AIDS Research and Therapy volume 22, Article number: 40 (2025) Cite this article
HIV/AIDS remains a public health threat globally. The disclosure rates of positive HIV status by young people living with HIV (YPLHIV) to their sexual partners vary and have been reported as low as 31%, despite the consequences of non-disclosure. Little is known about disclosure to sexual partners among YPLHIV in most of Sub-Saharan Africa, including Uganda. We assessed the prevalence, determinants, barriers and facilitators of HIV status disclosure to sexual partners among YPLHIV in care at an urban HIV clinic in Uganda.
The study utilized a cross sectional design using a parallel-convergent mixed method approach. We conducted 281 structured interviews through random sampling and 16 purposively sampled in-depth interviews (IDIs) among YPLHIV (18 to 24 years). Descriptive analysis was done to obtain the frequency and percentage of HIV status disclosure to sexual partners of YPLHIV. Modified Poisson regression was used to determine associated factors at multivariate analysis and adjusted prevalence ratios, 95% CI and p values were obtained using STATA version 14. Verbatim transcription and thematic analysis using NVIVO version 12 was used to explore the barriers and facilitators of HIV status disclosure to sexual partners using the health belief model.
The prevalence of HIV status disclosure to sexual partners was 45.2%. Having a known HIV free partner (aPR = 0.6, P < 0.001), being a partial or complete orphan (aPR = 1.4, P = 0.022), knowing one’s HIV status for > 1 year (aPR = 0.7, P < 0.001), and having 2 rather than 3 sexual partners (aPR = 1.7, P = 0.013) were among the determinants of HIV status disclosure. Facilitators of disclosure included; health worker/peer support, nature of relationship, protecting partners against HIV, need for social/financial support. Barriers to disclosure included; lack of confidence to disclose, fear of sexual partners’ reaction, awareness of undetectable HIV viral load equated to none HIV transmission, influence by parents among others.
This study revealed a low HIV status disclosure prevalence to sexual partners among YPLHIV. Addressing potential barriers through comprehensive health education including the role of viral load in HIV transmission, and creating supportive environments to enhance their confidence, will improve disclosure rates among YPLHIV to their sexual partners.
Despite several interventions, the Human Immunodeficiency Virus (HIV) incidence remains high globally with over 1.3 million newly acquired HIV infections, 92.3% of which among people aged 15 + years by 2022 [1]. Likely, the majority of these new HIV infections among the young people in their early reproductive age resulted from sexual transmission [2]. Approximately 4000 females aged 15 to 24 years were newly diagnosed with HIV per week globally, 77.5% occurring in Sub-Saharan Africa [1]. There have been several interventions targeting HIV prevention. Moreover, as part of positive health, dignity, and prevention, it is important for PLHIV to protect their sexual partners by adhering to their anti-retroviral therapy (ART) and maintaining a suppressed viral load (VL). Disclosing to sexual partners about one’s HIV status and consistent condom use is reduces HIV sexual transmission [3]. Disclosure to a sexual partner may bring about improved social and treatment support [4], better adherence on ART, viral load suppression and reduced risk of HIV transmission. In SSA, prevalence of HIV status disclosure to sexual partners greatly varies among different populations, ranging between 32% and 86.5% [5,6,7]. In Uganda, it has been reported between 57% and 83.7% among adults [8, 9] and 31% among YPLHIV [10]. The decision to disclose positive HIV status to a partner is influenced by various factors which may include, discussion with partner about HIV testing, socio economic dependency [11], partner’s status, advanced HIV disease, education level, nature of relationship [9, 12], time spent in HIV care and on ART [13], consistent condom use and use of leisure substances including alcohol [14, 15].
Consequences of non-disclosure to sexual partners may include as taking ART in hiding, poor coping skills and psychological stress [5, 16], and thus poor health outcomes. Moreover, non-disclosure affects adherence to ART and also leads to interruption of care [17], resulting in unsuppressed VL, ill health and transmission of HIV to sexual partners [18,19,20,21]. Improving disclosure rates of HIV status by YPLHIV to sexual partners may improve adherence on ART, viral load suppression and ultimately a reduction HIV transmission [19] in this sub-population.
In this study, we set out to determine the prevalence, associated factors, barriers and facilitators for HIV status disclosure to sexual partners among YPLHIV and make recommendations for improvement based on the observed dynamics.
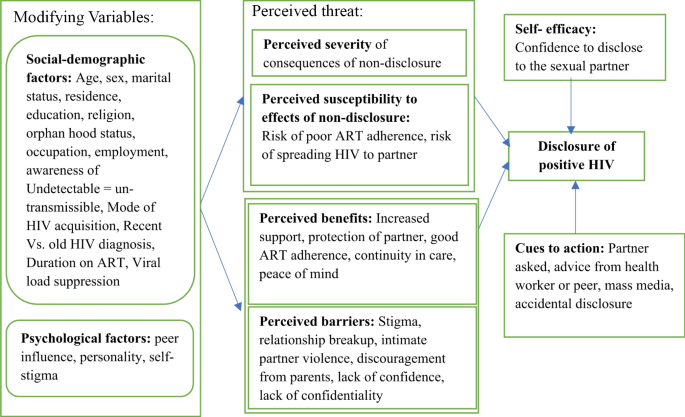
We adopted the health belief model [22], which is widely used in health behaviour, to understand the different barriers and facilitators of HIV status disclosure among YPLHIV to their sexual partners (See Fig. 1).
Illustration of the health belief model [23], adopted from the Handbook for Designing and Conducting Clinical and Translational Research, 2023
[22] In this model, performing a health behaviour is as a result of balance between the perceived threat of a health condition and benefits and barriers to the behaviour. The perceived threat and benefits should outweigh the perceived barriers if positive action is to be done about a behaviour [22]. It also requires that one must be confident enough to act. It is suggestive that performing a desired health behaviour, in this respect disclosure of positive HIV status to a sexual partner, is as a result of individual’s characteristics and assessment of different aspects including; perceived threat of nondisclosure, perceived benefits and, perceived barriers of disclosure, self-efficacy and cues to action [22, 24].
This was a mixed methods parallel convergent study in which both quantitative and qualitative data were collected concurrently and analysed concurrently, and later on interpreted together. To determine the prevalence and factors associated with disclosure of HIV status to sexual partners of YPLHIV, a cross-sectional study was conducted. An exploratory design was used to determine the barriers and facilitators of disclosure of HIV status to the sexual partner(s). This gave us some explanation for the observed prevalence of HIV status disclosure.
The study was conducted at the Baylor Foundation Uganda, HIV clinic, a provider of family centred HIV care with a population of over 8,500 PLHIV of which 35% were YPLHIV aged 15 to 24 years at the time of the study. The clinic is located at Mulago National Referral Hospital within the capital city of Uganda, Kampala and offers a variety of services on an outpatient basis including HIV care and treatment, clinical research and education. The proportion of sexually active young people at the clinic was unknown. It was however observed during clinic visits, that non-disclosure to sexual partners was among the common reasons for non-adherence to ART, hence the observed detectable viral loads and missed appointments among the YPHLIV at the clinic.
Determining the prevalence and factors associated with disclosure of HIV status to sexual partners by YPLHIV;
The study population was YPLHIV aged 18 to 24 years, attending the HIV clinic. We included those who reported to have been in a relationship(s) involving sexual intercourse, then or within 12 months prior to the study and consented to participate in the study. Presence of mental impairment after chart review would lead to exclusion from the study as it would potentially affect the ability to offer informed consent for participation. However, none of our potential participants had mental impairment at the time of the study.
For the quantitative study, we used the Leslie Kish formula [25], to estimate a sample size of 281 participants to determine the prevalence and factors associated with HIV status disclosure to sexual partners. Daily, we used the clinic’s booking electronic medical record system to identify potential participants who were then approached and screened for eligibility. After ascertaining sexual activity, a sampling frame was made and potential participants were assigned unique identifiers. Participants were then selected by simple random sampling from this frame using Microsoft Excel generated random numbers until the desired sample size was reached.
We collected data between February and April of 2023 at the Baylor Uganda clinical centre of excellence (C.O.E) clinic through face to face interviews using a pretested semi structured electronic questionnaire powered by Kobo Toolbox software [26]. Potential participants were approached, informed about the study and assigned unique identifiers in a sample frame after ascertaining sexual activity. Participants were then randomly selected using Microsoft Excel generated random numbers. They were then offered consent discussions and once they gave consent, the research assistants (RAs) administered the questionnaires. Questionnaires were checked for completeness, accuracy or errors at the end of every session and then submitted. Data was downloaded and stored electronically on a password protected personal computer.
The dependent variable was reported disclosure of HIV status to sexual partners, measured on a binary scale (yes/no) while the independent variables included: socio-demographic characteristics (age, gender, marital status, religion, residence, education, occupation, employment, orphan hood status), awareness of undetected HIV viral load (VL < 200 copies per ml) being equated to un-transmissible HIV infection (U = U), caregiver/treatment supporter, behavioural factors such as relationship status, substance use, disclosure to household member(s), disclosure to a friend(s), history of gender based violence, fear of being stigmatized (yes or no) and biological factors (such as mode of acquisition of HIV as per self-report and new or old HIV diagnosis based on whether under or ≥ 1 year) among others. In addition, we assessed history of HIV testing, ART status and VL suppression status (VLSS) as per most recent test. However, VL was not a prerequisite for enrolment in the study. Except age which was a numerical discrete variable, all other independent variables were measured as categorical nominal variables.
For the quantitative study, data were analysed using STATA 14 (Stata Corp, College Station, TX, USA). Categorical variables were summarized using percentages and frequencies while numerical variables were summarized using means and standard deviations. Prevalence of HIV disclosure was summarized as proportions with their 95% confidence intervals (CI). The outcome variable was having ever disclosed one’s HIV status to the sexual partner or any of the partners if one had multiple partners with in a past period of a year. The participants were asked if they had ever disclosed to any of their sexual partner(s) and this was irrespective of the form the disclosure process took. The independent variables included socio-demographic, clinical and behavioural factors.
We used modified Poisson regression to examine factors associated with disclosure of HIV status to sexual partners. At bi-variable analysis, all factors that had p < 0.25 or had potentially reasonable association with disclosure of one’s HIV status to their partner(s) were considered for the multivariable analysis. Backward elimination was used to select which predictors to keep in our model and which to exclude using a threshold p = 0.05. Effect modification (interaction) was assessed using the Wald’s test for the generated interaction terms however none was significant thus dropped from the model. Adjusted prevalence ratios (aPR) and their 95% confidence intervals were obtained and presented in Table 2. Independent factors with p value < 0.05 at multivariable analysis were considered significant.
Study population and sampling
Some of the participants in the quantitative study were selected purposively considering maximum variation by marital status, age and sex, and asked for consent to participate in the in-depth interviews (IDIs) until there was saturation of the information given in the IDIs.
Data collection
In-depth interviews were conducted in parallel to the quantitative interviews. Using a semi structured guide, DN, a research assistant with an academic background in social sciences and experience in qualitative research conducted the in-depth interviews. The interviews were conducted in English and Luganda which is the commonly used native language. On a given day, the selected participants for the IDIs were linked to the research assistant (DN) who in a private space gave more information about the study and sought their consent to participate. Once consent was obtained, DN went on to conduct the interview. All conversations were audio-recorded and short hand-written notes were made during the interviews. Interviews audios were transcribed verbatim and translated to English as word documents for easy storage and analysis. Access to the data was limited to the concerned study team members and was stored using password protected documents.
Data analysis
Qualitative data was analysed using thematic analysis, a method used to identify, analyse, and report patterns (themes) with in data. Thematic analysis involves systematically coding qualitative data to develop meaningful themes that reflect key findings. In this study, verbatim transcription was done and the transcripts were proof-read and re-read several times for familiarization. DN and MM independently reviewed the transcripts to identify preliminary codes, which were then discussed and refined to resolve any discrepancies, leading to the development of a final codebook. The finalized codebook was applied to all transcripts using NVivo software Version 12. The coded data were then categorized into broader themes which were mapped onto the components of the health belief model using a deductive approach. Additionally, barriers and facilitators of HIV status disclosure were identified using an inductive approach. Findings were presented alongside supporting quotes from the interviews.
The mean age of participants was 21 years with 1.9 standard deviation. Majority (61.2%) were females, lived in urban areas (74.4%), from central Uganda (68.7%), and were reportedly single in regards to relationship status (73.7%) though sexually active. About 76.1% of participants had attained secondary or a higher level of education and involved in casual work (43.8%). (See Table 1).
Overall, disclosure of HIV status among participants was low at 45.2% (95% CI: 39.2–50.9). (See Table 1) Majority of those who had disclosed were female (76.4%), had a suppressed viral load (90.4%), and only slightly less than 2/3 had one sexual partner (64.6%). (See Table 2).
Adjusted for other variables (as indicated in Table 2), participants were less likely to disclose their HIV status to their sexual partners if: (1) aware that their spouse/partner was not living with HIV compared to those who knew their partners as living with HIV (aPR = 0.6, 95% CI: 0.5–0.7); (2) who had known their HIV status for more than a year at the time of the study compared to those who had known it in a year or less (aPR = 0.2, 95% CI: 0.1–0.4); (3) did not know their viral load suppression status at the time of the study compared to those who knew that they had a suppressed VL (aPR = 0.4, 95% CI: 0.1, 0.9); and (4) were not aware that with an undetectable VL, one could not spread HIV to his/her sexual partner compared to those who were aware (U = U) (aPR = 0.7, 95% CI: 0.5–0.9). On the other hand, YPLHIV were more likely to disclose their HIV status to their sexual partners if: (1) they had one or no biological parents alive as compared to those who had both parents alive (aPR = 1.4, 95% CI: 1.1–1.7); (2) had two sexual partners compared to those with three or more ( aPR = 1.7 95% CI: 1.1–2.6); (3) originated from the northern region of the country compared to the central region (aPR = 1.9, 95% CI: 1.1–3.3); (4) were Catholic or Muslim compared to those who were Anglican (aPR = 1.6, 95% CI: 1.2–2.1), (aPR = 1.6, 95% CI: 1.1, 2.3) respectively. See Table 2 below.
Barriers and facilitators of HIV status disclosure to sexual partner by YPLHIV
Out of the 16 interviewed participants, most participants (81.2%) were aged between 21 and 24 years, the males were 9 (56.2%) and females 7 (43.8%). 7 (43.8%) of the participants reported being in causal sexual relationships. Adopting the Health Belief Model, barriers or facilitators of HIV status disclosure have been organized into constructs of: perceived susceptibility and perceived severity which both contribute to the perceived threat of disease, cues to action, self-efficacy, likelihood of action, and perceived benefits vs. barriers to HIV status disclosure.
Perceived threat
The perceived threat was assessed under 2 sub domains namely:
Perceived susceptibility to consequences of non-disclosure
Some participants perceived the burden of non-disclosure was a threat to their psychological and physical wellbeing. The YPLHIV feared possible illnesses that may arise due to poor clinic appointment keeping and inability to achieve adequate ART adherence as a consequence of non-disclosure. This gave them a feeling of being susceptible to ill health and as result, this fear facilitated their disclosure to the sexual partners of some participants.
… that is the most burden of a secret that I have. I feel that if tell her I will have lifted off the heaviest load from myself. I will feel free whenever I am with her, even if it comes to taking the ARV tablet in her presence, I will be free without hiding.(20-year old male).
I really don’t even know, because by that time, I think I was not with a sound mind enough because I was too stressed, so I told her. (24-year-old female)
And if I am at his home and I have to go to hospital to pick my drugs, where will I tell him that I am going to, because you can’t tell him all the time that you are going at your parents’ home. Then I said let me tell him. (21- year-old female)
Perceived severity of non-disclosure consequences
Perceived severity in this context referred to how the young people living with HIV looked at the seriousness of the consequences of not disclosing their status to their partners. Many YPLHIV who participated in the IDIs cited that with a suppressed VL, they could live together with their partners without them contracting HIV, having learnt about undetectable VL = un-transmissible HIV (U = U). Such YPLHIV did not disclose to their partners as they perceived no serious consequence of their partners contracting HIV.
Personally, I might fail to tell her that I am living with HIV but my viral load is suppressed because I take my drugs well and I cannot spread HIV…(20-year old male).
However, some participants were worried of the consequences of non-disclosure such as loss of trust and at worst futile ending of their long-term relationships with their sexual partners. As a result, they disclosed their status to them as one of them explained:
…I thought I would get married to a person of my status because there is a boyfriend I got and my siblings did not want him for me, and they disclosed to him. Then he got very angry because I had not told him, so I told this one because I didn’t want to repeat the same mistake. (21- year- old female)
Some participants thought it was useful to disclose their positive status to the sexual partners in order to protect them from acquiring HIV through taking extra precautionary measures that reduce the risk of spreading HIV by the sexual route. This was a facilitator for disclosure to sexual partners for a number of participants
I told my girlfriend,…that I am living with HIV…, for her she is negative and me I am living with HIV, so to protect her from acquiring HIV, (20-year old male)
Moreover, some participants reported receiving encouragement from peers and healthcare providers to disclose, because many other people are living with the virus.
I am thankful because we used to have meetings here every Saturday and they helped me to take away that fear. In those meetings there was a lady who told us that, any one should not fear to disclose to his or her partner that he has HIV. (24-year-old male)
It gives them peace of mind, to know that one’s partner is also aware of their HIV status and if not living with HIV takes measures to protect themselves against contracting HIV having been disclosed to as one of them narrated:
So, she told us not to fear because even that person you meet, he or she might be positive. So, don’t fear to disclose to your partner and it also helps to reduce on the spread of HIV.… Yes, it helps in not spreading it, because that person is very aware that the person I am going to sleep with is on ARVs…(24-year old male).
Other participants deemed it necessary to disclose so as to benefit from social support and the fruits of having their partner as a treatment supporter/buddy, reminding them to take their medicines and leading healthy lives together.
It was once there but I told her because all of us we have to be healthy, such and such time you can remind me because I may be thinking of some issues or when I am busy and the time (for taking ARV medicine) reaches, I told her if the time reaches you can remind me but not in public because there might be visitors, at least you can call me privately and tell me the time has reached, I can understand it.(24-year old male)
Disclosing to one’s partner was perceived as a form of building trust and strengthening the foundation for long lasting and fruitful relationships by some YPHLIV with their sexual partners. For some, this came from previous lived experiences that they foresaw happening again if they did not disclose to their partners or if there was accidental disclosure as per the excerpts below.
… they disclosed to him, then he got very angry because I had not told him, so I told this one because I didn’t want to repeat the same mistake. (21-year old female)
Maybe the other reason which is on a positive note would be; the reason why I am being pushed to tell her is that in most cases when you tell someone and she is able to understand you, there happens to be trust. (20- year old male)
I feared that if I don’t tell her she will land on my documents because I have a book which we use, she can read it and even sees the drugs. So, I said if I hide it and she finds out, it will be very dangerous and it can make her feel bad, so that is why I told her…(23 year old male).
Also, interestingly, one participant cited that some young people use disclosure of one’s HIV status to the sexual partners as a means of ending unhealthy or financially exploitative relationships. He reported that the sexual partners might not continue with the relationship if they learnt about a partner’s positive HIV status.
There are even people who always intend to get rid of people…You can find someone, they are living with HIV, but the pressure they get from the wife prompts them to tell them the truth and for the sake of getting rid of her. (19 year old male)
Even with intentions to disclose, some participants felt there had been barriers to doing so. Some participants reported that fear of their partner's reaction prevented them from disclosing their HIV status to them. This ranged from thinking that the relationship will end, rumours being spread about their HIV status, being negatively judged or worse still they may experience intimate partner or gender-based violence and possibly death in form of homicide. These perceived possible negative effects of disclosure inhibited YPLHIV from disclosing their HIV status to their sexual partners.
I am scared and the things I am scared of are like two; I might lose her or maybe another worry is that it might not end at that/there, it (the information) might be spread to other people. Or maybe we can even breakup and she ends up saying; ‘that is why you wanted to transmit HIV to me.’ that is why I am scared when it comes to telling her.(20- year old male)
The fears carried by YPLHIV are sometimes cultivated by their friends whom they often consult regarding their decisions to disclose:
…it’s still scaring me. because I was very ready, but still I have to first get advice and every person I get…, even that friend of mine just told me don’t bother the man will kill you. (22 year old female)
Other participants, explained the fear of partner reaction to have come from their relatives, who cited possible severe consequences, while for others it was upon advice from their health care providers to delay disclosure to their sexual partners until an appropriate time. Consequently, the YPLHIV were discouraged from disclosing their HIV status to their partners.
.before going there, my grandmother told me that do you want the man to cut you into pieces after telling him or to kill you? Since then, I have never told him anything about that because my grandmother made me afraid, she told me scary words.(22 year old female)
So, when I got him, there is a counsellor here whom I consulted…… she told me when time comes you will tell him but don’t tell him now.(24-year old female)
Indeed, some YPLHIV reported experiences of strained relationships with their sexual partners after disclosing their HIV status
The relationship stayed for a bit, but it didn’t last that long and the results were not good.…. it affected our relationship, for some time. For a time being after disclosure, it was well off, it was fine, it was okay it was stable and it had no much effects but; on the later days, things changed a bit.(24-year old male)
Participants who knew that suppressed HIV viral load minimized the risk of transmission of HIV to their sexual partners (U = U), did not hold the perception that their partners would be susceptible to consequences of non-disclosure especially HIV transmission. This in return inhibited disclosure of HIV status to their sexual partners, because they believed there was no threat to their health or that of their partners.
Personally, I might fail to tell her that I am living with HIV; my viral load is suppressed because I take my drugs well and I cannot spread HIV…(20-year old male).
Yes, I thought she might not take it, and decided not to disclose to her, because I knew that I can’t transmit HIV to her. Then why would I tell her? So, I said may be with time, up to when she discovered it by herself.(24-year old male)
Some participants perceived their partners to lack of confidentiality. As a result, they opted not to disclose to them about their status for fear that they would tell their private information to none significant other persons.
… others fear to be talked about because if someone gets to know your status, some of them are not good in keeping secrets, for example if he had broken up with someone, he starts discussing your issues with other people in the community, and start to talk about you and you know how rumours move in the community.(23-year old female)
Uncertainty about society and community response, in particular stigma. They felt to be at a threat of being discriminated against and complicating their life in the community after disclosure to their partners
…there was a woman who was sick then my grandmother wanted to bring her here, so when she learnt that I also get drugs from here, she spread the information in the village and told everyone how I am living with HIV. That really made me feel bad and I said to myself like living with HIV virus is really a bad thing. So, I was there but I felt very bad and stigmatized.(21-year old female)
To some participants, the nature of their sexual relationships was a barrier to disclosing their HIV status to their sexual partners. This is because they perceived themselves to be at risk of bad outcomes of disclosure. One participant wanted to be wedded first and then would disclose to the husband about her status, others were uncertain of the outcomes of their relationships while some are in long distance relationships.
.laughs, I am waiting for everything to finish (partner to first commit and be legally bound), we first do give away (traditional pre-wedding ceremony) then we wed, ah…(24-year old female).
Some people tend to give trust when in a relationship but when they separate, they start to regret telling them certain things. To avoid that, you have to first give it time and confirm whether he/she is the right person or not.(19-year old male)
Because we are in a distance relationship, she works far from where I am and I am in Kampala and she is in another distant district. The distance; what if I disclose to her and she is far and she never returns.(24-year old male)
YPLHIV reported several pointers which intrigued and gave them the impetus to disclose their HIV status to their sexual partners. These cues ranged from initiatives by the partners to know their HIV status, mass communication such as adverts and prior accidental exposure that inspired them to disclose their HIV status to partners as illustrated by the excerpts below.
It is from that experience I had with my ex-boyfriend, because they were always encouraging us to be open to our partners and even there are adverts on TV.(22-year-old Female)
Two female participants, who had not planned to disclose narrated how they found themselves in a situation where they had no other option, but reveal to their partners:
… he asked, the pills I found, what are they for? Then I had no reason to lie again because I was not telling him, it means I was lying. So, I was open and I told him; but he knew already, that’s what I know, because he never asked me right away. If someone is to ask you and he doesn’t know, he asks you the moment he sees the pills.(22-year-old female)
We were discussing and somehow, somewhere that came up; and he was saying: ‘if I meet a woman who is living with HIV, I will stay with her’. So, I had an idea that if he can say like this, maybe I should tell him…(22-year-old female).
Some YPLHIV lacked self-efficacy and feared to discuss HIV status in front of their sexual partners. Others reported being shy and perhaps feared to be stigmatized, making it hard to open up to their sexual partners, as narrated in the excerpts below.
The first point is fear; you ask yourself how I am going to tell her, then the heart starts to beat hard, you can even meet her when you are ready to disclose to her, but due to fear you fail to tell her and change the topic. Fear is the strongest weapon that limits us from disclosing to our partners. Every time if you fear your partner, and you don’t tell him/her what transpired, fear… that’s it.(21-year old male).
This study set out to determine the prevalence of disclosure of HIV status to sexual partners among YPLHIV, the associated factors and to explore behavioural influencers using the health belief model (HBM). We found a generally low prevalence of HIV status disclosure among YPLHIV to their sexual partners which was less than half, at 45.2%. While the prevalence of HIV status disclosure among YPLHIV to their sexual partners comparable to prevalence rates of other SSA countries; 46.2% among women living with HIV in Côte d’Ivoire [27] and 40% in South Africa [17], it is considerably lower than findings of studies conducted in northern Ethiopia (63.8%) and other parts of Ethiopia (86.5% and 82.5%) [5,6,7]. It was however higher than the prevalence rates found in previous studies conducted in Kampala at 31% among YPLHIV [10] and 34% in Nairobi among women [14] in 2019. The disclosure rate in this study remained suboptimal. The difference in disclosure rates could be due to difference in the locations, age difference of the study populations and the social experiences lived. However, the low disclosure rate in this study can be partly attributed to barriers reported by YPLHIV in the study such as lack of self-efficacy to disclose and fear of the outcome such as stigma, relationship break up and intimate partner violence among others as noted in the IDIs. This implies that more efforts are needed towards promoting disclosure of HIV status to sexual partners among YPLHIV.
Though not significant at multivariable analysis, female sex was independently found to be a significant predictor for disclosure, as women were more likely to disclose too their sexual partners as compared to the men which aligns with studies conducted in other regions, such as Zimbabwe and South Africa [17, 28, 29], where women living with HIV showed a higher prevalence of disclosing their positive status to partners. This could be attributed to traditional gender roles just like gender differences were found to influence HIV status disclosure to sexual partners in East African communities in 2016 [30]. Men have poor HIV testing, care and treatment seeking behaviours [31, 32] and should be encouraged to disclose to their sexual partners using focused interventions [33]. This will improve their adherence and continuity in care.
Having ever been in a long-term relationship e.g. those who were married or later separated, was independently positively associated with disclosure of HIV status to sexual partners as it was with YPLHIV who had less than 3 sexual partners at multivariable analysis. This may be because those with less partners may be in or considering more stable and long-lasting sexual relationships sometimes leading to birth of children and hence may prefer to disclose for the sake of continuity of care and having negative children. This finding is consistent with studies conducted by Kiula and Damian in 2013 and 2019 [12, 34] and Endalamaw in 2021 [35] who reported higher rates of disclosure among individuals in long-term relationships or marriage. Therefore, long term relationships possibly resulting to marriage and having one sexual partner at ago should be encouraged among YPLHIV.
Partial or total orphan status was positively associated with disclosure of one’s HIV status to sexual partners in this study. This may be due to the need for social and financial support from their partners as compared to those with both parents alive as reported in the IDIs. This conquers with findings among YPLHIV in South Africa in which social support from the family was found to negatively affect disclosure to their sexual partners [36]. Also, YPLHIV may be prohibited from disclosing their HIV status by their parents who may be stigmatized, as disclosure by their children may imply disclosure of the HIV status of the parent for those who acquired HIV perinatally. This kind of prohibition later in life may negatively impact on one’s self-efficacy to disclose to anyone including their sexual partner(s). Parents and guardians should be encouraged to talk to YPLHIV in their care about sexual relationships in the context of the HIV epidemic and build their courage.
The longer someone knew their HIV status, the less likely they would disclose their HIV status to sexual partners. This was inagreement with findings by Adeniyi et al. in 2021 [15]. This might be a result of having a good health status which may conceal signs and symptoms of illnesses secondary to HIV/AIDs from the sexual partners, awareness of U = U and having adapted to the life of living with HIV.
YPLHIV who had no idea about U = U and those who were not aware of their most recent VL suppression status were less likely to disclose their HIV status to sexual partners. Those who had a suppressed VL disclosed better to their partners than those with detectable VL and this agreed with findings from Ethiopia by Melis Berhe et al. in 2020 [37]. YPLHIV should be educated about U = U and also empowered to always inquire about their VL results and share with partners as then they will be supported to remain in care by their partners knowing that they are protected from HIV.
YPLHIV who knew that their sexual partner’s HIV status was negative were less likely to disclose to them about their positive HIV status, which is contrary to findings elsewhere in Brazil [38]. This may be due to fear of breaking up of their relationships and intimate partner violence as expressed in the IDIs and similarly, reported by earlier studies in Ethiopia [39]. More efforts need to be directed to creating awareness in the general public to reduce stigma against PLHIV through education about U = U, the possibility of living in discordant relationships and having HIV negative children.
The barriers to disclosure of HIV status to sexual partners cited by YPHLIV which included fear of partners’ reactions after disclosure, this could have been stigma and discrimination, breaking up of relationships, intimate partner violence such as emotional violence and physical harm among others. This was similar to the reasons for non-disclosure among PLHIV in Ethiopia [39] and may explain the observed low disclosure rate in this study.
On the other hand, some participants had the will to disclose but lacked the confidence to open up about the positive HIV status before the partners while others could not confide in their partners. This may be due to low self-efficacy as a result of upbringing by the parents/guardians who may prohibit them from disclosing to anyone contrary to Maman, Van Rooyen, & Groves who found that family members may avail support in terms of disclosing the YPLHIV’s status to their partner(s) [40] as it may imply disclosure of the parents’ status as well. Hence health workers, peers and relatives have an invaluable role, assisting the YPLHIV to disclose their HIV status to their sexual partner(s) [4]. Others worry that their partners spreading rumours and discriminating against them because of their HIV status and hence not willing to disclose to them. The health workers and ministry of health have a role to fight stigma against PLHIV in the community. Surprisingly, there was hesitancy to disclose due to the confidence brought about by U = U. This could partly explain why some YPLHIV did not disclose as observed in this study and as observed in reports from earlier studies elsewhere [14, 17]. YPLHIV need to be advised and routinely reminded that their partners are better protected when they are disclosed to as then they will take necessary precautions.
The interplay between social support, family dynamics, and HIV disclosure to partners among YPLHIV is complex and underscores the importance of considering the diverse needs and experiences of YPLHIV, including those who have lost one or both parents, as well as those who have intact family support systems. Prevention of HIV transmission to the sexual partners just like in earlier studies elsewhere [17] was mentioned among the facilitators for HIV status disclosure to the partners. Proper adherence to treatment, health care providers’ and peer support [36, 37], knowledge of U = U, winning trust, discussions about HIV with partners and prospects of long term and positive relationships [35] like in earlier studies were among the facilitators of disclosure to sexual partners in this study. Health workers should benchmark on these facilitators to encourage the other YPLHIV who have not disclosed to their sexual partners to do so.
In this study, primary data collection was done and hence we were able to get as much variables and thoughts as possible from the participants [41]. The mixed methods approach employed helped to generate explanations for the observed rates of disclosure to sexual partners through triangulation of results/findings [42, 43].
However, social desirability bias was a potential limitation given the sensitive nature of the topic concerning living with HIV and sexual relationships with participants potentially providing socially and morally acceptable responses [44]. Nevertheless, efforts were made to minimize this by clearly explaining the study objectives, its importance in helping other young people living with HIV to disclose to their partners and reassuring them of confidentiality during and after the interviews.
This study revealed a generally low HIV status disclosure rate of 45.2% among young people living with HIV. Using the health belief model lens, this study shows that disclosure of HIV status is a behavioural practice, influenced by individual and environmental factors. Before deciding to disclose to their sexual partners, young people first weigh the potential benefits and risks, however disclosure may also be determined by individual and social circumstances.
Addressing potential barriers of disclosure by promoting comprehensive health education including the role of viral load suppression in reducing HIV spread, and creating supportive environments to enhance their confidence, will improve disclosure to sexual partners among YPLHIV. This will promote good adherence to ART and continuity of HIV care, improve VL suppression and reduce HIV transmission to their sexual partners.
The dataset used and/or analyzed during this study are available from the corresponding author on reasonable request.
- ART:
-
Anti-Retroviral Therapy
- C.O.E:
-
Centre Of Excellence
- IDIs:
-
In-Depth Interviews
- PIDC:
-
Paediatric Infectious Disease Clinic
- PLHIV:
-
People Living with HIV
- PrEP:
-
Pre-Exposure Prophylaxis
- UNAIDS:
-
Joint United Nations Program on HIV/AIDS
- U = U:
-
Undetectable = un-transmissible
- VL:
-
Viral Load
- YPLHIV:
-
Young People Living with HIV
Authors are grateful to the following persons for their invaluable support: the administration and staff of Baylor Foundation Uganda, C.O.E clinic, Mr. Nakedde Musa, Mr. Ronald Nabimba, Mrs. Christine Namugwanya, and Mr. Denis Ndekezi the research assistants who supported this study. Special thanks to Mr. Kelvin Bwambale, and Mr. Collins GK Atuheire for their support in quantitative analysis and Mr. Denis Ndekezi for his support in qualitative data analysis. Lastly, we acknowledge the Makerere University, Behavioral Social Sciences Research (Mak-BSSR) program and administration for their support.
The research reported in this publication was supported by the Fogarty International Center, National Institute of Alcohol Abuse and Alcoholism, National Institute of Mental Health, of the National Institutes of Health under Award Number D43 TW011304. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The Research and Ethics Committee of Makerere University School of Public Health (Mak-SPH-REC) gave approval for this research, protocol number 124 in 2022. Permission was sought from research directorate of Baylor Uganda to conduct the study at their site. Informed consent was sought from participants and unique identifiers were used during data collection for confidentiality.
Not applicable.
The authors declare no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Mugerwa, M., Namutundu, J., Nangendo, J. et al. Disclosure of positive HIV status to sexual partners among young people receiving treatment at an urban clinic, Kampala, Uganda. AIDS Res Ther 22, 40 (2025). https://doi.org/10.1186/s12981-025-00727-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12981-025-00727-7