Health Research Policy and Systems volume 23, Article number: 76 (2025) Cite this article
Existing research indicates that both subject trust and procedural justice exert an influence on government staff’s level of identification with health impact assessment (HIA) policies, revealing notable differences in attitudes, comprehension levels and preferences for implementing HIA policies among staff from different sectors. There is an urgent requirement to develop an integrated research model that systematically investigates the extent of HIA policy identification and its underlying drivers, commencing with the perspectives of staff from health and nonhealth sectors alike.
A questionnaire survey using a multistage stratified random sampling method was conducted among health sector staff (n = 247) and nonhealth sector staff (n = 408) in Zhejiang province in China. Univariate analysis was used to describe differences in HIA policy identification between the two groups. A multigroup analysis within a structural equation model tested the similarities and differences of influencing factors on HIA policy identification in different sectors.
Health sector staff (4.26 ± 0.59) demonstrated a significantly higher level of policy cognition regarding HIA than nonhealth sector staff (3.96 ± 0.63). Conversely, nonhealth sector staff (3.72 ± 0.73) exhibited significantly higher levels of policy evaluation than health sector staff (3.47 ± 0.88). Subject trust positively influenced the three dimensions of HIA policy identification for both groups. However, procedural justice only positively influenced the policy sentiment and evaluation of health sector staff, with no significant impact on nonhealth sector staff. Additionally, other factors, such as position, education, work experience and familiarity with HIA, impacted HIA policy identification across sectors.
This study confirms that subject trust can enhance policy identification and cooperative behaviour. On the basis of this, the health sector should strive to understand the policy objectives of other sectors to seize opportunities for action, thereby enabling nonhealth sectors to participate in the actions of the health sector.
Health impact assessment (HIA) serves as an effective governance tool to promote health in all policies (HiAP) by assessing the potential health impacts of policies, programs or projects on populations. It generates recommendations for decision-makers and stakeholders to maximize positive health outcomes [1, 2]. The core of health impact assessment (HIA) is to identify and analyse the effects of social determinants of health (SDH) on health and propose interventions that promote health equity [3]. SDH encompasses socioeconomic factors influencing health status, including housing, income, education, employment, transportation, healthcare and social relationships. Despite their profound impact on health, these factors are often overlooked [4]. Addressing SDH typically requires collaboration across multiple sectors, as they extend beyond the control of any single field. For example, UNESCO has emphasized the interdependence of education and health policies and has urged governments to develop policies that support both [5, 6]. HIA underscores the importance of considering the effects of SDH in policymaking to achieve equitable and sustainable health [7, 8].
HIA has gained significant attention and support from global leaders in many countries and has been widely applied in policymaking and project evaluations across various fields, including housing policy, transportation planning and education reform [6, 9, 10]. In Hangzhou, the capital of Zhejiang Province, the so-called health in all policies concept has been incorporated into local planning guidelines. The city has established a collaborative framework for comprehensive health development, enabling multisectoral coordination and integration. Health recommendations have been extensively adopted in urban spatial planning and public policymaking, such as road classification and the optimization of green space layouts, to enhance residents’ health environments [11]. Moreover, Hangzhou has developed a public policy health impact assessment tool to integrate health considerations into urban design and planning [12]. Scholars have conducted extensive research on related concepts [13,14,15], theoretical frameworks, implementation status, challenges [16,17,18], practical applications and methodologies [19, 20]. These studies emphasize the significance of HIA in achieving health governance and offer guidance for departmental HIA implementation. However, both practice and research indicate that successful HIA implementation hinges on intersectoral collaboration between health and nonhealth sectors [21]. The complexity of health determinants and the diverse domains involved in HIA necessitate collaborative efforts across multiple sectors [22]. Several countries, such as Finland [23] and Thailand [24], have established intersectoral health committees responsible for coordinating national HIA endeavours.
Intersectoral collaboration hinges on sectors reaching a consensus on the same policy and establishing a strong policy identity. Eugene Bardach [25] advocates that cross-sector collaboration occurs when different sectors with shared interests collaborate to form a cooperative intention and enhance public value through their complementary advantages. Further research suggests that robust policy identification can strengthen trust between sectors [26], facilitating the resolution of policy issues and advancing mutual interests, thereby effectively driving policy implementation. The original conceptual framework for HIA developed by Harris-Roxas highlights that departments (or organizations) can collaborate most effectively when common values and objectives are identified [27, 28]. Health and nonhealth sector staff, as the crucial actors responsible for enacting HIA policies, have a direct impact on the effectiveness of implementation through their level of understanding and alignment with these policies. Therefore, enhancing the level of alignment among health and nonhealth sector staff in executing HIA policies is crucial for fostering interdepartmental cooperation in HIA policy implementation.
Policy identification, a psychological concept, generally refers to the target group’s tendency to exhibit affirmation, approval and support towards a policy, ultimately manifested through their behaviour. Talcott Parsons’s social system theory [29] suggests that every specific action encompasses cognitive, emotional and evaluative elements. Cognitive elements refer to knowledge, emotional elements are associated with emotions and evaluative elements relate to judgment and ranking of the object. Zhang and Tang [30] proposed a general formula for public policy identification: Policy identification equals trust in political authority multiplied by procedural justice multiplied by subjective evaluation of distributive justice. This indicates that the acceptability of public policy is the subjective evaluation of the expected outcomes of policy implementation by the policy target and the public’s level of identification. In the health domain, scholars such as Toumpakari et al. [31] highlight that policy effectiveness, justice and clear communication of policies are crucial factors influencing acceptability among the public and policymakers.
Existing research indicates differences in attitudes, comprehension levels and preferences for implementing health impact assessment policies among staff from different sectors [32]. These disparities lead to limited recognition and importance within sectors, subsequently affecting the smooth implementation of HIA [33].
Harris-Roxas et al. [34] assert that the primary threat to HIA originates within the health sector. They highlight the concerning issue of medicalization, where medical interventions are favoured even for nonmedical concerns, potentially leading to the neglect of broader considerations. This phenomenon neglects external factors contributing to adverse health outcomes and overlooks the roles other sectors play in health promotion and disease prevention [35]. From the perspective of nonhealth sectors, enhancing health awareness and proactiveness is necessary. However, influenced by self-interest, nonhealth sectors tend to focus solely on their departmental work, failing to consider health impacts beyond their immediate interests [36, 37]. Additionally, the inherent functional separation between departments, coupled with limited interdepartmental interaction, hampers their capacity for comprehensive health consideration. Furthermore, differing organizational cultures and limited understanding of each other’s specialized terminologies may lead to discourse discrepancies and conflicts between health and other policy objectives, hindering the formation of strong interdepartmental work relationships [38]. On the basis of social system theory and the general formula proposed by Zhang and Tang [30] for public policy identification, Liu et al. [39] explored the levels of policy identification among staff involved in HIA in Zhejiang Province. Their study found significant differences between health and nonhealth sector staff in terms of policy cognition and sentiment. Additionally, subject trust influenced policy cognition, sentiment and evaluation among HIA staff, while procedural justice had a positive impact on their policy sentiment and evaluation.
However, existing research often encompasses all HIA staff without differentiating the factors influencing policy identification between the health and nonhealth sectors. Therefore, we propose dividing HIA staff into these two categories for a comprehensive examination of the differences in their policy identification and the factors influencing them. This approach aims to identify and address the barriers to intersectoral collaboration in HIA, offering valuable insights and enhancement strategies for fostering collaboration. Ultimately, this work contributes to more coordinated health governance and stronger consensus across diverse sectors.
Zhejiang Province is the only region in China designated as a pilot for establishing a HIA system. Since 2016, it has been working toward developing a comprehensive HIA framework, with the goal of achieving full implementation at the provincial, municipal and county levels by 2025 [40]. This initiative aligns with the Healthy China 2030 Planning Outline and aims to integrate health considerations into all policies through HIA, ultimately improving the overall health of residents across the province.
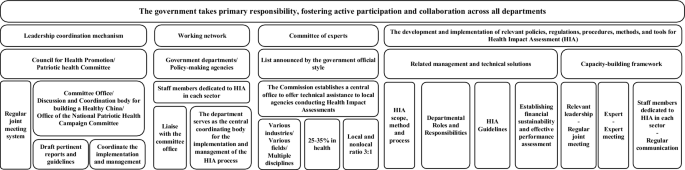
The HIA system demands stronger intersectoral collaboration to build a functional network. The establishment of the HIA system in Zhejiang Province (Fig. 1) requires the creation of organizational management and coordination mechanisms alongside the development of a functional network. Existing health-related coordination mechanisms at all levels of government should be combined to oversee the progression and execution of significant public policy health impact assessments within their respective administrative regions. Additionally, each department involved in HIA work must integrate it into their routine responsibilities, appointing accountable leadership and assigning dedicated personnel to coordinate, implement and manage health impact assessments for crucial public policies within their department.
Furthermore, the HIA system calls for pooling resources from various sectors to establish an expert committee. This committee should comprise members from diverse fields and disciplines across various sectors, including experts and professionals with distinguished academic achievements from both health and nonhealth sectors. The objective of constructing the HIA system is to foster voluntary collaboration among personnel from different sectors through the sharing of information, resources, risk assessments and decision-making. This collaborative effort seeks to achieve departmental synergy, mutual cooperation and collective planning, with the ultimate goal of protecting population health and promoting health equity. It enables the accomplishment of health-related tasks that may be challenging or impossible for the health sectors alone, thereby realizing coordinated health governance. This collaborative model establishes the groundwork for the successful implementation of HIA and provides valuable lessons and models for HIA initiatives in other regions and domains. The continual enhancement of HIA mechanisms through intersectoral collaboration has positively contributed to the health and well-being of the populace.
Nevertheless, Zhejiang Province faces common challenges in cross-departmental collaboration during implementation, including poor communication between departments and inconsistent policy interpretation. Selecting Zhejiang as the research area not only reflects broader trends in HIA implementation in China but also provides region-specific insights with practical guidance. Examining Zhejiang’s HIA practices can serve as a valuable reference for other regions, facilitating the broader adoption of health policies.
Policy identification, essentially a psychological phenomenon, reflects how individuals acknowledge and support public policies [41]. Parsons’s social system theory [29] provides a theoretical framework and guidance for understanding the formation and impact of policy identification, explaining the relationship between an individual’s level of identification with a policy and other elements within the social system. On the basis of this theory, we distinguish three dimensions of policy identification – policy cognition, sentiment and evaluation – as measured in Xi Junyuan’s [42] research. Policy cognition refers to the depth of understanding that different departmental personnel possess regarding the value and execution details of HIA policies. This acts as the prerequisite and foundation for policy identification. Policy sentiment represents the emotional response of different sectoral staff towards HIA policies, manifesting as psychological approval, satisfaction or other forms. It forms the core and essence of policy identification. Policy evaluation pertains to the assessment of the outcomes of HIA policy implementation, reflecting the attitudes of different departmental personnel towards the policies. This serves as a tangible manifestation of the ultimate significance and value of policy identification. Strong policy identification signifies alignment between policy values and the needs of target groups within the HIA policy process, thereby enhancing support and cooperation for policy implementation.
Liu et al.’s [39] research highlights the differences in levels of policy identification among HIA staff across different sectors. Their study also indicates that both subject trust and procedural justice impact HIA staff’s policy sentiment and evaluation, while only subject trust was significantly associated with policy cognition. However, the research did not specifically differentiate the factors influencing policy identification between the health and nonhealth sectors. Building upon this, we categorize HIA staff into health and nonhealth sectors and examine in more detail the distinct influencing factors of policy identification within each group. Subject trust refers to the extent of approval and trust that individuals within various sectors hold toward the government health department responsible for formulating and executing HIA policy, as well as toward evaluation agencies, experts and assessment outcomes. This measurement approach builds upon Liu Bing’s [43] method for measuring government trust dimensions. Procedural justice pertains to whether individuals perceive the methods and processes leading to decision outcomes as fair. It involves perceptions among sectoral staff regarding the fairness and consistency of the HIA implementation process, the comprehensiveness of experts involved in HIA, the diversity of policy evaluation methods and the transparency of information related to HIA implementation. This measurement is based on Harold et al.’s [44] Procedural Justice Perceptions Scale.
Therefore, this article proposes the following hypotheses:
H1: Subject trust positively influences policy identification (policy cognition, policy sentiment and policy evaluation) among health sector staff.
H2: Subject trust positively influences policy identification (policy cognition, policy sentiment and policy evaluation) among nonhealth sector staff.
H3: Procedural justice positively influences policy identification (policy sentiment and policy evaluation) among health sector staff.
H4: Procedural justice positively influences policy identification (policy sentiment and policy evaluation) among nonhealth sector staff.
This study employed a multistage stratified random sampling method to conduct a questionnaire survey among health and nonhealth sector staff in Zhejiang Province, China’s public policy HIA pilot areas (hereafter referred to as pilot areas). Health sectors included provincial health departments, city health bureaus, health inspection institutes, centres for disease control and prevention and medical insurance bureaus, while nonhealth sectors comprised transportation bureaus, agricultural and rural bureaus, education bureaus, ecological environment bureaus and water resources bureaus. The pilot areas were stratified and sampled on the basis of Zhejiang Province’s geographic distribution, with representatives selected from Hangzhou, Taizhou, Quzhou and Jiaxing. Subsequently, one to three counties/districts were randomly selected from each city. Finally, 20–30 HIA policy implementation staff from the health sector and 30–40 from the nonhealth sector were surveyed in each city and county/district. Between June 2021 and December 2022, a total of 690 staff members were surveyed using a one-on-one approach, yielding 655 valid questionnaires (247 from health sector staff and 408 from nonhealth sector staff). The scientific research ethics committee of Hangzhou Normal University granted ethical approval for this study (approval number: 2021–1040).
The questionnaire consisted of four sections: sociodemographic information questions, subject trust questions, procedural justice questions, and questions measuring policy identification. Participants were asked to rate the items on a 5-point Likert scale, ranging from 1 (strongly disagree) to 5 (strongly agree), respectively. The questionnaire’s reliability and validity have been established in Liu et al.’s studies. The internal consistency of the measurement was assessed using Cronbach’s alpha, which ranged from 0.731 to 0.912, indicating good reliability. Validity was evaluated using standardized factor loadings and average variance extracted (AVE). All standardized factor loadings were statistically significant (p < 0.001), and all AVE values exceeded 0.5, demonstrating satisfactory validity.
Questionnaire data were entered into the Epidata software (version 3.1) and then transferred to the SPSS software (version 23.0) for cleaning, merging and analysis. Descriptive statistics, including frequencies and proportions, were used to describe the demographic characteristics of survey participants. Independent sample t-tests were conducted to investigate potential differences in policy identification between staff in health and nonhealth sectors. t-tests and one-way analysis of variance (ANOVA) were employed to assess the influence of demographic characteristics on policy identification among staff in both sectors. Measurement invariance was tested using Amos (version 24.0). Subsequently, the differences in the effects of policy cognition, policy sentiment and policy evaluation, which are important dimensions of HIA policy identification, were investigated on subject trust and procedural justice between health sector and nonhealth sector staff using multigroup structural equation modelling.
Herein, we conducted in-depth interviews with 30 experts, each with over 3 years of professional experience in HIA, healthy city development and health promotion at the county (district) level. Among them, 15 were members of the HIA system leadership group from pilot cities and counties. The interview questions were developed on the basis of a comprehensive literature review and focused on the following topics: (1) awareness of HIA policies, (2) understanding of cross-departmental collaboration in HIA policies, (3) perspectives on current barriers to implementing cross-departmental collaboration in HIA policies and (4) suggestions for improving interdepartmental cooperation.
Table 1 provides an overview of the basic demographic characteristics of the study sample. The ratio of male-to-female participants was relatively even in both health and nonhealth sectors. The age distribution of the participants was well-distributed, with most ranging between 31 and 50 years. The educational level of the participants was mostly bachelor’s degree or higher, indicating a high level of education within the sample. Both health and nonhealth sector participants had been in their current positions for less than 5 years. Regarding prior knowledge of HIA policies, over half of the health sector staff had prior knowledge, while only 38.2% of nonhealth sector staff had heard of it.
Table 2 highlights the key differences in the levels of policy cognition, sentiment and evaluation of HIA between health and nonhealth staff. Specifically, health staff had significantly higher levels of policy cognition (4.26 ± 0.59) compared with nonhealth staff (3.96 ± 0.63). In contrast, nonhealth staff (3.72 ± 0.73) exhibited significantly higher levels of policy evaluation than the health sector staff (3.47 ± 0.88). However, both groups demonstrated similar levels of policy sentiment, with health staff scoring slightly higher; however, the difference was not statistically significant.
Table 3 summarizes the findings of a univariate analysis examining the influence of demographic characteristics on HIA policy identification among health and nonhealth sector staff. For health sector staff, holding deputy officer or higher positions and having postgraduate education or higher were associated with significantly higher levels of policy cognition compared with clerks, officers and those with lower education levels. Additionally, prior HIA knowledge was linked to higher mean scores in both policy cognition and sentiment. Notably, individuals between 21 and 30 years old displayed the highest mean scores in policy evaluation. Among nonhealth sector staff, positions at deputy officer level or above were associated with significantly higher policy cognition compared with clerks and officers. Prior HIA knowledge was also linked to significantly higher mean scores in all three dimensions of policy identification. Overall, the findings suggest that, within the health sector, higher levels of education, management positions and prior HIA knowledge are associated with stronger policy identification. For nonhealth sector staff, only management positions and prior HIA knowledge showed a significant positive association with policy identification.
To assess the comparability of measurements across sectors, we followed the established procedure for testing measurement invariance [45]. We examined five models: one with no constraints (M1), one with equal factor loadings (M2), one with equal structural coefficients (M3), one with equal structural covariances (M4) and one with equal residual variances (M5). As indicated in the Table 4, the nonsignificant differences between M2 and M1 (p = 0.646), M3 and M2 (p = 0.225), M4 and M3 (p = 0.562) and M5 and M4 (p = 0.432) support the conclusion that the HIA policy identification and its influencing factors model are measurement-invariant across sectors in terms of factor loadings, factor variance–covariance, structural coefficients and residuals.
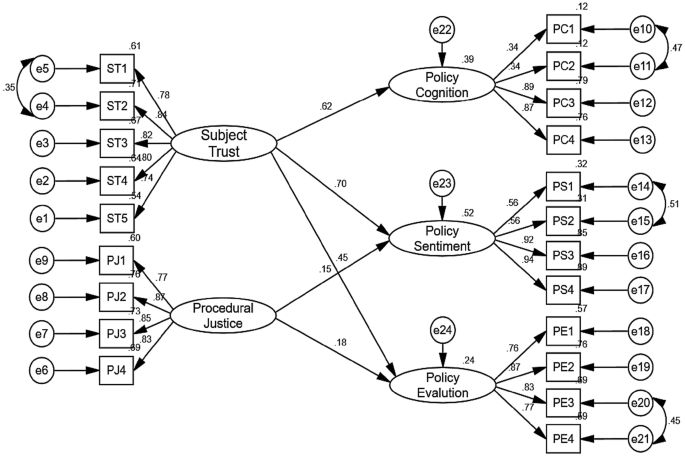
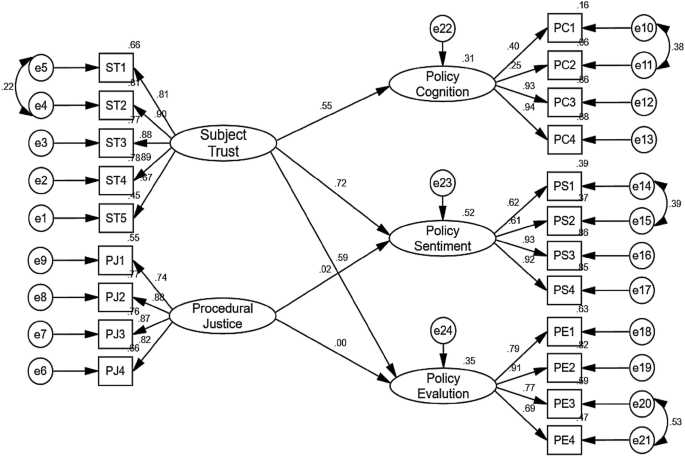
Building upon the measurement invariance analysis, Figs. 2 and 3 present the structural equation model results for HIA policy identification and its influencing factors among health sector staff (n = 247) and nonhealth sector staff (n = 408), respectively. As presented in Table 5, the impact of subject trust on all three components of policy cognition was statistically significant across both groups. This suggests that employees with a higher level of trust in the HIA executing department, regardless of sector, exhibit higher levels of understanding and knowledge about HIA policy. However, the impact of procedural justice on policy sentiment and policy evaluation differs between sectors. In the health sector data, we observed a positive and statistically significant relationship between fairer and more transparent HIA execution processes and both higher positive feelings towards the policy and more positive evaluations of its outcomes. Conversely, for nonhealth sector staff, procedural justice did not have a statistically significant impact on either policy sentiment or evaluation.
Herein, we investigated the level of understanding and support for HIA policies among health and nonhealth sector staff involved in HIA implementation, exploring the factors that influence their level of engagement with the policy.
A significant disparity exists in how health and nonhealth sector staff understand and support HIA policies. Health sector staff often exhibit a higher level of awareness and understanding, while nonhealth staff may be more actively involved in implementation.
As key contributors to health improvement, health sector employees typically have professional expertise in medicine and public health. Their work is directly related to public health, disease prevention and medical services [46]. Consequently, they tend to have a strong interest in and a high level of awareness of the core concepts, theoretical foundations and practical applications of HIA policies. In addition, the health sector frequently organizes training and educational programs to help staff update their knowledge and deepen their understanding of HIA policies. This may account for the higher level of awareness of HIA policies among health sector employees.
In contrast, employees from nonhealth sectors typically have diverse academic backgrounds, including economics, sociology, law and management. This interdisciplinary knowledge structure allows them to examine HIA policies from multiple perspectives, adopting a more macro-level view that considers the economic, social and environmental impacts of policies [47]. Their practical experience in policy analysis and evaluation further enables them to identify key policy elements and assess implementation outcomes more effectively. The distinct roles played by the two sectors in HIA policy implementation also shape their approaches to policy evaluation. In the implementation of HIA policies, the health sector is responsible not only for coordinating the participation of various departments but also for ensuring that these departments actively utilize HIA tools, placing considerable pressure on them. Under such circumstances, coordination difficulties and challenges in cross-departmental collaboration may contribute to lower policy evaluation levels within the health sector. In contrast, employees from nonhealth sectors are directly involved in executing HIA policies, prioritizing health considerations in developing policies, projects and plans. While pursuing their original policy objectives, they place greater emphasis on population health. One nonhealth sector employee explained: “Our department is primarily responsible for urban planning and construction. Previously, we focused more on the economic benefits and technical feasibility of projects. However, after implementing the health impact assessment, we began to place more emphasis on public health issues during policy formulation. For instance, when planning a new residential area, we use HIA to predict and analyse the potential impacts on the health of nearby residents, such as environmental pollution, traffic conditions and noise levels. This enables us to take appropriate measures during the planning stage to mitigate or eliminate these adverse effects, ensuring both the sustainability of the project and the health of the public”.
This demonstrates that nonhealth sector employees may have a higher evaluation of HIA policies owing to their recognition of the impact of their own work. Such patterns are also evident in various fields, including healthcare [48] and agricultural projects [49]. The roles and contributions of the two sectors in HIA policies have different focuses, offering diversified perspectives and approaches that collectively advance the improvement and implementation of HIA policies. The results are summarized in Table 6.
Demographic characteristics
Our findings suggest that several factors significantly influence staff acceptance of HIA policies, regardless of their sector. Staff in higher positions displayed greater understanding and support for the policies, as previously noted by Zhu and Liu [50]. This may be due to the so-called top-down communication model in most organizations, where senior management receives and disseminates policies, leading to increased awareness among those in higher positions.
Staff with prior HIA training displayed significantly higher levels of policy understanding and support compared with those with no prior exposure to HIA concepts. This finding underlines Silveira et al.’s assertion that raising awareness of HIA’s importance among both health and nonhealth professionals is crucial. To this end, health sectors should actively invest in training programs for policy implementers, specifically focusing on HIA principles and best practices [51]. Such initiatives would not only enhance policy comprehension but also improve overall effectiveness in implementing HIA initiatives. Furthermore, our data suggests that health staff with higher educational attainment demonstrate a stronger grasp of HIA policies. This could be explained by their systematic education in health promotion and related fields, which fosters a greater receptiveness to policies aimed at public health advancements. However, it is important to acknowledge that other factors, such as individual interest or specific work experience, might also play a role in shaping HIA acceptance and understanding.
Subject trust
Higher trust in the HIA system, whether in the professionals, process or implementing organization, positively influences all three dimensions of HIA policy cognition for both health and nonhealth staff, as shown by Lan Gao [52] and Lingyi Zhou [53]. For health professionals, this trust deepens their understanding of HIA and other policy domains, fostering strong intersectoral relationships. This understanding often stems from improved access to information and more open communication channels [21]. For nonhealth staff, trusting the HIA system fosters collaboration because it creates a willingness to work together. This leads to better information sharing, resource integration and coordinated actions when implementing HIA [21]. Importantly, high trust across sectors motivates staff to actively develop the public health skills needed for HIA implementation. They become more critical in applying various evidence and data types, analysing how policy decisions impact health across different domains. This deeper understanding leads to greater acceptance of policy goals and principles within each sector, reducing disputes and promoting long-term policy stability [54].
Procedural justice
Procedural justice only positively influences the policy sentiment and evaluation of health sector staff (p < 0.05) for HIA policies, not those of nonhealth sector staff. Two explanations might account for this difference. First, health sector staff may actively participate in formulating HIA policies or leading their implementation. This involvement allows them to voice their opinions and judge the fairness of decision-making, potentially influencing their policy acceptance. In contrast, nonhealth staff might primarily perform tasks such as project evaluations, limiting their understanding of the overall fairness of the process.
Second, the impact of procedural justice might not be as constant as expected. Research suggests an interaction with subject trust: when individuals trust policy implementers, they might demand less procedural justice [55, 56]. In real-world situations, interactions between HIA staff and both health and nonhealth personnel might build trust before they receive procedural information about HIA policies [57]. This high level of trust might weaken the effect of procedural justice.
International studies consistently identify insufficient collaboration between different sectors as a major barrier to effective policy implementation [58]. In Denmark, for example, implementing health impact assessments faces challenges owing to the lack of universal tools and a culture of cross-sectoral cooperation [18]. To address this issue, fostering collaboration between departments can help staff consider the broader health implications of their work. Public health professionals, in particular, should actively build relationships and engage with sectors such as housing, education and transportation, which significantly impact social determinants of health and equity [16, 59,60,61]. As a tool specifically designed to facilitate cooperation between different sectors, HIA offers the flexibility to adapt to evolving needs.
However, in China, a significant disparity exists in the level of participation between health and nonhealth sectors in HIA research and implementation. This is despite the recognition that policies outside the health sector, such as economic development and planning, have profound impacts on health and equity. Therefore, strengthening coordination mechanisms between health and nonhealth sectors is crucial. Supporting cross-sectoral collaboration and multilevel governance can create synergies that improve health outcomes, ultimately enhancing policy understanding in both health and nonhealth sectors. In HIA practice, establishing trust-based multisectoral collaboration mechanisms is key to achieving this goal. Government-level initiatives promoting cross-sectoral cooperation and building trust among stakeholders through effective communication and clear roles are crucial for institutionalizing HIA [62]. Trust acts as a foundation for collaboration, facilitating information exchange and encouraging positive behaviours. Within the HIA work process, trust relationships are essential for constructing collaborative governance models. Fostering a positive working environment and cooperative atmosphere that promotes mutual trust among government staff across sectors enhances their identification with the organization and policies. For the health sector, procedural justice not only increases trust in the HIA system but also motivates healthcare professionals to actively engage in implementation. Establishing and maintaining open channels for meaningful public participation, actively seeking feedback and encouraging transparency enhances information sharing and overall effectiveness.
To foster successful HIA implementation in nonhealth sectors, we must clearly communicate the policy’s impact and benefits. Differentiated training programs should be designed by developing targeted HIA courses that address the specific needs of nonhealth sectors, incorporating practical case studies to illustrate the potential impacts of HIA. Highlighting how the policy affects not only the organization but also the wider community can encourage stronger buy-in and identification from nonhealth staff. Providing necessary support and resources is essential to empower nonhealth staff to understand and apply HIA policies effectively [63]. Furthermore, policy transparency should be enhanced by openly sharing the policy-making process and evaluation standards, promoting greater recognition of procedural fairness and improving policy acceptance among nonhealth sectors. By integrating the expertise and experiences of diverse stakeholders, cross-sectoral collaboration can lead to more comprehensive policy decisions with broader support.
This study utilized multigroup analysis to assess the invariance of the HIA policy identification model across health and nonhealth sectors. The results confirmed the positive influence of subject trust on policy identification in both groups. However, a limitation of this study is that we examined the main effects of trust and procedural justice without investigating their potential interactions. Future research should further explore their effects and interactions by integrating both quantitative and qualitative methods, thereby providing a more comprehensive understanding of the factors influencing policy identification across different sectors.
The key to implementing HIA is cross-sector collaboration between health and nonhealth sectors. This study, from the perspective of policy acceptance, categorizes HIA practitioners into health sector and nonhealth sector staff and examines the differences in their acceptance of HIA policies and the influencing factors. The findings reveal distinct characteristics between the two groups regarding policy awareness, sentiment and evaluation. These differences highlight the varying priorities of each sector in policy acceptance and implementation, providing a foundation for developing more targeted strategies for cross-sector collaboration.
The health sector should strengthen training and support for nonhealth sectors to improve their understanding of HIA policies. At the same time, the nonhealth sector should engage more actively in the policy-making and implementation processes, incorporating the concepts and methods of health in all policies into their routine work, such as developing policies, projects and plans. Building trust and enhancing communication efficiency between sectors is crucial for advancing cross-sector collaboration in HIA. Open communication, joint working groups and information sharing can all help foster trust and mutual understanding.
The hypothesis regarding the influence of procedural fairness was not fully supported, indicating that future research could further explore the interaction between trust and procedural fairness. Additionally, it could investigate how specific management measures might enhance the effectiveness of cross-sector collaboration.
No datasets were generated or analysed during the current study.
We thank all the study participants for giving their time to complete the questionnaire. We are also grateful to the Home for Researchers editorial team (www.home-forresearchers.com) for language editing service.
No external funding was received for this study.
The scientific research ethics committee of Hangzhou Normal University granted ethical approval for this study (approval number: 2021–1040). Before distributing the questionnaires, oral informed consent was obtained from all participants.
Informed consent has been obtained from all participants in the study.
The authors declare no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Xu, Y., Song, L., Liu, X. et al. Exploring factors influencing health impact assessment policy identification in China: a comparative study of health and nonhealth sectors. Health Res Policy Sys 23, 76 (2025). https://doi.org/10.1186/s12961-025-01312-0