BMC Sports Science, Medicine and Rehabilitation volume 17, Article number: 179 (2025) Cite this article
Identifying the determinants of physical (in)activity behaviour among people with spinal cord injury (PWSCI) will aid the prediction of speed and extent of recovery and inform strategies to optimise physical activity participation during physical rehabilitation. This review examined the association between socio-demographics, injury factors, and physical activity in PWSCI.
The Preferred Items for Reporting Systematic Reviews and Meta-analysis Protocols (PRISMA-P) provided the structure for this review. The epidemiological triangle and Bradford criteria further informed the review, as well as Rothman's causality model and Nweke's viewpoints. The review outcomes included injury factors and socio-demographic (intrinsic and extrinsic) factors associated with physical (in)activity in PWSCI. We searched four databases: PubMed, Medline, the Cumulative Index for Nursing and Allied Health Literature (CINHAL) and Academic Search Complete. The review used predefined eligibility criteria and a data screening and extraction template. The first author verified the extracted data. We employed narrative and quantitative syntheses and used a comprehensive Meta-analysis 4 to answer the review question.
We retrieved 4,129 articles, of which 16 (nine cross-sectional studies, six cohorts and one non-randomised clinical trial) with 2,716 participants were eligible. The mean age of participants in the included studies was 45 years, and about 14% were female. Physical (in) activity was statistically significantly associated with income (OR = 1.58, CI 1.23–2.04), completeness of lesion (OR = 0.86 CI 0.82–0.90), and mobility aid (3.12, CI 1.57–6.19). No statistically significant association existed between physical (in) activity and age (OR = 1.09, CI 0.46–2.58), sex (OR = 0.66, CI 0.43–1.03), education (OR = 0.66, CI 0.42–1.06), time since injury (OR = 0,971, CI 0,749–1,26), vertebral level of the lesion (OR = 0.92, CI 0.71–1.11), or mechanism of injury (OR = 1.48, CI 0.74–2.97) among PWSCI.
Efforts to optimise physical activity participation among PWSCI should consider the completeness of injury, income and type of mobility aid during rehabilitation programs. Factors such as employment status, residence, and type of house were less underscoring, and most studies needed more robust conceptual and theoretical underpinnings.
The review was registered with PROSPERO (ID: CRD42024544295).
Physical inactivity is a common occurrence among people with spinal cord injury (SCI) (PWSCI) [1, 2]. About half of PWSCI lead inactive lifestyles compared to a quarter of the general population [3,4,5]. Physical inactivity is a common cause of all-cause mortality and chronic diseases – notably cardiovascular disease [1]. Research recommends physical activity (PA) for people with SCI to help manage complications, including cardiovascular function and pain [6]. Twenty minutes of vigorous exercise can reduce mortality risk by 30% [7]. Compared to sufficiently active people, those who are not sufficiently active have a 20% to 30% increased risk of death [8]. Despite this, PA remains one of the neglected outcomes in the care of PWSCI [9]. There is little emphasis on the behaviour of PWSCI about their levels of PA in the rehabilitation plans [10]. Incidentally, PA is a strong predictor of mobility [11] and quality of life, reduced loneliness [12] and overall well-being [12]. The neglect of PA in both in-hospital and community rehabilitation is evident in the lack of a model for predicting PA behaviour in this patient population. A scoping of the literature shows that the prediction of PA behaviour as a treatment outcome among patients with SCI is an uncommon practice in rehabilitation plans. Comprehensive identification and stratification of the barriers and facilitators of PA among PWSCI is an essential step to creating an algorithm to assist with PA planning during in-hospital and post-discharge rehabilitation.
Several studies have reported the predictors, correlates and factors associated with PA/PIA levels in patients with SCI. Of these, impairments in physical functioning and environmental and psychological barriers have been widely investigated [3, 13]. Other independent predictors of PA participation in patients with SCI include self-regulatory efficacy, task self-efficacy, self-regulation, and social support and outcome expectations [14]. Also, factors such as outcome expectancies, social support and task-self efficacy, knowledge on how to perform tasks related to PA, planning, coping, scheduling and barrier self-efficacy have been associated with PA behaviour among people with SCI [15]. However, the increasing recognition of the biopsychosocial model of care has drawn attention to the further need to unravel the roles of non-biological determinants of health outcomes, including socio-demographic and injury factors, in PA behaviour of PWSCI [16].
Studies exploring factors associated with physical activity in PWSCI need more sound theoretical underpinning [16,17,18]. Evidence underscoring the roles of socio-demographic and injury factors in predicting PA in PWSCI are conflicting. For example, reports state a higher propensity for physical activity among younger adults with SCI than the older cohort [16,17,18]. At the same time, other authors found no association between age and physical activity behaviour/participation among PWSCI [19,20,21]. Similarly, a higher physical activity participation among male folks compared to their female counterpart was observed in some studies [2.18.19], while no such association was reported in others [16, 22, 23].
Regarding the association of injury factors with physical activity behaviour, many studies reported high levels of physical activity among individuals with incomplete lesions [2, 23,24,25,26]. In contrast, others showed no association between lesion completeness and physical activity behaviour of PWSCI [27,28,29]. Three review papers have considered factors associated with PA and exercise participation amongst PWSCI [30,31,32]. However, the included studies utilised descriptive and/or qualitative analyses without recourse to the magnitude of the identified factors contributing to PA behaviour in the study population. As expected, physical inactivity amongst PWSCI is a multivariate health outcome [30,31,32]; hence, quantifying the aggregate contributions of putative barriers and facilitators, especially the socio-demographic and injury factors, is warranted. This study will quantify each contribution to aid better PA planning during rehabilitation by indicating which factors must be adjusted and prioritised to optimise care. A systematic meta-analysis is essential, as it allows an unbiased and definitive synthesis of the differential contributions of the potential predictors in a given exposure-outcome association, thus affirming the certainty of emergent evidence [30]. Therefore, the study aims to examine the association between socio-demographic and injury factors and PA in PWSCI using a systematic review and meta-analysis design.
The review utilised three models to explore the association between physical activity behaviour and socio-demographic and injury factors in PWSCI. The epidemiological triangle informed the broad-spectrum sampling of factors linked to physical activity in PWSCI. The study used Bradford Hill's criteria and Rothman's causal pie to frame the inclusion criteria and deduction of causal inferences from the observational studies.
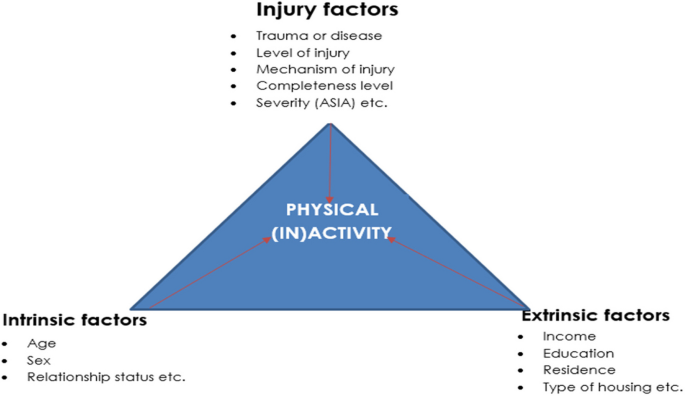
The epidemiological triangle explains the interaction between exposure and outcome. In our context, physical (in)activity is the outcome of the interaction between agent (injury), host (personal), and environmental factors [33]. It posits that an outcome arises from a disturbance in the balance among these three elements. All three factors are often necessary to trigger an outcome [32], with different outcomes requiring varying degrees of interaction [33]. Therefore, effective and holistic care measures should consider all three components and their interactions [33]. Accordingly, we sampled injury factors (mechanism of injury, lesion level, completeness, time since injury, and severity), intrinsic factors (age, sex, relationship status), and extrinsic factors (education, income, employment, residence, housing type, and mobility aid) (Fig. 1). The limitations of the epidemiological triangle in explaining the development of non-communicable diseases necessitate the use of Bradford Hill's [34] and Rothman's models.
Epidemiological triangle explaining possible associations between socio-demographic– and injury factors and physical (in)activity among PWSCI
The Bradford Hill Criteria assess causation in observational studies [35]. The framework evaluates the causal relationship between exposure and outcome using the following criteria: strength of association, consistency, specificity, temporality, coherence, biological gradient, experiment, and analogy [35]. Our study focused on the four extensive criteria: strength of association, consistency, temporality, and biological gradient.
Strength of association
Hill [36] suggests that a strong association between exposure and outcome implies causality. This criterion evaluates the strength of the relationship as crucial for establishing causality [36].
Consistency
The reproducibility of the exposure-outcome association across various populations, studies, and methodologies is termed consistency [32]. Consistent observations across different scenarios enhance the likelihood of a causal inference [34].
Temporality
Hill stated that exposure must precede the outcome to establish causality [35]. It is important to note that temporality may occur from a cohort study; our study included mostly cross-sectional and fewer cohort studies. Therefore, it is necessary to triangulate the resulting evidence to allow for a robust estimation of the association between physical activity and socio-demographic and injury factors.
Biological gradients
Defined as a dose–response relationship, it posits that the outcome changes with varying levels of exposure [34, 36]. To estimate the biological gradient, we employed the Rothman model.
Rothman’s model, or causal pie, elucidates the complex nature of exposure-outcome associations [37]. In this study, physical activity was the outcome, while the 'causal factors'/exposures were socio-demographic and injury factors. Defining the following key concepts is imperative to elucidate Rothman's model and its application. The "necessary cause" is the most recurring risk factor in developing an outcome. However, there is no absolute “necessary cause" for non-communicable diseases since two or more factors may share similar ‘pathogenicity’ [37]. A component cause is any clinically relevant risk factor of an outcome, regardless of the consistency with which it is reportedly a risk factor [38]. A sufficient cause is a mathematical set of exposures whose combinations are sufficient to induce an outcome [38]. The 'causal pie' encompasses all factor combinations leading to the outcome [37], each representing a distinct causal path [39]. Evaluating all putative exposures is essential for modelling this population's physical (in)activity behaviour [39].
The epidemiological triangle posits that physical (in)activity results from the interaction between injury (agent) factors, intrinsic (host) factors, and extrinsic or environmental factors, informing our review question and approach. This study examined the interplay between physical (in)activity and each of the injury factors, personal factors (age, sex, relationship status), and environmental factors (income, education, residence, housing type) (Fig. 1). Notwithstanding, we may not have sampled all the physical (in)activity determinants among SCI. We used quantitative data synthesis to assess each factor's clinical and prognostic importance, measuring the strength of association using the odds ratio metric. Following the criteria [36], we assessed how consistently socio-demographic and injury factors contribute to physical (in)activity among PWSCI, as measured by risk responsiveness (Ri). The Ri is the ratio of studies with statistical significance to the total studies involved in synthesising a given factor's risk estimate (odds ratio) [38]—the risk responsiveness measures of the strength of association between an exposure and outcome. Examples include odds ratio (OR), hazard ratio (HR), and relative risk (RR). In this study, all estimates were converted to OR for comparability [38]. This ratio, drawn from well-controlled epidemiological studies, ranges from 0.85 to 0.99 for excellent consistency and one for perfect consistency [40]. We estimated temporality using the study design type, and our study had a mix of cohort and cross-sectional. To determine the dose–response relationship, we applied the principle of irreversibility [40], which states that the change in exposure dosage may not permanently alter the outcome proportionally. However, an increase and a decrease in exposure dosage should not alter the outcome in the same direction. This study used the effect size (OR) direction to determine the irreversibility of the exposure-outcome association.
The review was structured following the Preferred Items for Systematic Reviews and Meta-analysis Protocols (PRISMA-P). Furthermore, the study drew perspectives from the epidemiological triangle, Bradford Hill’s criteria and Rothman’s causal pie. The frameworks were selected based on relevance and application to the deduction of causality in an exposure-outcome association [33, 35, 37]. The review was registered with PROSPERO (ID: CRD42024544295).
The population of the review included people with spinal cord injury (PWSCI) cross-sectionally or prospectively sampled. Studies were included irrespective of exposure, injury factors, and socio-demographic (intrinsic and extrinsic) factors. Hence, Studies were included irrespective of whether a comparator was employed. The secondary outcomes include study characteristics: sample size, sampling technique, setting, and outcome measures. We searched the databases from the inception of the oldest database in March 2024. The conduct of the review spanned between March and June 2024.
Eligibility Criteria
Exclusion criteria
The primary outcomes were injury factors (mechanism of injury, severity of injury, completeness of lesion, vertebral level of lesion and time since injury), intrinsic socio-demographic factors (age, sex, and relationship status) and extrinsic socio-demographic factors (employment, income, education, type of housing, residence and mobility aid). Studies were included irrespective of the physical activity measures used. Even so, only studies which employed reliable measures were involved. This study defined physical activity as physical activity, physical inactivity, sedentary behaviour, exercise capacity and participation.
We searched four databases: PubMed, Academic Search Complete, cumulative Index for Nursing and Allied Health Literature (CINAHL) and MEDLINE. Databases were searched from inception to March 2024.
The principal reviewer developed, tested, and refined the search strategy using search terms identified from the key concepts in previously published articles. The MeSH statuses of the search terms were confirmed using the Cochrane Library Advance Search. Different combinations of search terms, including MeSH and free–search terms, were included and tried using PubMed. The most appropriate search strings were retained (Appendix 1). Further, we modified the search terms to suit the syntax and subject headings of the other databases, which include Medline, Academic Search Complete, and CINAHL. Appendix 1 is a draft of the PubMed.
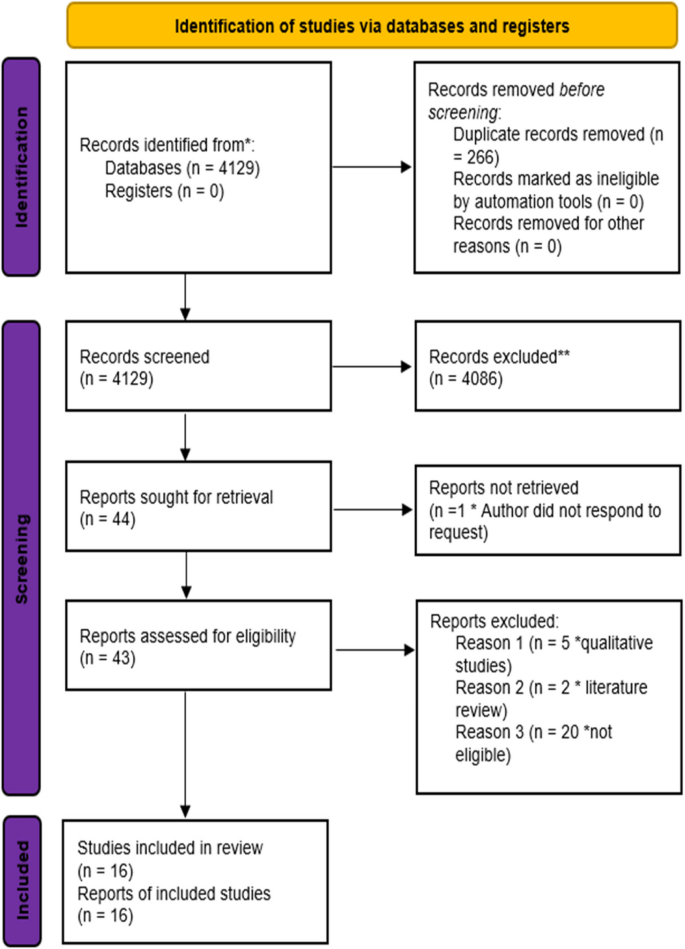
All the results retrieved from the literature search were entered into an EndNote 20 program for duplicate removal, elimination and data management. After removing duplicates, the article title and abstract were screened to determine their outcome. Included and excluded articles were organised in EndNote 20 and exported to generate the PRISMA flow chart (Fig. 2).
PRISMA Flow Diagram for the systematic review of the association between Socio-demographic factors, injury factors, and physical activity among PWSCI
Four reviewers (KB, AM, LV and AD) screened the titles and abstracts—data extractions by NM and KB. We validated the screening process through discussion and consultation with MN. We shared all eligible full-text articles among four reviewers (KB, AM, LV and AD). NM and KB collected the extracted data. The PRISMA diagram displays the details of the flow of studies throughout the selection process, as well as the rationale for exclusion (Fig. 2).
Primary data items extracted from each included study are (1) Injury factors (mechanism of injury, severity of injury, completeness of lesion, vertebral level of lesion and time since injury). (2) Intrinsic socio-demographic factors (age, sex, and relationship status) (3) Extrinsic socio-demographic factors (employment, income, education, type of housing, residence and mobility aid). (4) Measure the association between physical (in)activity and any injury and socio-demographic factors. (5) Secondary data items include study design, sample size, sampling technique and setting.
To evaluate the methodological quality of the included studies, we employed the mixed method appraisal tool (MMAT) [41, 42]. NM and AN independently carried out quality appraisals. On completion, discussions were held to resolve the discrepancies in assessments until there was a consensus on the final risk of bias ratings. This iterative process ensured that the study carried out the risk of bias assessment systematically and rigorously, enhancing the reliability of the study.
Descriptive and quantitative characteristics of the participants in the review were analysed using the mean and standard deviation. We measure the occurrence of injury and socio-demographic factors with the frequency and percentages.
Using narrative synthesis, we presented the results of the individual studies and examined the findings vis-a-vis study design and sample size. We pooled the odds ratios from eligible studies using the random-effect meta-analysis model. Where applicable, we obtained the odds ratios from study effect sizes or data [40, 43, 44]. We conducted a meta-analysis per factor of at least two studies using the Comprehensive Meta-analysis (CMA) version 4. We computed I2 to estimate heterogeneity [45, 46]. In the presence of heterogeneity, where applicable, we carried out sub-group analysis. Certainty in the body of evidence was assessed using the Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) [42]. The study characteristics were profiled using tables.
The funnel plot was visually inspected to assess publication bias. Additionally, the symmetry of the funnel plot was tested statistically using Egger’s test. A non-significant test statistic demonstrates the symmetry of the funnel plot, indicating no publication bias [42].
Certainty in the body of evidence was assessed via the Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) [42, 46]; the certainty of the evidence underpinning the exposure-outcome association was graded assessed as follows: where there were serious concerns about the possibility of bias, the grade of evidence was lowered by one level for a high risk of bias or by two levels for a moderate risk of bias [47].
Inconsistency refers to the significantly different effect estimates derived from the heterogeneity and variation in study findings. It shows the natural variations in effect estimates with less bias [48]. We evaluated inconsistency using the I2. Less than 40% was considered low, 30 to 60% was considered moderate, 50 to 90% was considered substantial, and 75 to 100% was considered significant. In the event of significant heterogeneity, the evidence was downgraded by one level [43].
The evidence supporting a research question may be implicit due to patient differences, exposures, comparisons, or outcomes. Guyatt and colleagues state that when there are significant differences between the population, comparisons, or outcomes of interest and those measured in the available evidence, the degree of certainty in the evidence is downgraded by one level [48].
Imprecision
Results with wider confidence intervals and lower precision are usually obtained from research involving small numbers of patients or events observed or a high degree of variability in patient effects [49]. A study is imprecise if its confidence interval is greater than the predefined threshold or if its data set is smaller than it could be. These factors reduce the certainty of the evidence. The result may be imprecise if the confidence intervals overlap concerning the clinically significant difference. Relative risks of 0.75 and 1.25 are used to benchmark for assessing the precision of findings [42].
Publication bias
Reporting biases may occur when studies are not fully reported in the published literature, where a claim that publication bias makes studies more eligible to be included in guidelines or systematic reviews [48]. Therefore, depending on the degree of bias, the existence of publications may lower the grade of evidence by one or two points [48].
Risk estimate
The predictive potential of a particular exposure was assessed in this study using the pooled odds ratio (RR) as obtained through meta-analysis. The quality of the evidence was rated one level higher when the risk of death is reduced or increased by at least two times; when the risk is reduced or increased by at least five times, the rating will be two levels higher [50, 51].
We retrieved 4,129 articles, of which 16 were deemed eligible. Of the 16 studies, four were from the Netherlands; two studies were in the United States of America (USA), Canada, and Switzerland. The remaining six studies were conducted in the United Kingdom (UK), Poland, Spain, Sweden, Malaysia and Denmark; the latter six studies included in the review and regarding sample size ranged from 37 to 485, where five studies had a sample size of < 50, while 11 had a sample size of > 50. The mean age of the review participants was 45 years, and about 14% were female. Concerning the sampling technique, three studies used random sampling and thirteen employed non-probability sampling techniques. Regarding study design, nine were cross-sectional studies, six were cohorts, and one was a non-randomised clinical trial. The settings of the studies were community-based (n = 11), rehabilitation centres (n = 3), and hospitals (n = 2) see Table 1.
Except for two studies with a moderate risk of bias [28, 49], all the other studies had a low risk. Evidence supporting the association between PA and each age, sex, lesion completeness, employment and severity of injury was low (Appendix 2). Evidence underscoring PA and each of education, relationship status, income, time since injury, lesion level, vertebral level of injury, and mobility aid/type of locomotion were moderate (Appendix 3).
Among the sixteen studies attached in Appendix 4, 13 reported an association between PA and age, 12 studies reported an association between PA and sex, nine reported an association between PA and education, three studies reported an association between PA and relationship status, and three reported an association between PA and income. Eleven studies reported on the association between PA and level of lesion (paraplegia vs quadriplegia), three studies reported on the association between PA and vertebral level of injury, and seven studies reported on the association between PA and lesion completeness. Five studies reported the relationship between the mechanism of injury and PA, and three studies each reported on the PA-employment and PA-mobility aid association categories (Appendix 4).
Age, sex, education and relationship status
Five studies with an average sample size of 214, primarily cohorts, reported a statistically significant association between age and PA behaviour (OR = 0.054–2.47). Eight studies with an average sample size of 112 and primarily cross-sectional found no significant association. Four studies with an average sample size of 200 and mainly cross-sectional showed a statistically significant association between sex and PA level (OR 0.49–1.30). Seven studies found no significant association. None of the studies reported a statistically significant association between education and PA behaviour. Also, none of the studies reported a statistically significant association between relationship status and PA behaviour (Table 1).
Income, residence, type of housing and employment
Three studies reported relationship status, with an average sample size of 202. The studies were mainly cross-sectional. Three studies reported on income, and none found a statistically significant association between income and PA level. The average sample size was 194. The studies were mainly cross-sectional. Two studies reported on residence, and one also reported the type of housing. None of the studies reported a statistically significant association between residence and PA behaviour. The average sample size was 92. The studies were mainly cross-sectional. The singular study that reported the type of housing found no statistically significant association between type of housing and PA (OR = 0.47 (0.15–1.48). The sample size was 70. Of the three studies that reported an association between employment and PA, one cross-sectional study with a sample size of 123 found a statistically significant association between employment status and PA participation (OR = 0.79, p = 0.03). In comparison, the remaining two studies (cross-sectional and cohort) with a combined sample size of 555 did not find any significant associations (Appendix 2).
Lesion level, time since injury and completeness of lesion
Of the eight studies that reported lesion level, two cross-sectional studies [2, 25] and one cohort [16], with sample sizes of 358, 130 and 51, reported a statistically significant relationship between time since injury and PA level. Eleven studies reported time since injury, of which only two reported statistically significant association [16, 22]. Seven studies reported on the association between completeness of lesion and PA. Three studies found a statistically significant association between lesion completeness and PA behaviour (OR = 0.39–1.55) (Appendix 2).
Mechanism of injury, vertebral level of injury and mobility aid/type of locomotion
None of the articles report a statistically significant relationship between vertebral level of injury and PA participation. Also, none of the studies reported a statistically significant association between the mechanism of injury and PA level. Four studies reported the association between mobility aid and PA, out of which two cohort studies found statistically significant associations between mobility aid or type of locomotion and PA level (OR = 0.24–0.68), while two cross-sectional found no significant association (Appendix 2).
Age, sex and education
Following meta-analysis, there was no statistically significant association between age and physical activity among PWSCI (pooled OR = 1.092 (95% CI 0.463–2.575), I2 = 80,887) (Appendix 3: Fig. 3). It suggested that physical (in)activity participation among PWSCI is not dependent on age. There was no publication bias (Egger’s t = 1.074, p = 0,332) (Appendix 3: Fig. 4). A further sub-subgroup consisting of only cohort studies showed no statistical significance [0.628 (CI 0.105–3.743)], indicating the robustness of the review finding (Appendix 3: Fig. 5). Similarly, there was no statistically significant association between physical activity and sex (OR = 0.663, 95% CI 0,427–1,030, I2 = 66.502) and education (OR = 0.663, 95% CI 0.415–1.059, I2 = 0.000) (Appendix 3: Fig. 6, Appendix 3: Fig. 7). It also suggested that the physical activity behaviour of PWSCI did not vary either with sex or education. We observed no publication bias (Egger’s t = 0,09396, p = 0,929) (Figs. 7, 8).
Relationship status and income
There was no statistically significant association between relationship status and physical activity among people with SCI (pooled OR = 0,892, 95% CI 0,716 to 1,112, I2 = 89,16) (Appendix 3: Fig. 9). The inclusion of a few studies disallowed sensitivity or sub-group analysis. Also, we found no statistically significant association between income and physical activity among people with SCI (pooled OR = 1,582 (95% CI 1,225–2,044), I2 = 0.000) (Appendix 3: Fig. 10). In addition, there was publication bias (Egger’s t = 0,24532, p = 0,84685) (Appendix 3: Fig. 11), indicating that neither relationship status nor income status influenced the physical activity behaviour of PWSCI.
There was a statistically significant association between lesion completeness and physical activity among PWSCI (pooled OR = 0,860, 95% CI 0,822–0,900, I2 = 0.000) (Appendix 3: Fig. 12). The higher the lesion level, the lower the propensity for physical activity. No publication bias was observed (Egger’s t = 0,79401, p = 0,57,278) (Appendix 3: Fig. 13). There was no statistically significant association between physical activity and time since injury (OR = 0,97, 95% CI 0,75–1,26, I2 = 0.00) (Appendix 3: Figs. 14 & 15) and vertebral level of injury OR = 0,917, 95% CI 0,71–1,109, I2 = 0.00) (Appendix 3: Figs. 16 & 17). There was no publication bias for each exposure-outcome association (Table), meaning that time since injury and vertebral level of injury did not influence the physical activity behaviour of PWSCI.
There was no statistically significant association between physical activity and mechanism of injury (pooled OR = 1,480 (95% CI 0,737–2,971) (Appendix 3: Fig. 18). The fact that there were two studies limits sensitivity or sub-group analysis. In addition, there was publication bias (Egger’s t = 15,7121, p = 0,0405), I2 = 20.978) (Appendix 3: Fig. 19). Similarly, no statistically significant association was reported between lesion level and physical activity among people with SCI (pooled OR = 2,31 (95% CI 0,35–15,29), I2 = 89,160) (Appendix 3: Fig. 20). Also, the fact that there were two studies limits sensitivity or sub-group analysis. We found a statistically significant association between mobility aid and physical activity among people with SCI (pooled OR = 3.117 (95% CI 1.570–6.187), I2 = 28.589) (Appendix 3: Fig. 21). In addition, there was publication bias (Egger's t = 0,306, p = 0,81) (Appendix 3: Fig. 22), signifying that the physical activity level of PWSCI varies depending on the type of mobility aid used. Individuals who use manual wheelchairs were more active than their counterparts who use electric wheelchairs.
All of the studies possessed a low risk of bias apart from Baehr et al. (2022) and Handlery et al. (2024), which possessed a moderate risk of bias. Evidence supporting the association between PA and each age, sex, lesion completeness, employment and severity of injury was low (Appendix 2). Evidence underscoring PA and each of education, relationship status, income, time since injury, lesion level, vertebral level of injury, and mobility aid/type of locomotion were moderate (Appendix 4).
The study explored the association between physical activity and socio-demographic and injury factors amongst PWSCI as here discussed:
The finding was that there was no significant association between age, sex, education and PA among PWSCI, which suggests that age, sex and education may not be important determinants of PA behaviour among people with SCI. Interestingly, these findings were reported with a fair degree of consistency (N-factor = 0.5). However, the fact that temporality could not be established as 40% of the studies were cross-sectional indicates the need for more cohort studies. Biological gradient is not applicable since there was no significant association between age and PA in people with SCI. Our findings showed a similar physical (in)activity distribution between young and older adults with SCI, contradicting the idea that physical activity declines with age [50], female gender [52, 53] and less education [56.57]. However, the disparity could be because our study involved people with SCI instead of the general population studied in [50]. Spinal cord injury significantly impairs functional capacity, and being young or old, male or female, educated or uneducated may not serve a critical prognostic function. Although it could be significantly different, we have confidence that the actual effect will likely be similar to the evidence espoused in this study.
The fact that relationship status was not associated with physical activity among people with SCI suggests that physical inactivity is equally common in people with SCI in a marital relationship/partnership as well as those in no such relationship [54]. The finding contradicts the notion that physical activity increases when married in the general population [55, 47, 56]. Therefore, it is possible that their partners may not know much of the benefits of PA or patients are not motivated to engage in PA as a high rate of probable depression, as much as 63.9%, has been reported among PWSCI [20, 57]. The positive association between income and PA among people with SCI implies that the propensity for PA increased with increasing income. A consistent finding stated positive physical activity behaviour among PWSCI with higher income than their lower-income counterpart [23, 28].
Interestingly, there was a perfect consistency across studies. However, the fact that two out of three cross-sectional studies disallows causal inference since temporality could only be partially established. We have a reasonable degree of confidence that the actual effect will likely be similar to the estimate obtained in this study. However, it may be changed with further research, especially cohort studies.
The significant association between completeness of lesion and PA among individuals suggests that the level of the lesion may serve as an important prognostic factor for PA behaviour among people with SCI. The finding aligns with findings that participation was higher in PWSCI with incomplete injury compared to those with complete injury [24]. However, the finding was reported to have much inconsistency (N-factor = 0.33). In addition, the fact that temporality could not be established as all three studies were cross-sectional indicates the need to explore further the association between completeness of injury and PA among PWSCI using cohort designs. Regarding biological gradients, the findings of the three studies were in the same direction, suggesting that the propensity for physical inactivity was higher in individuals with complete lesions.
Furthermore, it contributes to the definiteness of the association between completeness of injury and PA among PWSCI. While we could not establish the association's temporality, the completeness of injury level may serve an essential prognostic function in planning PA interventions for PWSCI. Although it could be significantly different, we have confidence that the actual effect will likely be similar to the evidence espoused in this study.
The lack of significant association between each of the injuries and vertebral level of injury and PA among PWSCI suggests that these factors may not be necessary when modelling PA behaviour among people with SCI. Interestingly, these findings were reported with perfect consistency. With two of the three studies being cohort, it is almost certain that time since injury is not a prognostic indicator for PA behaviour among PWSCI. Although all three studies investigating the association between vertebral level of injury and PA were cross-sectional, the lack of association reduces the need for further exploration using cohort studies. The functional capacity of PWSCI does not vary with how long a person has lived with SCI [16, 23], nor does it matter whether the injury is cervical, thoracic or lumber [24, 28]. Instead, what counts is the level of completeness of the lesion. We have a reasonable degree of confidence that the actual effect will likely be similar to the estimate obtained in this study. However, it may be changed with further research, especially cohort studies.
The causes of SCI are classified into traumatic and non-traumatic [21, 57]. We found no significant association between the mechanism of injury and PA in people with SCI. Interestingly, there was consistency across the three studies [2, 15, 23], and the fact that one of the studies was a cohort lends credibility to the result that PA behaviour did not differ with the mechanism of injury. While there was no significant association between mobility aids, substantial heterogeneity and inconsistency call for further exploration. In addition, of the three studies, the two cohort studies [23, 25] reported a significant association between mobility aid and PA, thus questioning the finding that mobility aid did not determine physical activity behaviour. Following the principles outlined in the conceptual and theoretical framework, we argue that mobility aid was an important determinant of PA among PWSCI.
Regarding the gradient of that association, individuals with manual wheelchairs consistently recorded more positive physical activity behaviour than those who used an electric wheelchair or wheelchair with support [23, 25]. Biomechanically, this is plausible as it resonates with the finding that individuals with complete lesions who were more inclined to receive support on mobility were more likely to be physically inactive [24, 58]. The certainty of the underlying evidence is moderate, indicating that the evidence may change with further research.
This review's strength lies in applying appropriate conceptual and theoretical frameworks to inform the review method and discussion of findings. Meta-analysis was an additional strength. However, the limited number of studies and the fact that most included studies were cross-sectional constitute limitations to the review findings. Cross-sectional studies are traditionally weak and designed to estimate risk factors and disease determinants. Also, the small number of eligible studies indicates that the emerging evidence needs to be more conclusive, as further research could alter the current evidence position. However, without a well-controlled cohort, the outcomes from the available cross-sectional studies are helpful to inform hypothesis generation and guide further research. It could serve as an initial guide to rehabilitation clinicians on what factors to modify to improve physical activity participation among PWSCI. Furthermore, the substantial heterogeneity recorded with some factors constitutes a limitation. However, we undertook a sub-group analysis to explain the possible cause of heterogeneity.
With our result showing the association between physical activity and each of lesion completeness, income and mobility aid, we postulate that participation in physical activity among PWSCI is directly proportional to income and degree of use of manual wheelchair but indirectly proportional to the lesion completeness, i.e. [PA level = income * use of manual wheelchair] / [severity in terms of lesion level]. In other words, the physical activity behaviour will improve as patients' income (social/financial support) increases but will be negatively impacted when a high lesion level (cervical lesion) is involved, provided that physical activity is given considerable attention during the rehabilitation with emphasis on early mobilisation and training on wheel use.
In the meantime, efforts to optimise physical activity participation among people with SCI should consider factors such as completeness of injury, income and type of mobility aid during rehabilitation plans. First, there is a need for a renewed emphasis on the health benefits of physical activity in terms of health and disease among PWSCI and their caregivers. Every minute of physical activity promotes a healthy life and longevity [57]. Strategies to improve physical activity uptake among PWSCI, mainly targeting modifiable factors such as income (social support) and early training on using manual wheelchairs, should be prioritised. Where a manual wheelchair is limited, using an electric wheelchair should be completed by regular exercise using a resistance-free bearing arm ergometer. For example, providing financial protection through insurance may facilitate access to healthcare services and specialist care, such as physiotherapy among PWSCI, on a long-term basis. By extension, reduced out-of-pocket expenditure could promote access to moderate residential apartments, incentivising physical activity participation among people with disabilities. Clinicians and caregivers should prioritise activities targeted at gaining upper limb functional independence and cardiorespiratory fitness, as this will improve their wheelchair-use efficacy. Manual wheelchair practice should commence as early as possible, and wheelchair use should be encouraged and monitored during and after in-rehabilitation. Also, the attention of policymakers to the role of built environments in facilitating the inclusion of persons with disability should be pursued more vigorously, especially in low– and middle-income countries where access to wheelchair-supportive environments is limited.
One of the most critical gaps revealed in this review is the need to develop a valid and reliable measure of physical (in)activity among people with SCI. While the accelerometers hold a promise, the inability to differentiate steps or arm effort from wheel cadence constitutes a severe limitation. At the same time, most of the subjective measures, including the Physical Activity Recall Assessment for People with SCI questionnaire PARA-SCI and LTPAQ-SCI, have shown poor validity, especially for mild physical activity, which constitutes a significant proportion in this patient group [59, 60]. The preponderance of cross-sectional studies disallows the establishment of temporality and causality. Therefore, more cohort studies are required to investigate the exposure-outcome relationship further, particularly the association between completeness of lesion, income, mobility aid, and physical activity among PWSCI. Factors such as employment status, residence, and type of house, among others, were less reported, indicating that the conduct of most of the studies needed more robust conceptual and theoretical underpinnings. We recommend further studies targeting the improvement of the validity of the subjective measures of PA in this patient group as a necessity. Further studies should employ a longitudinal design to explore the association between injury, personal and environmental factors and PA in people with SCI. Finally, we recommend that future studies exploring the factors associated with physical (in)activity among people with SCI should be based on a sound conceptual and theoretical underpinning, preferably drawing perspectives from the epidemiological triangle, Bradford Hill's criteria and Rothman's model, thus allowing a comprehensive sampling of additional factors.
Factors such as completeness of injury, income, and type of mobility aid were associated with physical activity participation among PWSCI. Given the level of certainty involved, this evidence may change with further research. In the meantime, we postulate that higher income and manual wheelchair use facilitate physical activity among PWSCI, whereas lesion completeness constitutes a barrier. The use of theoretical guidance thoroughly examines the association between physical activity and socio-demographic and injury factors, resulting in rigorous and valid findings. However, the postulation might change as more longitudinal studies emerge.
Study data will be available upon reasonable request.
- LTPAQ-SCI:
-
Leisure-time Physical Activity Questionnaire for People with Spinal Cord Injury
- PA:
-
Physical Activity
- PACDPAI:
-
Leisure Time Physical Activity Index
- PARA-SCI:
-
Physical Activity Recall Assessment for People with SCI Questionnaire
- PASIPD:
-
Physical Activity Scale for Individuals with Physical Disabilities
- PIA:
-
Physical Inactivity
- PWSCI:
-
Persons with Spinal Cord Injury
- SCI :
-
Spinal Cord Injury
- TSI:
-
Time Since Injury
- WHO:
-
World Health Organization
The authors acknowledge Professor Joyce Mothabeng for envisioning us to carry out this review.
This research did not receive a grant, funding or sponsorship from a funding agency in the public, commercial, or not-for-profit sectors, nor individuals.
Not applicable.
Not applicable.
The authors declare no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Nweke, M., van Vuuren, M., Bester, K. et al. Association between socio-demographic and injury factors, and physical activity behaviour in people with spinal cord injury: a theory-informed systematic review and meta-analysis. BMC Sports Sci Med Rehabil 17, 179 (2025). https://doi.org/10.1186/s13102-024-01021-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13102-024-01021-1