BMC Health Services Research volume 25, Article number: 882 (2025) Cite this article
Palliative care can improve the quality of life of people with dementia. However, nurses and other healthcare professionals often lack the confidence and skills to provide palliative care and struggle to initiate timely conversations about wishes and needs for palliative care. The DEDICATED approach aims to enhance the quality of palliative dementia care by improving knowledge, competencies, and interprofessional collaboration of healthcare professionals. This study explores its impact on palliative care provision from the perspectives of: (1) healthcare professionals implementing the approach; (2) their care team members; and (3) bereaved family caregivers.
This multi-method evaluation study used: (1) qualitative interviews with those who had acted as ambassadors in implementing the DEDICATED approach; (2) questionnaires measuring perceived self-efficacy, work engagement, and psychological empowerment among healthcare professionals working in these ambassadors’ teams; and (3) questionnaires with bereaved family caregivers exploring the frequency of advance care planning discussion and their experiences with the end-of-life care provided to their relative with dementia.
The DEDICATED approach was implemented across 28 wards in three healthcare organizations. Interviews with ambassadors (n = 17) revealed that the approach raised awareness about person-centered palliative care and the importance of timely advance care planning (ACP) for people with dementia. DEDICATED showed no significant impact on healthcare professionals’ self-efficacy, work engagement, and psychological empowerment. The frequency of ACP discussion and quality of end-of-life care showed no significant differences over time.
DEDICATED ambassadors found the DEDICATED approach to be of value in enhancing person-centered palliative care. Although quantitative assessments of healthcare professionals’ competence did not fully capture this, the positive feedback received suggests that more time may be needed for the approach to be fully integrated into practice. This could explain the modest results observed among team members and bereaved family caregivers. Future research should explore the long-term impact of the DEDICATED approach using longitudinal study designs.
Dementia is a chronic, incurable condition [1], and palliative care aims to improve quality of life for individuals with life-limiting illnesses [2]. While the optimal timing for initiation is ambiguous [3,4,5,6], an early introduction of palliative care in dementia is recommended to improve quality of life across the whole disease trajectory [7, 8]. Palliative care aims to improve the quality of life of a person with a chronic disease, focusing on physical, psychological, social, and spiritual needs [1]. Advance care planning (ACP) is an essential component of palliative dementia care, as cognitive decline and communication difficulties can hinder discussions about palliative care preferences, making timely ACP crucial for aligning care with the wishes and needs of the person with dementia [9,10,11,12]. However, healthcare professionals (HCPs) can experience difficulties with the timing of ACP conversations or lack confidence in their communication skills [13,14,15]. In addition, insufficient knowledge and competencies (e.g., related to pain management and interprofessional collaboration, etc.) can hinder the provision of person-centered palliative care at home or in nursing homes [9, 16,17,18,19,20,21].
Lastly, palliative dementia care requires coordination across care settings, such as home care, hospital and nursing homes [21, 22]. Effective interprofessional collaboration in these settings is challenging but essential for continuity of care throughout the disease trajectory [6, 8, 10, 21]. Overall, HCPs, family caregivers, and people with dementia emphasize the need for improved person-centered care and collaboration [23]. Research suggests that training, tools, and knowledge can enhance palliative care provision [24,25,26]. Co-creation of such healthcare interventions is increasingly valued, as user-driven approaches can improve effectiveness [27, 28]. However, to our knowledge, interventions rarely address the full dementia trajectory while also incorporating input from all stakeholders [29,30,31].
The DEDICATED (Desired Dementia Care Towards End of Life) approach was co-created to improve the quality of palliative care for individuals with dementia by enhancing HCPs’ skills, knowledge, and competencies in palliative dementia care [32]. This study explores its impact on palliative care provision from the perspectives of: (1) HCPs implementing the approach; (2) their care team members; and (3) bereaved family caregivers.
The DEDICATED approach to dementia-specific palliative care consists of a training format and practice tools. The ultimate goal of the DEDICATED approach is to empower HCPs involved in the provision of palliative care for people with dementia to improve the quality of such care. The DEDICATED approach can be applied from the point of diagnosis and throughout the entire disease trajectory of the person with dementia. Tools of the DEDICATED approach can be used during specific stages of the trajectory. For instance, the tools for ACP might be more suitable in the diagnosis or early stages of dementia, while the tools for a warm transfer to a nursing home can be used later in the care trajectory. A description of the DEDICATED approach, its development and implementation has been provided elsewhere [32]. In brief, the development of the DEDICATED approach included an extensive needs assessment, in which needs for palliative care provision were inventoried from the perspective of people with dementia, family caregivers, and HCPs [16, 33,34,35,36,37,38]. From the results of the needs assessment, six central themes were extracted, and tools (e.g., communication tools for ACP, informative clips about dementia care, etc.) were developed in iterative co-creation sessions to address the following themes:
In addition to practical tools, a DEDICATED training program was developed to educate HCPs about the content of the DEDICATED tools and how to implement it in practice. HCPs who have completed the DEDICATED training are known as DEDICATED ambassadors. DEDICATED ambassadors are HCPs who play an important role in stimulating awareness about palliative dementia care and in implementing the DEDICATED approach in practice [32].
The DEDICATED approach was built by a development team consisting of HCPs, education professionals, and representatives of people with dementia. This team was directly involved in the iterative co-creation and pilot testing of the DEDICATED approach in practice. HCPs involved in caring for people with dementia from this development team were trained to become the ‘first wave’ of DEDICATED ambassadors (n = 14). After the co-creation of the DEDICATED approach was finalized, a ‘second wave’ of ambassadors was trained to implement and evaluate the DEDICATED approach in practice (n = 10). Thus, both the first-wave and second-wave ambassadors implemented the DEDICATED approach in practice, whereas only the first wave of ambassadors was involved in the co-creation and pilot testing phase.
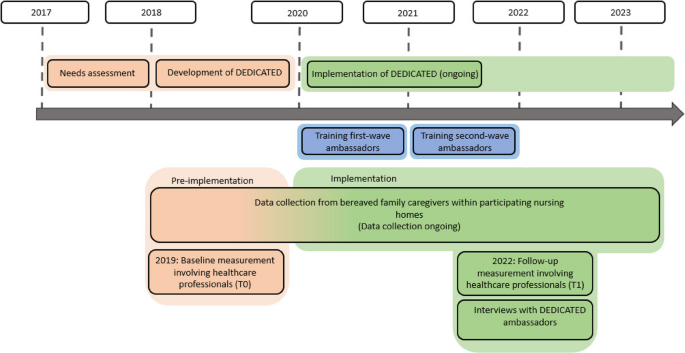
This study involved a multi-method design, and was conducted over a period of six years (Fig. 1), aiming to evaluate the impact of the DEDICATED approach in practice based on three forms of data collection:
Timeline of development and implementation of the DEDICATED approach and data collection for this study
Population and recruitment
After implementation of the DEDICATED approach, all DEDICATED ambassadors (n = 24, at the time) were invited to participate by email. After they had agreed to participate, an online interview was scheduled.
Data collection
We performed one-to-one, semi-structured interviews with ambassadors during the implementation phase [39] (Fig. 1). Due to COVID-19 restrictions, the interviews were held online using Microsoft Teams and recorded using Microsoft Game Bar. The DEDICATED research team developed an interview guide that contained questions about how the impact of the DEDICATED approach was experienced in practice (Additional file 1). The interview guide was based on relevant literature, such as the Dutch Palliative Care Quality Framework [40], and revised by members of the research team (JB, JM, SB, LD, CK and EK) following input from an advisory board consisting of experts from the practice and education fields (n = 21).
Data analysis
Interview transcripts were analyzed using Atlas.ti version 9 software (Atlas.ti Scientific Software Development GmbH). The interview recordings were transcribed verbatim and analyzed using a conventional content analysis approach (CCA). In a CCA approach, open codes flow directly from the data, without the imposition of specific theoretical presumptions formed in advance of data analysis [41]. First, three researchers (JB, TW, and SB) read all transcripts thoroughly. After this, the transcripts were independently coded using four intermediate reflective sessions which allowed cross-validation of codes and categories. SB and JB continued axial coding as an iterative process, moving back and forth between the transcripts to refine codes and to cluster them into categories. A list of final codes and categories was defined within the primary research team (JB, JM, SB, DJ).
Population and recruitment
The DEDICATED approach was implemented within healthcare organizations that belonged to Living Lab in Ageing and Long-term Care Limburg (AWO-L), a consortium of collaborating healthcare organizations providing (palliative) care for older persons [42]. The 28 involved long-term care wards belong to three organizations which are part of the AWO-L. These nursing wards are located across various sites in the south of the province of Limburg, the Netherlands. The DEDICATED ambassadors’ care team members were requested to fill in a questionnaire at baseline and follow-up measurement points relating to self-efficacy, work engagement and psychological empowerment (Fig. 1).
The DEDICATED ambassadors’ team members were eligible to participate if they: (1) worked directly with the DEDICATED ambassador and (2) were directly involved in palliative care for people with dementia. Questionnaires were also distributed to team members from a control group. The control group was also recruited from AWO-L organizations; however, it consisted of nursing home wards and home care teams with no active role in the development or testing of the DEDICATED approach. These wards and teams were selected by managers from the participating organizations.
In summary, team members were sorted into three experimental groups:
Data collection and measurements
Three validated scales, namely the Palliative Care Self-Efficacy Scale (PCSES), Spreitzer’s Psychological Empowerment scale (PE) and the Utrecht Work Engagement Scale (UWES-9), were used to explore self-efficacy, work engagement, and psychological empowerment. In addition, we elicited descriptive information such as: participant’s age, years of work experience, years working in an intra- or extramural setting, occupation, and gender. The three scales were combined into one questionnaire, which was sent to participating team members in the test, design, and control groups. Paper versions of the questionnaires at the baseline measurement point (2019) were distributed via DEDICATED ambassadors to participating teams in the design group and via unit and team managers for the test and control group. Digital versions of the questionnaires were distributed to the design and test groups at follow-up (2021) via DEDICATED ambassadors using Qualtrics, which is an online data management platform (Qualtrics International Inc., Provo, UT; 2024). The control group received the digital questionnaire via their managers. Questionnaire return was anonymous, and the study design ensured that collected data could not be traced back to specific individuals.
The primary outcome was self-efficacy in providing palliative care for people with dementia, which was measured using the PCSES [43]. The PCSES is a validated instrument which was developed to assess the self-efficacy of nursing staff providing end-of-life care [43]. The PCSES comprises 12 items and two subscales: Psychosocial support and symptom management. The PCSES was designed to be rated using a four-point Likert-scale with the response options: (1) need further basic instruction, (2) confident to perform with close supervision/coaching, (3) confident to perform with minimal consultation, or (4) confident to perform independently [43]. Higher scores indicate higher perceived self-efficacy. The overall scale has demonstrated excellent internal consistency (Cronbach’s α = 0.92) in a population of nursing staff working in care facilities (n = 405).
As secondary outcomes, we assessed psychological empowerment (PE) and work engagement. We used the PE-scale for psychological empowerment [44, 45]. PE was defined more broadly as increased intrinsic task motivation, manifested in a set of four cognitions reflecting an individual’s orientation to their work role: meaning, competence, self-determination, and impact [44, 45]. Each of these four aspects is a subscale in the PE scale. Each subscale is assessed in the PE questionnaire by three items and scored on a five-point Likert scale (ranging from 1 = strongly disagree to 5 = strongly agree). Higher scores indicate higher perceived psychological empowerment by HCPs. The PE instrument has good construct validity, and its subscales have demonstrated good (Cronbach’s α = 0.80) to excellent (Cronbach’s α = 0.92) reliability in a population of nursing staff [44]. We translated the PCSES and PE scale into Dutch using a forward-backward approach, with assistance from a native English speaker. Afterwards, we calculated Cronbach’s α for reliability. The UWES-9 was used to assess work engagement [46]. Work engagement is defined as a positive work-related state of fulfilment that is characterized by vigor, dedication, and absorption [46]. The UWES-9 is available in Dutch and comprises nine items that are scored on a seven-point Likert scale (ranging from 0 = never to 6 = always (every day). Higher scores indicate greater work engagement. The instrument has demonstrated excellent reliability for measuring work engagement as a single factor in a population of nursing staff across ten different countries [46].
Data analysis
Data from questionnaires with team members were aggregated at group-level (i.e., design, test, or control group) using IBM SPSS version 28.0 (IBM Corp., Armonk, NY). Descriptive statistics were calculated to summarize participant characteristics and outcome measures, using mean and standard deviation for continuous variables, and frequencies and percentages for categorical variables. Differences in participant characteristics were tested by independent t-tests [47] and Chi-square [48] tests, respectively.
Inferential statistics were performed to study differences in outcome measures. Within-group changes over time (i.e., from baseline to follow-up) were assessed using separate independent t-tests for the design and control groups, given that both groups included categorical and continuous variables [47]. Between-group differences were analyzed using a multiple linear regression at the follow-up measurement [49]. The linear regression models were adjusted for possible confounding variables, namely: age of the participant, years of work experience, working in an intra- or extramural setting, occupation, and gender. This approach allows for the estimation of the effect of the categorical variable (i.e., design, test or control group) on the continuous outcome (i.e., scores op the EPCS, PE-scale and UWES-9) while controlling for other influencing factors [49]. Statistical tests and analyses were performed in collaboration with a statistician (NH).
Population and recruitment
From the start of the DEDICATED project in 2017, up to December 2023, bereaved family caregivers of persons with dementia who received care from one of the AWO-L partner organizations were invited to complete a questionnaire. During this period, the DEDICATED approach was developed, tested, and implemented in practice. Figure 1 provides a visualization of these pre-implementation and implementation phases and the respective data collection at each phase through questionnaires with bereaved family members. The partner organizations included the questionnaire as part of their standard quality evaluation, sent to bereaved families six weeks after the death of their relative. Bereaved family caregivers received paper versions of the information letter and questionnaire by mail. The information letter stipulated that returning the questionnaire indicated consent to participate in the study. Collected data could not be traced back to specific individuals and the questionnaire was returned anonymously. There was no follow-up for individuals who did not return the questionnaire.
Data collection and measurements
The questionnaire elicited the demographic characteristics of bereaved family caregivers: age, sex, relationship to the person with dementia and care location. The names of the specific wards where their relatives had been treated were not requested. Bereaved family members were asked to indicate if ACP conversations had taken place between HCPs, the person with dementia, and family caregivers regarding wishes and needs in regard to palliative care in the final phase of life. Bereaved family members could answer the question either: ‘’yes,’’ ‘’no,’’ or ‘’partially’’. Additionally, family members were asked if stated wishes had been respected during care provision. In addition, the validated End-of-Life in Dementia (EOLD) scales were completed by bereaved family caregivers of people with dementia who received palliative care. We used the EOLD Satisfaction with Care (SWC), Symptom Management (SM), and Comfort Assessment in Dying (CAD) scales [50,51,52]. In this study, the EOLD-SWC, which uses a four-point Likert scale, had a score range of 10 to 40 [50,51,52]. The EOLD-CAD uses a three-point Likert scale and had scores ranging from 14 and 42 [50,51,52]. Lastly, the EOLD-SM uses a six-point Likert scale and scores ranged between 0 and 45 [50,51,52]. Higher scores within the questionnaires indicated higher satisfaction with care, better symptom control, and a better quality of dying. The questionnaires were filled out from February 2018 to December 2023 and data collection is ongoing at the time of writing. The DEDICATED approach was developed and implemented during this period.
Data analysis
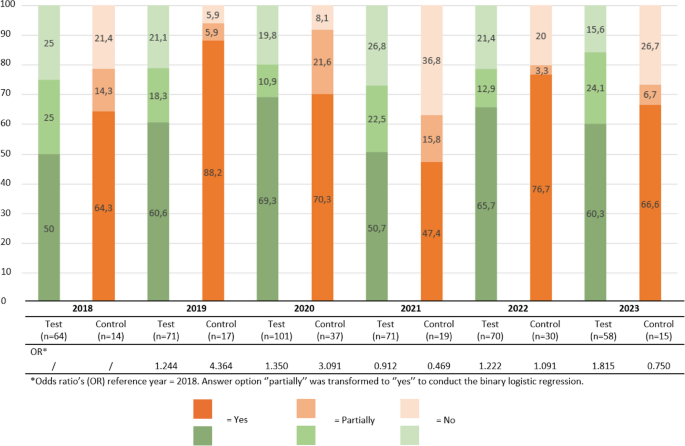
Binary logistic regressions were performed to analyze differences in frequencies of ACP over time. We used the study’s duration years (i.e., 2018, 2019, 2020, 2021, 2022 and 2023) as the categorical predictors and made dummy variables of the years, using 2018 as the reference year. Logistic regressions were performed separately for the test and control group, to analyze if the DEDICATED approach impacted frequencies of ACP discussions. Therefore, the dataset of bereaved family caregivers were split into two groups:
In order to conduct the logistic regression, the answer options to the question about ACP needed transformation to binary answers only. Therefore, the answer options ‘’yes’’ and ‘’partially’’ were transformed to ‘’yes’’, as partial ACP conversations still indicates that actions were taken within our study population. In addition to the logistic regression, frequencies of ACP and wishes being acted upon were calculated descriptively for each year of the study’s duration. The EOLD scales were analyzed using analysis of variance (ANOVA). Descriptive statistics are provided for the participants. Data analyses were conducted using IBM SPSS version 28 (IBM Corp., Armonk, NY).
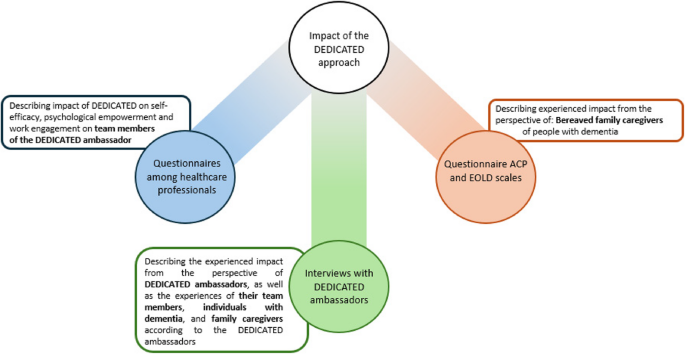
The DEDICATED approach was implemented in three AWO-L healthcare organizations, comprising 28 wards where people with dementia received palliative care. Figure 2 illustrates the integration of the results, showcasing the experienced impact of the DEDICATED approach in practice from the various perspectives.
Findings of the three studies describing the impact of the DEDICATED approach from the perspective of DEDICATED ambassadors, team members, people with dementia and (bereaved) family caregivers
Interviews took place between April and June 2022. We interviewed 17 out of 24 active DEDICATED ambassadors about their perceptions of the impacts of working with the DEDICATED approach. The other seven ambassadors were invited but did not participate due to illness or other work priorities. Seven participants belonged to the first wave of ambassadors and ten belonged to the second wave. Their mean age was 33.4 years, and most were nurses (n = 8) or certified nurse assistants (n = 5). Other participants were dementia case managers (n = 2), a psychologist, and a nurse manager. The results of the interview analysis are structured in three sections: (1) Impact according to the DEDICATED ambassador, (2) Impact on team members of the DEDICATED ambassador and (3) Impact on the person with dementia and their family caregivers. These findings are described in six themes, each containing several subthemes. Table 1 presents these themes and subthemes.
Impact of DEDICATED on ambassadors
The DEDICATED approach raises awareness and knowledge about palliative care.
DEDICATED ambassadors felt more aware that palliative care extends beyond end-of-life care. In addition, DEDICATED ambassadors felt more aware that they have an important role to play within the palliative care trajectory, for instance, by conducting ACP conversations and ensuring continuity in the care provided to people with dementia.
‘’I started as someone who didn’t know much about palliative care itself. I mainly thought of it as just the terminal phase, the final stage of palliative care. But throughout the process, I gained more knowledge and a deeper understanding of palliative care in general. I also received more tools to help me deepen my own understanding and to guide my team in this area. That was really helpful’’. (P.9, Nurse, second-wave ambassador).
In addition, DEDICATED ambassadors found that the enhanced knowledge and awareness they had gained from the approach helped them to acknowledge the human behind the disease, their life story, and needs. Ambassadors used the tools from the DEDICATED approach to identify this information.
‘’I started to see the resident as a resident. As a person. A person with a life instead of a resident with a disease’’. (P.1, consulting palliative care nurse, first-wave ambassador).
‘’Yes, what DEDICATED has given me, is thinking about that aspect of the life story, right. You are always looking for that a bit, right. I also find it very important that when you write a profile of a client, you describe much more of the client’s entire life, so you know, you have conversation topics with the client.’’ (P.5, Dementia case manager, first-wave ambassador).
DEDICATED ambassadors explained that the DEDICATED approach has an impact on their work engagement and enthusiasm. DEDICATED ambassadors described that they felt motivated by the new knowledge they had gained, and that this increased their work satisfaction.
‘’Yes, I think you gain a lot of knowledge, but also more awareness, really. You seek more collaboration with others, so yes, it brings you a lot. And it especially brings you more job satisfaction, as I feel like, ‘Oh no, I’m really doing something good for the client.’’’ (P.6, Psychologist, first-wave ambassador).
The DEDICATED approach enhances practical skills and competencies.
Ambassadors gave specific examples of how certain tools associated with the DEDICATED approach had helped them (or their colleagues) in their care provision or in their teams’ knowledge development. For instance, they used communication tools, such as photo cards, to start conversations on topics that were difficult to address, like wishes and needs for the end of life. Additionally, other DEDICATED approach tools helped them to identify symptoms and problems, such as pain or agitation. Thus, according to ambassadors, using the DEDICATED approach can positively influence palliative care provision, through enhancing the competencies and skills of HCPs.
“The ABC-form and PASLAC-D (i.e., tools for identifying pain and responsive behavior), we already used those. But I have to say, since I have been involved in DEDICATED, I am more inclined to use them. I am more aware of this and now actively promote their use. So, I noticed that they are used more frequently.” (P.17, Nurse, second-wave ambassador).
The DEDICATED ambassadors indicated that the DEDICATED approach motivated them to act and improve aspects of palliative care provision, through means such as timely initiation of ACP conversations or improved preparation of the person with dementia prior to a move to nursing home care. Nevertheless, DEDICATED ambassadors expressed that they sometimes lack confidence in finding the right time to start these conversations and in knowing which topics should be discussed as part of ACP.
‘’Well, what it mainly taught me is the aspect of moving a client from home to a nursing home—don’t call it an admission, call it a move. That really stood out. And how important that process is. That you need to work towards it gradually. That a client should have the chance to get used to it, to first go there for a coffee, to first get acquainted. The whole process of moving from home to a nursing home simply needs to change.’’ (P.13. Home care nurse, second-wave ambassador).
Impact on care team members, according to DEDICATED ambassadors
Awareness of person-centered palliative care among team members.
DEDICATED ambassadors mentioned that implementation of the DEDICATED approach has affected their care teams. For example, the DEDICATED approach made team members more aware of their roles and of the importance of proactively initiating conversations with people with dementia regarding their wishes and needs. On the other hand, in previous research, DEDICATED ambassadors had expressed the need for additional implementation strategies, because involving the whole care team in DEDICATED was found to present challenges if the approach was not structurally embedded and used in practice.
‘’Yes, it has opened my eyes because now I see everyone that needs to be involved and what we can offer the residents. And I do notice that now, as a team, we are quicker to respond when something changes with someone, so that we can act faster based on what we observe or what a resident needs.’’ (P.9, Nurse, second-wave ambassador).
Ambassadors indicated that the skills, knowledge, and professional attitude of their team members were enhanced after being introduced to DEDICATED. As the care team better learns its own strengths and areas of improvement, which can stimulate joint learning and may ultimately improve the quality of care for people with dementia and their families. For instance, one DEDICATED ambassador explained that by getting to know a person with dementia, HCPs can more easily alleviate discomfort or stress for that person.
“Regarding the use of a person’s life story, I notice that many colleagues now bring that up when someone is in distress. It often helps to talk about the past with the person’’. (P.2, Quality nurse practitioner, first-wave ambassador).
Increased collaboration among team members.
Furthermore, the DEDICATED approach highlighted the importance of collaboration between team members, such as information exchange between involved HCPs that supports the provision of consistent and continuous care. Additionally, DEDICATED ambassadors explained that using the “Chatter jar” (i.e., a tool containing question cards related to palliative care, end-of-life care and interprofessional collaboration) gave the team members new insights regarding different roles, responsibilities and needs of the members of their care teams. One ambassador explained that he felt that he was part of the whole care trajectory and belonged to the interprofessional team, instead of providing care for people with dementia on his own.
‘’Yes, I find it especially useful with colleagues because it allows for multidisciplinary discussions, opening up the topic for conversation. But also, allied HCPs often tend to think, ‘Well, that’s not our concern, that’s something for the doctor.’ Or maybe they think it’s something for the psychologists to handle if someone gets very upset and needs to talk about it. However, we all play such an important role in this, and we’ve tried to convey that. What each person’s role as a caregiver is; because often patients interact much more with a physiotherapist than a psychologist—they know them, they trust them. So, how can that person play an important role in this entire process, this care process, or in the quality of life?” (P.6, Psychologist, first-wave ambassador).
Impact on the person with dementia and family caregivers, according to DEDICATED ambassadors
The life story of the person with dementia is better understood.
DEDICATED ambassadors found the DEDICATED approach helpful in gathering personal information (such as the biography, wishes, needs, and values of people with dementia). Access to that information could in turn provide a basis for further interaction and topics of conversation. For example, a first-wave ambassador explained that she used DEDICATED in a group of family caregivers and people with dementia. This provided an opening to share more comprehensive information, which could later be useful in the course of palliative care provision.
‘’Yes, what I like is that, for example, we have informal caregivers who come to the psychogeriatric wards. They come to visit their family. The HCPs on the ward gather several caregivers and people with dementia together for a cup of tea. So, they sit with a group of about five people. And yes, how do you start the conversation, and what do you talk about? They approached me, asking if I had something they could use to share, to start a conversation and share information’’. (P.1, Consulting palliative care nurse, first-wave ambassador).
Ambassadors recognized that investing in care relationships had added value for family caregivers as well. For instance, investing in a close care relationship with a person with dementia led to greater satisfaction among family members. Tools such as the life story poster or book could contribute to this, especially if family caregivers play a role in creating them. This could help in building a trustful relationship between the HCPs and family caregivers.
‘’And you learn a lot about those clients, which makes family much more engaged in providing person-centered care. So really just looking at who the person behind the disease is and how we interact with them.’’ (P.2, Quality nurse practitioner, first-wave ambassador).
In total, 105 team members completed the questionnaires at the baseline measurement and 110 team members completed the questionnaire at the follow-up measurement (Table 2). The composition of professions and work settings represented in the design and control groups differed significantly between the baseline and follow-up measurement.
Table 3 shows the mean sum scores of the three scales at the baseline and follow-up measurement points. A significant decline is observed in the total sum score for the PCSES scale (i.e., self-efficacy) in the design as well as the control group. In the control group, scores for the UWES-9 scale (i.e., work engagement) increased significantly. The between-group comparison at the follow-up measurement (Table 4) showed no statistically significant differences.
Within the timespan of February 2018 to August 2023, 567 bereaved family caregivers answered the question about whether wishes and values for end-of-life care had been discussed. Of these, 77% (n = 435) of respondent caregivers’ relatives with dementia received care in test/design group units (where DEDICATED was implemented by the DEDICATED ambassador), and 23% (n = 132) respondent caregivers were part of the control group (where DEDICATED was not implemented). Table 5 provides the characteristics of the bereaved family caregivers included in this study.
Percentage of bereaved family caregivers indicating that wishes and needs for the end of life were discussed and documented in the groups where DEDICATED was implemented by the ambassador (i.e., test/design groups) and where it was not (i.e., control group)
Binary logistic regression analyses for the test and control group indicated no significant difference in ACP conversations throughout the research period (Fig. 3). Odds ratio’s (OR) in the test and control group were mostly higher compared to 2018, with 2021 being an exception for both groups, and 2023 for the control group only. In total, 449 family caregivers indicated that wishes and needs were completely or partially discussed. The follow-up question was answered by 252 family caregivers from the test/design group, and 71 from the control group. In the test/design group, the percentage of family caregivers indicating that wishes and needs were acted upon was comparable in 2018 (79.2%) and 2023 (89.1%). Due to the small numbers (n = 71) of respondents in the control group over the given timespan, no results are given for this follow-up question.
The EOLD-CAD, EOLD-SWC, and EOLD-SM scores showed small fluctuations over time, which were found not to be statistically significant (Table 6). This applied to both the wards that implemented the DEDICATED approach and those that did not.
This multi-methods study explored perceptions of the impact of working with the DEDICATED approach. We analyzed the perspectives and data of: (1) DEDICATED ambassadors; (2) the ambassadors’ team members; and (3) bereaved family members of persons with dementia. The results deriving from various perspectives and methodologies showed varying outcomes regarding the overall impact of the DEDICATED approach. DEDICATED ambassadors described positive experiences with the DEDICATED approach in practice. As regards their care team members, there were no significant changes in terms of perceived self-efficacy, psychological empowerment, and work engagement over time. The questionnaires with bereaved family members show that ACP conversations fluctuated over time and showed no significant changes.
In the interviews, DEDICATED ambassadors explained that they were enthusiastic about the DEDICATED approach. It raised awareness about timely conversations regarding care preferences as part of ACP and helped them to uncover a person’s life story and identify the needs of people with dementia and their families. Conducting personal, proactive conversations about the wishes and needs of people with dementia as part of ACP helped to build a more trusting care relationship. In turn, this supported palliative care provision according to the wishes and needs of people with dementia and their family caregivers. This could lead to greater autonomy and person-centered treatment for people with dementia [24]. A review by Raymond et al. (2014) described other interventions in which tools and training sessions were used to enhance the general knowledge about palliative care for people with dementia. Key differences between the DEDICATED approach and these other training programs were that the latter mostly aimed to enhance general knowledge about palliative care, while the DEDICATED approach focuses on specific topics and competencies needed to provide palliative care for people with dementia. Nevertheless, the training and tools mentioned in this review showed similar outcomes to those reported by DEDICATED ambassadors. For instance, the training-based interventions described in the review would lead one to conclude that participating HCPs learned new skills, such as identifying the readiness of people with dementia and family caregivers to discuss wishes and needs for end-of-life care. Additionally, HCPs emphasized quality of life rather than only focusing on clinical treatment during the provision of palliative care [53]. These findings are consistent with the experiences of DEDICATED ambassadors and support the assertion that training-based interventions like the DEDICATED approach can empower HCPs in their provision of palliative care for people with dementia. However, the adequacy of the implementation is a prerequisite for observing the impact of the DEDICATED approach in practice [32].
Questionnaires among care team members of the DEDICATED ambassadors showed no significant changes in self-efficacy, work engagement, and psychological empowerment over time. A first explanation for the absence of these changes could lie in the bottom-up implementation strategy of the DEDICATED approach. DEDICATED ambassadors formed the primary population of interest. They pursued the DEDICATED approach training program and were subsequently responsible for the stepwise implementation of the tools in practice. Additionally, they made the decisions about how to involve their team members in DEDICATED. A bottom-up strategy is adequate to ensure ownership and sustained usage of an intervention at different organizational levels [53, 54], but it can also be prone to complications with regard to involving other organizational layers, such as the different HCPs surrounding the DEDICATED ambassadors [55]. DEDICATED ambassadors explained a number of different implementation strategies they had deployed, such as giving presentations about the DEDICATED approach and using team meetings to discuss the program’s tools [32]. However, full implementation of an intervention (including all the tools that form part of the intervention) across various organizational layers can take considerable time and face substantial barriers. For instance, DEDICATED ambassadors explained that they needed more structure and training on how to implement the DEDICATED approach and that their team members might be reluctant to change their daily working routines [32]. These challenges may limit the impact of the DEDICATED approach, especially if the target population (i.e. team members) has not yet been effectively reached [56,57,58]. Our follow-up measurement could, therefore, have been conducted too early in the implementation process to detect any significant change. Moreover, if the DEDICATED approach was used only in specific situations rather than as part of team members’ daily routine, it might not have made an effective impact on individuals with dementia and their family caregivers. This could also explain the lack of reported increase in ACP conversations and in whether HCPs acted upon stated wishes and needs during palliative care provision. Other factors may have also influenced the implementation of the DEDICATED approach. The COVID-19 pandemic occurred between the baseline and follow-up measurements, which could have contributed to the finding of a decline in self-efficacy, work engagement, and psychological empowerment of HCPs in palliative care. The pandemic had a tremendous impact on care provision in nursing homes, including palliative and end-of-life care for people with dementia [38, 59]. The pandemic placed significant pressure on HCPs’ working lives and raised acute ethical dilemmas and levels of moral distress [60, 61]. A large-scale longitudinal study in the Netherlands showed that healthcare workers experienced deteriorating psychosocial working conditions, such as lower autonomy at work and greater psychological demands from their job [62]. Additionally, increased attention to palliative care and dementia could have heightened HCPs’ self-awareness, influencing their self-assessment regarding self-efficacy, work engagement, and psychological empowerment. The Dunning-Kruger effect describes how less skilled individuals may be unaware of their skill level and are therefore more likely to overestimate their abilities [63].
A second possible explanation for the limited extent of change found in the study relates to the compositional differences between the different experimental groups (i.e., test, design, and control groups) at both the baseline and follow-up measurement points. Specifically, the differences in the balance of occupations within the experimental groups might have influenced the outcome measures. For example, White et al. (2021) argued that HCPs in different roles often have varying perceptions of their skills and competencies. In their study, certified nursing assistants reported higher competence in communicating with clients compared to nurses, due to the extensive time they spend in direct contact [64]. This could have led to differing perceptions of self-efficacy, psychological empowerment, and work engagement compared to those with qualified nurse status. As the experimental groups in our study showed significant differences in group composition, this may have influenced their self-perceived scoring in terms of self-efficacy, work engagement, and psychological empowerment, possibly explaining our results. On the other hand, DEDICATED ambassadors themselves indicated having experienced greater work engagement while using the DEDICATED approach. This also underscores the need for longer-term usage or further development of validated scales to analyze the underlying skills and competencies that the DEDICATED approach aims to enhance in the field of palliative care for people with dementia, as the current scales may not fully explore the factors that underlie limited or improved self-efficacy, psychological empowerment, and work engagement in the field of palliative care.
The results from bereaved family caregivers indicated that the frequency of ACP conversations fluctuated over time and showed no significant increase. Many countries, including the Netherlands, have initiated national campaigns to raise awareness about what palliative care entails, and of the role of proactive conversations about the wishes and needs of a care recipient as crucial aspects of palliative care [65, 66]. This could also contribute to a growing emphasis on palliative care and ACP discussions. Furthermore, the COVID-19 pandemic may have prompted family members and HCPs to proactively discuss future (palliative) care needs with frail older persons [59]. This could have contributed to an overall increase in such conversations with family caregivers, making it difficult to assess the impact of the DEDICATED approach on this matter.
Palliative care provided to people with dementia was also assessed using the EOLD scales. During the research period, the EOLD scores showed no significant increase over time. Other research examining trends in EOLD scores over time, which also incorporated EOLD data from the DEDICATED project, found EOLD-SWC scores to have significantly increased, while total scores for EOLD-CAD showed no significant improvement, with a small decline in the “Wellbeing” subscale [67]. However, in the study by Klapwijk et al. (2021), the mean total score for EOLD-SWC was 32.7, while in our study, the mean total score was 28.1 for the test/design group and 28.4 for the control group. Other research regarding the EOLD-SM scores for people with dementia in nursing homes found a mean score of 28.7 [68], while in our study, the mean score was 25.7. The difference in scores might explain several needs of the bereaved family caregivers for enhancing nursing practice and policy. The relatively lower EOLD scores observed in our study might be caused by the fact that part of our data were collected during periods of restricted access for family because of the COVID-19 pandemic. There is a need to explore the underlying reasons for lower perceived quality of care. A qualitative study regarding the experiences of bereaved family caregivers with the provided end-of-life care might explain aspects of importance for family caregivers in end-of-life care, such as information provision caregiver expectations. This knowledge is needed to improve daily practice and inform policy.
There are several limitations to consider when interpreting the research results. First, interviews with DEDICATED ambassadors were conducted by members of the research team, possibly eliciting socially desirable or only positive responses. While these interviews offered valuable insights into the perceived impact of the DEDICATED approach, the small sample size limits generalizability. The quantitative studies included large amounts of participants and data. However, these too contain several limitations. For the questionnaires among team members, the PCSES and PE-scale were translated into Dutch using a forward-backward method. Cronbach’s α was 0.95 for the PCSES and 0.88 for the PE-scale, indicating a level of validity and reliability of the questionnaire of this study component [69]. However, the absence of broader psychometric evaluation might hamper the interpretation of our results.
Thirdly, the study among team members used a longitudinal design with baseline and follow-up measurements. High staff turnover led to differences in team composition over time, making it impossible to analyze the same individuals across both points and weakening the validity. Table 2 illustrates these changes. Additionally, many responses were incomplete due to participants not specifying their healthcare organization, making group assignment difficult and reducing usable data. Future research should aim to track individuals across measurements to reduce bias and improve analyses [70]. In addition, future research related to this topic, should collect more information on the background of the person with dementia. In this study, limited information was gathered regarding the profile of the people with dementia that the healthcare professionals worked with. For example, disease severity or communicational abilities may have influenced HCP’s perceived self-efficacy, psychological empowerment and work engagement. Adjusting for this information might have yielded different results in our regression analysis.
Finally, EOLD data were based on proxy responses from bereaved family caregivers, who may have had limited interaction with the person with dementia, especially during the COVID-19 pandemic. This could have influenced their evaluation of the quality of palliative care provided. Other factors, such as disease severity, symptoms, staff behavior may have also likely influenced their evaluations [71, 72]. As this was an exploratory study, such confounders were not accounted for. Further research could include these possible confounding variables in the data analysis and use multilevel regression and adjusted logistic regressions to show effects over time. Due to the small categorical answer sizes, the logistic regression analysis for the ACP data might have caused our outcomes to be non-significant.
In conclusion, the DEDICATED approach was considered valuable by the DEDICATED ambassadors, as it supports HCPs in delivering person-centered palliative care. It increased awareness about the importance of timely care preference discussions as part of ACP and helped uncover a person’s life story. However, no significant changes in perceived self-efficacy, psychological empowerment, or work engagement were observed among the care team members. ACP conversations varied over time, making it difficult to assess the impact of the DEDICATED approach, as many factors could have influenced these results. Further research using a longitudinal design will assess the effects of the DEDICATED approach, with follow-up measurements that can better explain its impact on palliative care for people with dementia.
The datasets used and/or analyzed during the current study are available from the corresponding author on (justified) request.
- ACP:
-
Advance care planning
- AWO:
-
L–Living Lab in Aging and Long–Term Care
- ANOVA:
-
Analysis of Variance
- CCA:
-
Conventional Content Analysis
- DEDICATED:
-
Desired Dementia Care Towards End of Life
- EOLD:
-
CAD–End of Life in Dementia Comfort Assessment in Dying
- EOLD:
-
SM–End of Life in Dementia Symptom Management
- EOLD:
-
SWC–End of Life in Dementia Satisfaction with Care
- HCP:
-
Healthcare professional
- METC:
-
Z–Medical Ethics Committee of Zuyderland Medical Centre
- OR:
-
Odds ratio
- PCSES:
-
Palliative Care Self–Efficacy Scale
- PE:
-
Psychological Empowerment
- SPSS:
-
Statistical Package for the Social Sciences
- UWES:
-
Utrecht Work Engagement Scale
We are grateful to Mrs. Sanne P.C.M. Vergouwen for her assistance in carefully checking the quantitative data related to the questionnaires used in this study.
This research was funded by The Netherlands Organization for Health Research and Development (ZonMw, grant number 10200012110004). ZonMw had no role or influence in the conduct of the research or its findings.
Ethical approval for the development and implementation of the DEDICATED approach and for collecting data from bereaved family caregivers was obtained from the Medical Ethics Committee of Zuyderland Medical Centre (METC Z), respectively METCZ20190095 and METCZ20180026, prior to the commencement of data collection. All involved HCPs and bereaved family members provided either written or verbal informed consent to participate in this study. This research adhered to the principles of the Declaration of Helsinki.
Not applicable.
The authors declare no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Biesmans, J.M., Bolt, S.R., Hameleers, N. et al. Impact of the DEDICATED approach to optimizing palliative care for people with dementia: a multi-method study. BMC Health Serv Res 25, 882 (2025). https://doi.org/10.1186/s12913-025-13063-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-025-13063-3