-up ultrasounds may be unnecessary for patients showing early recovery, as their clinical symptoms suggest resolution without additional imaging. For patients who died early before the second ultrasound, it is plausible they had more progressive lesions, potentially amplifying our findings. Fourth, while some clinical data (eg, mechanical ventilation and RICU admission) were recorded at the time of the second LUS, other dynamic parameters such as trends in vital signs, oxygen therapy escalation, lactate levels or renal function were not captured. Incorporating these variables could provide a more comprehensive prognostic assessment, as the absence of such data renders the prognostic value of LUSS less certain. For example, in patients with clear signs of deterioration, conducting an intensive LUS protocol may offer limited benefit, whereas follow-up LUS could be more valuable for those with uncertain trajectories. Future research should explore integrating LUSS with dynamic clinical data to improve risk stratification. Finally, ultrasound is an operator-dependent tool, and its interpretation is subjective to sonographer’s experience. Nevertheless, our study demonstrated high reliability between performers.
LUS serves as a non-invasive, rapid and bedside-accessible modality with high sensitivity for detecting CAP. However, the sonographic similarities between pneumonia and other respiratory conditions, such as TB, particularly in endemic regions, require careful interpretation and consideration of the clinical scenario, as well as further workup, to ensure accurate diagnosis. Monitoring with LUS revealed that consolidation size and total lesion resolved slowly. In contrast, changes in the LUSS were more notable. An increasing LUSS was strongly predictive of in-hospital mortality, making it a valuable tool for monitoring disease progression and stratifying patients at risk.
Data are available upon reasonable request.
Consent obtained directly from patient(s).
This study involves human participants. Ethical approval for this study was obtained from the Ethical Committee for Biomedical Research (no. 875/HĐĐĐ-DHYD). The study was conducted in accordance with the Declaration of Helsinki. Participants gave informed consent to participate in the study before taking part.
The authors thank Thong Dang-Vu, Dung Lam-Quoc and the staff at the Pulmonary Department, Cho Ray Hospital, for their assistance in data collection and all the patients for participating in this study.