BMC Pregnancy and Childbirth volume 25, Article number: 680 (2025) Cite this article
Maternal hypertensive disorders (MHD) are a leading cause of maternal and fetal mortality, with profound short- and long-term public health impacts. MHD epidemiology remains poorly controlled, and the incidence rate has shown an increase over the past few decades. Therefore, a comprehensive assessment of global burden and prevalence inequalities holds considerable significance for optimizing public health strategies.
The global burden and epidemic trend of MHD from 1990 to 2021 were investigated, and the incidence, prevalence, mortality, and disability-adjusted life years (DALYs) were examined utilizing the Global Burden of Disease (GBD). The trends were stratified by age and socio-demographic index (SDI), and further analysis was performed to delve into the correlation between SDI and incidence, prevalence, mortality, and DALYs. Additionally, a Bayesian Age-Period Cohort (BAPC) model was constructed to predict the burden of disease in MHD from 2022 to 2046.
The DALYs induced by MHD decreased significantly from 3.48 million (95% UI, 3.09–3.87 million) in 1990 to 2.47 million (95% UI, 2.08–2.96 million) in 2021, involving an Excess Annual Percentage Change (EAPC) of -2.10. Both the age-standardized DALYs rate (ASDR, AAPC = -2.11) and the age-standardized incidence rate (ASIR, AAPC = -0.60) exhibited evident decreasing trends. The ASDRs of all the age-stratified subgroups decreased as well. Notably, the largest declines were observed in the 20–24 age group with an EAPC of -2.39 (95% UI: -2.56, -2.23). The ASIR exhibited an obvious negative correlation with SDI, and the inequality tended to shrink. Projections for 2046 indicate that global ASDR and ASIR are expected to sustain their downward trajectory. Globally, ASDR in MHD linked to iron deficiency decreased significantly (EAPC = -2.03), with High-middle SDI countries experiencing particularly steep reductions (EAPC = -4.25).
This study performed a comprehensive analysis of the global burden of MHD and observed regional and national inequalities. The investigation also identified a correlation between MHD and SDI, and most regions exhibited an overall declining trend in disease burden. However, further investigations should still be conducted to assist the establishment of public health strategies for MHD prevention.
Maternal hypertensive disorders (MHD) are a critical unresolved challenge in perinatal medicine, encompassing a spectrum of common pregnancy complications, including chronic hypertension, gestational hypertension, preeclampsia/eclampsia, and chronic hypertension complicated with preeclampsia/eclampsia [1, 2]. Despite the identification of distinct MHD subtypes, an international consensus on their classification remains elusive. The high prevalence of MHD is associated with increased maternal and fetal morbidity and mortality and exerts a considerable threat to the public health [3, 4]. Furthermore, substantial evidence has demonstrated the long-term impacts of MHD on the cardiovascular system, endocrine, and metabolic systems, as well as its associations with various diseases in women and their offspring [1, 5, 6]. Despite growing recognition of the detrimental impacts of MHD, their epidemiology has not been effectively controlled. Data over recent decades show that MHD affects approximately 10% of pregnancies, with incidence rates demonstrating a significant upward trend [7].
Besides, the inequality of MHD prevalence across different ages, regions, and seasons has also been frequently described [8]. However, up to date, efficient diagnostic markers or methods for the prediction of MHD are still lacking. Meanwhile, risk factors contributing to the occurrence of MHD are complex and sometimes unmodifiable, further complicating disease treatment and prevention. Therefore, a comprehensive assessment of the global burden of disease, a prediction of the epidemiological dynamics, and an analysis of the inequality are all imperative, which will benefit the evaluation and establishment of public health strategies and facilitate the optimization of resource allocation.
Herein, the research was carried out to investigate the global burden and the epidemic developmental trend of MHD from 1990 to 2021. The incidence, prevalence, mortality, and disability-adjusted life years (DALYs) were examined utilizing the Global Burden of Disease (GBD). The trends were stratified by age and socio-demographic index (SDI), and further analysis was performed to study the correlation between SDI and incidence, prevalence, mortality, and DALYs, revealing the inequality of MHD burden between countries and regions across diverse economical developmental levels.
The GBD 2021 study serves as a publicly accessible epidemiological database. Leveraging updated data resources and refined statistical methodologies, it provides a comprehensive assessment of health outcomes attributable to 371 diseases/injuries and 87 risk factors across 204 countries and territories globally from 1990 to 2021 [1,2,3].
This study performed a descriptive epidemiological analysis based on the DALYs and incidence data for MHD across different age groups from 15 to 54 years old. The data were sourced from the GBD 2021 repository constructed by the Institute for Health Metrics and Evaluation (IHME, 2024) (https://vizhub.healthdata.org/gbd-results/). Specifically, data across multiple dimensions, including age, year, and geographical location (covering five levels of SDI, 21 GBD regions, and 195 countries) were compared to evaluate the global burden of MHD in 2021, its trends from 1990 to 2021, and projections up to 2046. According to the inherent characteristics of the GBD database, the 95% uncertainty interval (UI) for each indicator was determined by the 2.5th and 97.5th percentiles of the posterior distribution obtained from 1000 samples [1]. Notably, this study utilized publicly accessible resources, making it unnecessary to obtain any additional ethical review approval.
MHD
In the GBD 2021 study, the definition of MHD follows the Tenth Revision of the International Classification of Diseases (ICD-10) code O10-O16 (https:ghdx.healthdata.org/record/ihme-data/gbd-2021-cause-icd-code-mapping). This classification encompasses the following key subtypes: the original hypertension complicated by pregnancy, childbirth and the puerperium, chronic hypertension with preeclampsia, gestational hypertension, gestational hypertension complicated by preeclampsia and eclampsia, and unspecified maternal hypertension (https://icd.who.int/browse10/2019/en#/O10-O16). Hypertension during pregnancy is defined as systolic blood pressure≧140 mmHg and/or diastolic blood pressure≧90 mmHg [6]. Notably, while the GBD 2021 study continues to use the term "MHD" (maternal hypertensive disorder) to describe conditions associated with hypertension during pregnancy, the more popular term is "hypertensive disorder of pregnancy (HDP)" [4].
DALYs
DALYs represent an indicator used to measure the lethality and burden of diseases. Specifically, DALYs indicate the sum of Years of Life Lost (YLLs) due to premature mortality caused by diseases and Years Lived with Disability (YLDs) resulting from disability [7], i.e., DALYs = YLLs + YLDs. When combined with other inequality indicators, DALYs can provide a more comprehensive and effective assessment of the relationship between MHD (presumably referring to a specific disease or health condition, such as Mental Health Disorders, yet necessitating context-specific clarification) and health inequalities.
SDI
SDI is a comprehensive indicator reflecting the level of social development across different countries and regions. It is derived from a comprehensive assessment based on three key data points: the total fertility rate among women under 25 years old, the average educational attainment of women aged 15 and above, and per capita income [1]. According to the SDI values, the GBD 2021 categorizes 204 countries or regions into five distinct levels: High-SDI regions (such as Australia, Canada, France, etc.), High-middle SDI regions (such as China, Argentina, Belarus, Chile, etc.), Middle-SDI regions (such as Albania, Brazil, etc.), Low-middle SDI regions (such as Angola, Bangladesh, Cameroon, etc.), and Low-SDI regions (such as Afghanistan, Benin, Haiti, etc.). A higher SDI value indicates a higher level of social development in the region.
Age-standardized rate (ASR)
ASR is adjusted based on the rates of a specific age structure. It is commonly used to compare data from different populations or time points to eliminate the impact of differences in the age structure [8]. Herein, the world population age standards described in GBD 2021 were adopted as a reference to calculate the age-standardized incidence rate (ASIR) and age-standardized DALYs rate (ASDR) per 100,000 population across the all-age group. A stratified analysis of age (15–54 years) and SDI was then performed to explore trends in specific ages and regions.
Estimated Annual Percentage Change (EAPC)
EAPC is an indicator used to measure the trend of an indicator (such as incidence) over a certain timeframe. The specific calculation method is as follows: First, collect data on the research index over multiple years; then, logarithmically transform the original index values to better align the data with the linear model's assumptions; finally, perform linear regression analysis between the year and the logarithmically transformed index. The single slope assumption of the EAPC makes it better suited for assessing long-term trends. In contrast, the average annual percent change (AAPC) is calculated as a weighted average of annual changes over a segmental period, making it appropriate for describing annual changes at different stages in a long-term trend, particularly useful for non-linear or fluctuating trends. The formula is as follows:
$$\mathrm{EAPC}=\left(\exp^{\mathrm\beta}-1\right)\times100\%$$
where β denotes the slope coefficient from the regression of natural log-transformed rates against time.
This study compared the ASIR and ASDR across multiple dimensions, including age, year, and geographical location (covering five levels of the SDI, 21 GBD regions, and 195 countries). The Joinpoint regression model was employed to calculate the Annual Percent Change (APC) and AAPC for MHD, aiming to assess the global burden of disease and trends in MHD from 1990 to 2021.
The primary objective of the health inequality analysis w to uncover the unequal distribution of disease burden globally, which is influenced by various factors such as socioeconomic status, education level, and allocation of medical resources. Specifically, the Slope Index of Inequality (SII) and Concentration Index (CI) were utilized as assessment tools to measure absolute and relative inequalities in disease burden, respectively [9]. SII was calculated by sorting a weighted sample of the entire population by SDI and then performing a regression analysis based on the midpoint value. Conversely, CI was determined by matching the cumulative proportion of DALYS with the cumulative population distribution ranked by SDI and numerically integrating the area under the Lorentz curve [10].
Simultaneously, frontier analysis was conducted to assess the MHD disease burden in different countries or regions relative to their ideal or optimal performance based on their SDI. This analysis aimed to reveal the optimal level of disease burden control that each country or region could achieve at a specific stage of development. Locally Weighted Scatterplot Smoothing (LOESS) was employed to determine the frontier line. Subsequently, the absolute distance between each country's actual disease burden and the frontier line (i.e., the efficiency gap) was calculated, which reflected the country's deviation from optimal performance in disease prevention and control.
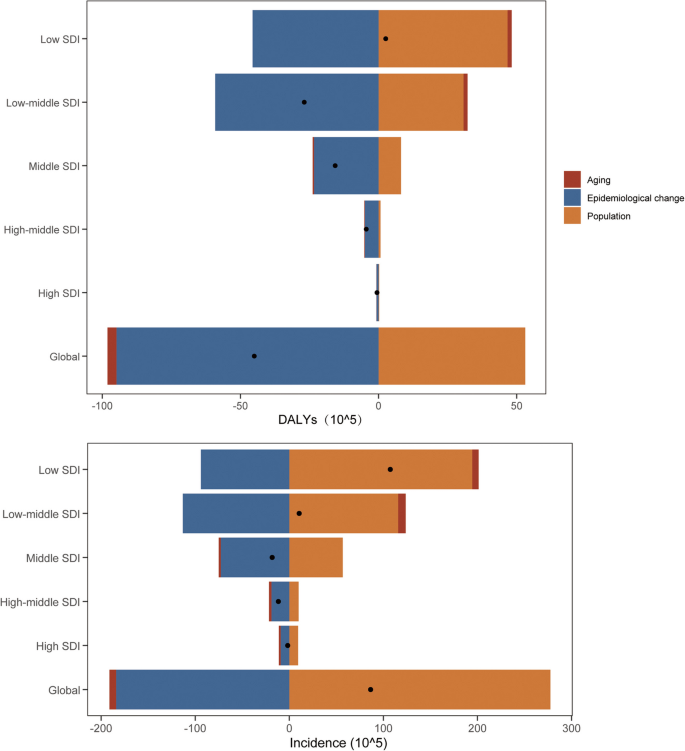
Furthermore, decomposition analysis was performed to explore the relationship between the MHD disease burden and three key determinants of sociodemographic development, namely aging, epidemiological shifts, and population size, spanning from 1990 to 2021. Decomposition analysis, as an innovative statistical tool, effectively dissected the overall changes in contributions from individual key factors. Delving into the contributions and evolutionary trends of these factors offered novel insights into the underlying causes of changes in the MHD disease burden.
Lastly, the Bayesian Age-Period-Cohort (BAPC) model was employed to predict the ASDR and ASIR of MHD up to 2046. While the BAPC model was originally designed for the prediction of cancer epidemiology [11], its hierarchical Bayesian framework for APC effects has been successfully extended to trend analysis for non-cancer diseases. The BAPC model was hereby selected for the following reasons: Firstly, the incidence of MHD was influenced by the interaction of three factors, namely age (such as physiological changes during childbearing years), period (such as prenatal care policy implementation), and cohort (such as intergenerational differences in childbearing delay). The BAPC model could capture this complex effect through random walk (RW) smoothing fitting and piecewise linear trend modeling. Concurrently, it could also combine prior information regarding unknown parameters with sample information to obtain a posterior distribution from which the unknown parameters could be inferred [12]. Secondly, the effectiveness of BAPC model in predicting non-cancer diseases such as diabetes, respiratory infection, and cirrhosis had been verified [13,14,15]. Compared to other methods, the BAPC model presented clear advantages in managing sparse data, providing estimates of uncertainty, and addressing homogeneity and complexity. Therefore, the flexibility of the BAPC model was adapted to the data structures in this study.
GBD 2021 data were also used to systematically assess risk factors associated with the burden of MHD. By comparing risk assessment models, population attribution scores (PAFs) for nutrition-related determinants were quantified, with particular emphasis on iron deficiency. The analytical framework integrated DisMod-MR 2.1 and Bayesian meta-regression tools to estimate exposure distributions and theoretical minimum risk exposure levels. Previous studies detailed specific estimates of the disease burden arising from risk factors [16]. All analyses and figures were hereby conducted using R software (version 4.4.2), with a P-value < 0.05 considered statistically significant.
From 1990 to 2021, the global DALYs due to MHD significantly decreased from 3.48 million (95% UI, 3.0859–3.8732 million) to 2.47 million (95% UI, 2.0834–2.9582 million). Consistently, the ASDR declined from 123.15 per 100,000 population in 1990 to 63.47 per 100,000 population in 2021. However, notably, despite a decrease in the ASIR (1990: 554.35 per 100,000 population versus 2021: 461.94 per 100,000 population), the actual number of incident cases increased from 15.663 million (95% UI, 12.935–19.255 million) in 1990 to 18.05 million (95% UI, 15.356–21.519 million) in 2021 (Tables 1 and 2, Figure S1).
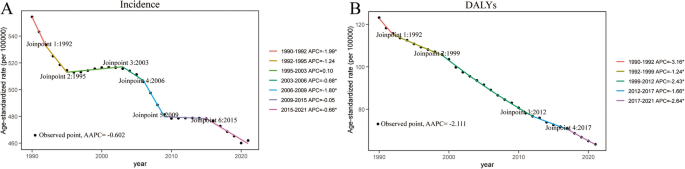
Joinpoint regression analysis revealed that between 1990 and 2021, both the ASDR (AAPC = -2.111%) and ASIR (AAPC = -0.602%) of MHD showed significant downward trends. The period from 1990 to 1992 witnessed the most significant declines in ASIR (APC = -1.99%) and ASDR (APC = -3.16%) (Fig. 1, Table 3).
Joinpoint regression analysis of total burden related to MHD from 1990 to 2021 at the global level. MHD maternal hypertensive disorder, APC annual percentage change, AAPC average annual percentage change, DALYs disability-adjusted life-years
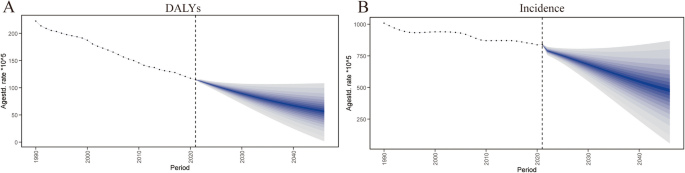
Furthermore, predictions using the BAPC model for the MHD disease burden from 2022 to 2046 indicate that the global ASDR and ASIR are expected to continue their downward trends. Specifically, by 2046, the ASDR for all age groups is projected to decline to 54.87 per 100,000 population, while the ASIR is expected to fall to 463.23 per 100,000 population (Fig. 2, Table S1).
Projected results of MHD disease burden from 2022 to 2046. A Age-standardized DALYs rate. B Age-standardized incidence rate. MHD maternal hypertensive disorder, DALYs disability-adjusted life-years
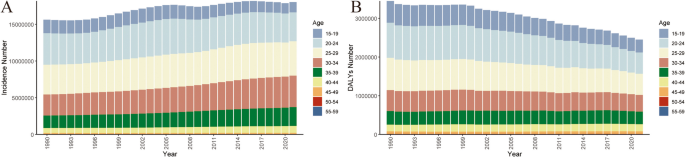
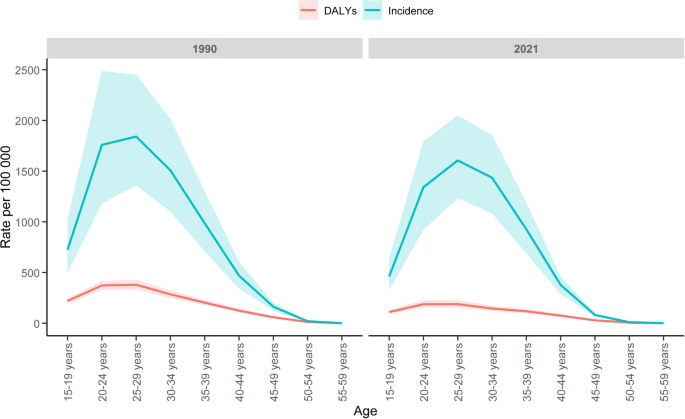
Compared to 1990, the ASDR for all age subgroups of MHD decreased globally. Notably, the 20–24 age group showed the largest decline with an EAPC of -2.39 (95% UI: -2.56, -2.23), while the 50–54 age group exhibited an EAPC of -2.39 (95% UI: -2.54, -2.24). In 2021, the peak ASDR for MHD globally was found in the 25–29 age subgroup (187.73 per 100,000 population), while the 20–24 age subgroup had the highest number of DALYs at 549,100 cases (95% UI: 456,300–657,500) (Table 1, Figs. 3, 4). Meanwhile, the ASIR decreased across all age groups as well, with the most significant decline in the 50–54 age group, involving an EAPC of -2.19 (95% UI: -2.35, -2.03). However, it should be particularly noted that despite the overall decline in ASIR, the incidence among populations aged 30 and above showed an upward trend, possibly attributed to population growth and aging. In 2021, the peak ASIR for MHD globally was also observed in the 25–29 age subgroup (1605.08 per 100,000 population). This subgroup also had the highest number of incident cases, totaling 46,705,700 (95% UI: 35,849,800–59,616,800) (Table 2, Figs. 3, 4).
Total burden incidence and DALYs associated with MHD, by age group, worldwide from 1990 to 2021 (A) Age-standardized incidence rate; (B) Age-standardized DALYs rate. MHD maternal hypertensive disorder, DALYs disability-adjusted life-years
Global trends in the total burden associated with MHD by age between 1990 and 2021. MHD maternal hypertensive disorder, DALYs disability-adjusted life-years
From 1990 to 2021, the ASDR or MHD decreased in all five SDI regions. Notably, the decline was most significant in High-middle SDI countries, with an AAPC of -4.37% (95% UI: -4.42 to -4.32). In contrast, the slowest decline was observed in High-SDI countries, with an AAPC of -1.74% (95% UI: -1.81 to -1.67) (Table 3). In 2021, the ASDR in Low-SDI regions was the highest (210.89 per 100,000 population), approximately 50 times that in High-SDI regions (4.18 per 100,000 population) (Table 1), which accounted for half of the total global cases.
Meanwhile, the ASIR also showed a downward trend across all SDI subgroups. Among them, Low-middle SDI regions experienced the fastest decline, with an AAPC of -1.68% (95% UI: -1.73 to -1.64), whereas High-SDI regions had the slowest decline, involving an AAPC of -0.30% (95% UI: -0.34 to -0.26) (Table 3). By 2021, the ASIR in Low-SDI regions remained the highest (1202.32 per 100,000 population), approximately six times that in High-middle SDI regions (207.21 per 100,000 population) (Table 2). Obviously, substantial disparities existed across countries with varying different SDI levels: Low-SDI countries reported significantly higher ASIR and ASDR compared to High-SDI countries. Targeted efforts and increased investments should therefore be ensured to advance health outcomes in these regions.
In 2021, among the 21 GBD regions, Central Sub-Saharan Africa had the highest ASDR at 255.22 per 100,000 population. Conversely, High-income Asia Pacific had the lowest ASDR at 1.90 per 100,000 population (Table 1). Joinpoint regression analysis revealed that from 1990 to 2021, with the exception of the Caribbean (AAPC = 0.18%; 95%UI: 0.06 to 0.28), which exhibited a slight upward trend, the ASDR in the remaining 20 GBD regions showed significant downward trends. Among these, East Asia witnessed the fastest decline with an AAPC of -5.55% (95%UI: -5.65 to -5.47), whereas High-income North America exhibited the slowest decline with an AAPC of -0.55% (95%UI: -0.64 to -0.47). Simultaneously, Eastern Europe (AAPC = 0.11%) and Western Europe (AAPC = 0.30%) showed slight upward trends in their ASIR. In contrast, South Asia had the fastest decline in ASIR with an AAPC of -2.43% (95%UI: -2.50 to -2.38) (Table 3). In 2021, Western Sub-Saharan Africa presented the highest ASIR at 1678.15 per 100,000 population, while East Asia had the lowest ASIR at 108.74 per 100,000 population (Table 2).
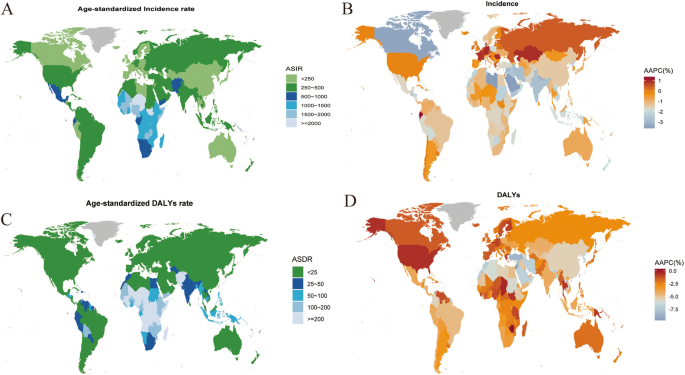
In 2021, Niger recorded the highest ASIR globally (2175.7 per 100,000 population), while South Sudan had the highest ASDR (428.07 per 100,000 population). In contrast, the Republic of Korea reported the lowest both in terms of ASIR (34.99 per 100,000 population) and ASDR (0.92 per 100,000 population) (Table S2, Fig. 5A, C). Between 1990 and 2021, the ASIR declined in most countries and regions, with 23 exceptions including Georgia, Kazakhstan, Monaco, Palau, and San Marino. Among them, Libya recorded the largest decline (AAPC = -3.64%), followed by Saudi Arabia (AAPC = -3.61%) and Canada (AAPC = -3.48%). Conversely, Ecuador witnessed the highest increase in ASIR (AAPC = 1.35%). Meanwhile, the ASDR declined significantly in most countries, with the exception of the Caribbean and Zimbabwe, where upward trends were observed. Jordan experienced the greatest decline in ASDR (AAPC = -9.69%), followed by Türkiye (AAPC = -8.48%) (Table S3, Fig. 5B, D).
Age-standardized rate of total burden related to MHD in 204 countries and territories (A) Age-standardized incidence rate in 2021; (B) AAPC in age-standardized incidence from 1990 to 2021; (C) Age-standardized DALYs rate in 2021; (D) AAPC in age-standardized DALYs from 1990 to 2021. DALYs disability-adjusted life-years, ASIR age-standardized incidence rate, ASDR age-standardized DALYs rate, AAPC average annual percentage change
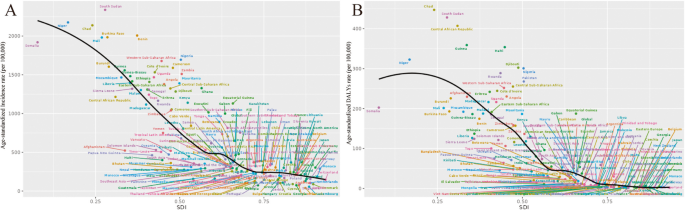
An in-depth analysis was conducted on the relationship between ASIR, ASDR, and SDI across 204 countries and regions. Globally, there was a notable negative correlation between ASIR and SDI. Specifically, in 2021, regions with higher MHD incidence rates were concentrated in Low- and Middle-SDI areas, while incidence rates remained relatively stable in High-SDI areas without pronounced changes. South Sudan, despite being categorized as Low-middle SDI, had the highest ASIR, significantly exceeding most other countries. Similarly, a negative correlation existed between ASDR and SDI, with ASDR peaks predominantly observed in Middle-SDI areas, while High-SDI areas exhibited stabilization. In particular, despite Chad's low SDI level, it recorded the highest ASDR value (Fig. 6).
Global, regional, and national levels of total burden related to MHD by SDI (A) Age-standardized incidence in 2021 in 204 countries and territories; (B) Age-standardized DALYs in 2021 in 204 countries and territories. SDI socio-demographic index, DALYs disability-adjusted life-years
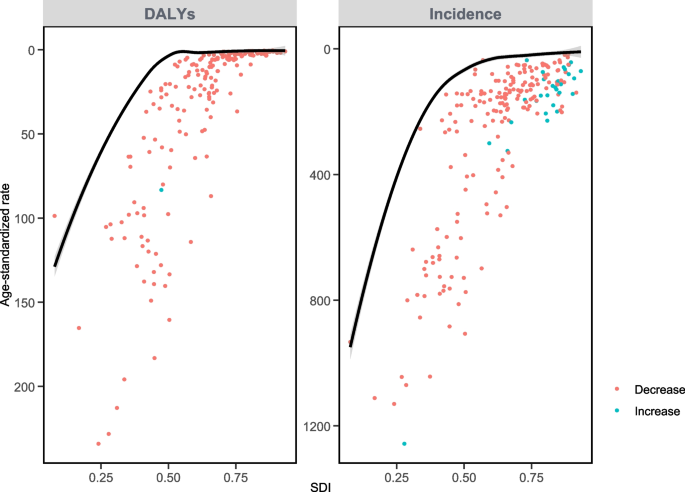
Frontier analysis results showed that in terms of ASIR in 2021, the five countries with the largest effective difference from the frontier line were South Sudan, Benin, Nigeria, Chad, and Burkina Faso, indicating significant room for improvement in Low or Low-middle SDI areas. Notably, some countries with relatively higher SDI, such as Ghana, Equatorial Guinea, and Zambia, also had large effective differences in MHD prevention and control, necessitating further improvement (Table S4, Fig. 7, Figure S2). On the other hand, the five countries with the largest effective differences in ASDR were Haiti, the Central African Republic, South Sudan, Djibouti, and Nigeria. As shown in Fig. 7, with socio-economic development, the effective differences between regions generally showed a decreasing trend. However, those with larger differences were mostly concentrated in Middle-SDI areas, suggesting the necessity of constant endeavors for Middle-SDI areas to reduce DALYs (Table S5, Fig. 7, Figure S2).
Frontier analysis exploring the relationship between SDI and ASR for MHD in 204 countries and territories. DALYs disability-adjusted life-years
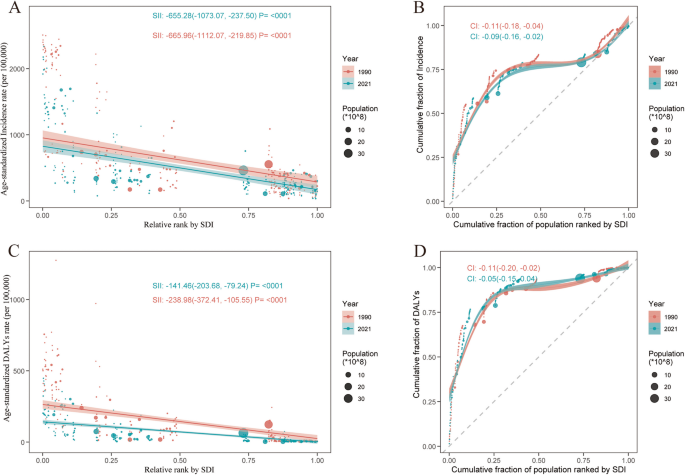
Analysis of health inequality uncovered significant absolute and relative inequalities between ASIR, ASDR, and SDI. In terms of ASIR, the SII in 2021 was -655.28 (95% CI: -1073.07 to -237.50), and the CI was -0.09 (95% CI: -0.16 to -0.02), indicating that countries with lower SDI bore a higher disease burden. Despite decreased inequality compared to 1990, the magnitude of improvement was relatively small. Meanwhile, the SII for ASDR decreased from -238.98 (95% CI: -372.41 to -105.55) in 1990 to -141.46 (95% CI: -203.68 to -79.24) in 2021. Consistently, the CI also declined from -0.11 (95% CI: -0.20 to -0.02) in 1990 to -0.05 (95% CI: -0.15 to -0.04) in 2021 (Fig. 8). These results indicated that while disparities in disease burden persisted across countries with varying levels of economic development, there was a trend toward improvement in this inequality.
Health inequality regression curves and concentration curves for the ASR of MHD worldwide, 1990 and 2021. The graph on the left illustrate the slope index of inequality, depicting the relationship between SDI and ASR for each condition, with points representing individual countries and territories sized by population. The graph on the right present the concentration index. SII slope index of inequality, SDI socio-demographic index, DALYs disability-adjusted life-years
This study conducted a decomposition analysis of the disease burden of MHD from 1990 to 2021 to explore the varying contributions of aging, epidemiological changes, and population growth. The results showed that globally and across the five SDI regions, MHD-attributed DALYs decreased in all regions except the Low-SDI countries, with the largest decline observed in Low-middle SDI countries (Fig. 9). Globally, population growth contributed to an increase in the number of DALYs (118.08%), while epidemiological changes were the primary factor leading to a significant reduction in DALYs (-210.84%), and aging had a slight negative impact (-7.24%). Notably, epidemiological changes contributed the most in Low-SDI countries (-1752.76%). However, in terms of MHD incidence, despite the role of epidemiological changes in reducing incidence (-212.89%), a substantial increase in population (321.13%) led to an upward trend in global incidence. This impact of population growth on incidence was most evident in the Low-middle SDI regions (1099.78%) (Table S6). In summary, this study revealed the trends in the MHD disease burden across different SDI regions and the driving factors behind these trends, providing important references for formulating targeted public health policies and interventions.
Population-level determinant changes in aging, population growth, and epidemiological changes for MHD globally and in various SDI regions from 1990 to 2021
From 1990 to 2021, the global MHD ASDR attributed to iron deficiency declined from 21.56 (95% UI 10.32 to 28.79) per 100,000 population to 11.38 (95% UI 5.46 to 16.19). The reduction in iron deficiency was the most significant in High-middle SDI countries (EAPC = -4.25), while High-SDI countries reported the smallest burden of MHD due to iron deficiency in 2021 (0.67 per 100,000 population). Unfortunately, limited data on other risk factors for MHD in GBD studies hindered the assessment of MHD risks (Table 4).
As one of the leading causes of maternal mortality, MHD is considered a knotty issue in perinatal medicine, and epidemiological evaluation of MHD is increasingly highlighted [17]. This study analyzed the trends of MHD incidence and mortality at the global, regional and national levels from 1990 to 2021. The results revealed that the incident rate of MHD kept decreasing, possibly attributed to the optimized healthcare during pregnancy, including the improvement of prenatal examinations, clinical intervention, public health education, and personal lifestyle [18]. Nevertheless, the total number of incident cases increased, which was probably correlated with the population expansion and aging worldwide. Notably, the age group over thirty showed increased number of incident cases, probably attributed to the delay of maternal age and the rising number of pregnant women over thirty. Furthermore, the decreasing trends of ASDR possibly resulted from the increasing attention to MHD and advances in clinical intervention.
To our knowledge, studies comprehensively evaluating the epidemic situation of MHD remain limited. Wang et al. analyzed the global, regional, and national incidence and inequality of distribution from 1990 to 2019 [7]. As an expansion, the present research investigated the epidemic status from 1990 to 2021, further analyzed the epidemiological dynamics of MHD, and performed a corresponding prediction utilizing BAPC modeling. The results suggested a decreasing tendency from 2022 to 2026, indicating the effect of current strategies for the prevention of MHD, including close monitoring and prompt treatment.
Risk factors for MHD include modifiable factors (e.g., smoking, anemia, BMI, alcohol intake) and nonmodifiable factors (e.g., maternal age, primiparity, genetic variations), as partially summarized by Umesawa and Kobashi [19]. Nevertheless, these risk factors can merely predict 20–30% of cases and may induce a high false-positive rate. Maternal age is a representative factor influencing the risk of hypertension disorders of pregnancy (HDP), with the associations described in different investigations. Specifically, the cohort study (N = 100,949) performed by Uchinuma, H., Tsuchiya, K., Horiuchi, S. et al. [20] using data from the Japan Environment and Children’s Study stratified patients according to their age, and found that the group of advanced maternal age (≥ 35) had a 30% higher risk of HDP compared to the group of < 35, despite comparable blood pressure between these two groups; in the investigation of Liu et al. [21], the risks of chronic hypertension and pregnancy-induced hypertension increased gradually with maternal age in the group of ≥ 35.
Moreover, teenage pregnancy is also accompanied with higher risk of HDP, which may be related with lack of income or financial support, poor nutrition, and insufficient healthcare knowledge due to the low educational level. Thus, it is advisable to establish diagnostic criteria and public health strategies according to the age of pregnancy. The present study showed that the ASIR and ASDR of MHD of all the age groups experienced a significant decline. However, as mentioned above, the total incident cases of age ≥ 30 increased. Indeed, while population expansion and aging over recent decades may partially explain the phenomenon, another plausible explanation could be the increasing pressures faced by this age group, which constitutes the primary demographic adapting to significant social changes to support their families. Consequently, women at the age group of ≥ 30 are more likely to suffer sub-health due to overwork, and furthermore become vulnerable to mood disorders due to mental pressure. To be noteworthy, psychological health during pregnancy is demonstrated to be associated with MHD incidence. Previous studies suggested that pregnant women with anxiety were at increased risk of pregnancy hypertension, indicating the important roles of emotional regulation and psychological intervention during pregnancy [22]. Therefore, the increasing incident cases of MHD at age ≥ 30 may result from the mental pressure and anxiety induced by social development. Additionally, a great number of women at age ≥ 30 should be multiparous, and as the delay of childbearing age, the ratio of multiparous/ primiparous should be changed in this age group. However, the present study did not differentiate between multiparous and primiparous individuals, precluding an analysis of the correlation between increased incident cases and changes in the multiparous/primiparous ratio within this age group.
Previous studies suggested the correlation between family poverty and the mortality of MHD [23]. In this study, a significant negative correlation was observed between ASIR, ASDR, and SDI at both regional and national levels, underscoring the significance of economy in gestational health care. Several risk factors of MHD reviewed by M Umesawa and G Kobashi [19] are closely related with family economic situation. For example, family financial status may directly influence their diet and lifestyle while exerting an impact on the nutritional status of pregnant women, further influencing BMI, the occurrence of anemia and metabolic disease, and, consequently, the risk of MHD. Therefore, improvement of family income driven by the dramatic global economic changes during the past decades may have led to the decreased incident rate of MHD. Besides, enhancement in women’s education and labor market participation, independent financial status, value changes, and gender equity also promote the advancement of women status, encouraging more women to be more self-decisive. As a consequence, more women may choose to bear children at appropriate reproductive age, and the insurance of women’s rights provide pregnant women with better psychological status, thereby contributing to reducing the incident rate of MHD. Moreover, both social advancement and family income improvement facilitate women to acquire better clinical and psychological services during pregnancy. Therefore, adequate financial insurance and maternal psychological healthcare deserves to be highlighted in MHD prevention.
The observation that the MHD incidence is the highest in the 25–29 age group, rather than among very young or advanced maternal age groups, indeed contradicts the commonly understood epidemiological pattern. While advanced maternal age (≥ 35 years) and teenage pregnancy are extensively recognized as high-risk periods for HDP, emerging evidence suggests that the 25–29 age group may also exhibit elevated risks due to unique demographic and lifestyle factors. Women in this age group may experience heightened occupational and social stress during early career and family formation stages, thus increasing HDP risks [24]. In some high-income countries, delayed childbearing has shifted the peak incidence to older ages (≥ 30), while in low- and middle-income regions, the 25–29 age group remains the most common childbearing window [2]. This age group accounts for the largest share of pregnancies worldwide, particularly in high-fertility regions. Moreover, GBD uses live births as the denominator for HDP incidence. In regions with high fertility rates (e.g., Sub-Saharan Africa), the 25–29 age group contributes disproportionately to live births, which may amplify incidence rates.
Based on the current epidemic trajectory, this study predicted the global burden from 2022 to 2046. However, the influence of potential changes in national policies over the coming decades could not be predicted. For example, the birth-friendly or birth-limiting policies may directly alter the gravida and para of different age groups, further affecting the risks of MHD. Moreover, unpredictable environmental factors, such as climate change, were not hereby taken into account. This could affect the prevalence of MHD through the fluctuation of temperature and humidity, as humidity and temperature were found to be related with the incidence of preeclampsia [25]. Additionally, industrial development could lead to the exposure to toxicants and metal(loids), which were proved to be associated with the hypertensive disorders of pregnancy [26]. Consequently, the inability to predict future trends in MHD based on the aforementioned factors was a limitation of the present study, warranting additional evidence to facilitate more convincing predictions.
Furthermore, this study has the following limitations. Despite the global standardized processing of GBD data, variations in the integrity and consistency of basic data sources could underestimate the true disease burden and affect analyses of health inequalities. In addition, in terms of study methodology, while a variety of analytical methods were utilized to analyze epidemiological changes in MHD, each may be subjected to inherent limitations that could affect the results. For example, in attribution analysis, limited data on risk factors for MHD were collected in GBD studies, hindering the assessment of MHD risks. Concurrently, this study only used BAPC model for prediction analysis, and a variety of prediction models could be used in the future and combined with machine learning methods to ensure the robustness of the results. Moreover, this prediction model did not incorporate the Socio-demographic Index (SDI) as a covariate or stratify predictions according to SDI levels. Such a limitation could affect the generalizability of the findings across populations with varying socioeconomic contexts. Future studies should consider integrating SDI or other socioeconomic indicators to refine predictive models and better capture the influence of socioeconomic factors on disease burden.
This study performed a comprehensive analysis of the global burden of MHD and observed inequalities in both the regional and national levels. The investigation also revealed a correlation between MHD and SDI. The overall tendency of the disease burden was decreasing in most regions, indicating the efficiency of prenatal examinations, clinical interventions, and health educations. Further investigations should be carried out to enable more convincing predictions for the future epidemiological dynamics and to assist the establishment of public health strategies for MHD prevention.
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Acknowledgements are extended to all individuals having contributed to this article.
This research was supported by the National Natural Science Foundation of China, Youth Science Foundation Project (82201863).
All data in this study were collected from GBD database, requiring no additional ethical approval.
All authors approved the publication of this article.
The authors declare no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Zhao, J., Gong, R., Sui, X. et al. Global, regional, and national burden, trends, and inequality analysis of maternal hypertensive disorders (MHD) from 1990 to 2021, and predictions to 2046. BMC Pregnancy Childbirth 25, 680 (2025). https://doi.org/10.1186/s12884-025-07777-9