Assessing the effectiveness of continuous glucose monitoring compared with conventional monitoring in enhancing surgical outcomes for patients with diabetes: protocol for a multicentre, parallel-arm, randomised, pragmatic trial in China
Diabetes and endocrinology
Assessing the effectiveness of continuous glucose monitoring compared with conventional monitoring in enhancing surgical outcomes for patients with diabetes: protocol for a multicentre, parallel-arm, randomised, pragmatic trial in China
Introduction The Comprehensive Complication Index (CCI) is an internationally recognised indicator of postoperative complications. During the perioperative period, patients with diabetes mellitus (DM) or impaired glucose tolerance (IGT) may experience a significant increase in the CCI associated with glucose-related complications and increased mortality. Continuous glucose monitoring (CGM) offers advantages such as portability, accuracy, real-time monitoring and rich information. However, few large-scale studies have investigated the effectiveness and safety of CGM in reducing CCI during major surgeries.
Methods and analysis This study is a multicentre, parallel-arm, randomised pragmatic trial to investigate whether CGM improves clinical outcomes in patients with type 1 or type 2 DM or IGT undergoing major surgery relative to conventional monitoring. This study is planned to be conducted in 50 secondary or tertiary hospitals in China. Eligible patients aged 18 years or older with DM or IGT undergoing elective major surgery will be recruited during a baseline screening period of 3 days before surgery. Eligible patients will be randomly assigned to receive CGM or conventional monitoring in a 1:1 ratio. The primary endpoint measure is the CCI score within 30 postoperative days. The margin of superiority is −12.0. A total of 10 168 participants will achieve 90% power to detect a clinically important difference of −13.0 between the means in the primary outcome. This trial includes multiple statistical analysis steps. For the primary outcome, a covariance model will be used to compare the difference in CCI within 30 days postoperatively between the two groups after adjusting for baseline and centre effects.
Ethics and dissemination This trial has been approved by the Ethics Committee of Beijing Tsinghua Changgung Hospital (No. 23684-0-02) and its corresponding branch centres. Informed consent will be obtained from all subjects involved in the study. The primary trial results will be submitted for publication to a peer-reviewed journal.
http://creativecommons.org/licenses/by-nc/4.0/
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Diabetes mellitus (DM) is a serious health problem with alarming levels worldwide. The International Diabetes Federation estimates that by 2045, the number of people aged 25–79 years with DM will reach 783 million worldwide. China has approximately 174 million patients with DM, which is the highest number of patients with DM worldwide.1 According to cross-sectional data from 31 representative provinces between 2015 and 2017, the prevalence of DM in China was 11.2%.2 With the increasing prevalence of DM, the proportion of patients with DM undergoing surgical procedures has increased. DM is an independent risk factor for adverse postoperative outcomes (OR, 1.653; 95% CI, 1.487, 1.839).3 Additionally, approximately 50% of patients are not diagnosed with DM before surgery,4 indicating that uncorrected glucose metabolism disorders are often present during the perioperative period, along with factors such as preoperative fasting, surgical stress and glucocorticoid use5; thus, perioperative blood glucose dysregulation frequently occurs with various types of surgeries.6 7
Blood glucose dysregulation includes hyperglycaemia, hypoglycaemia and high glycaemic variability, all of which can lead to glucose-related adverse reactions, including infectious complications such as pneumonia, surgical site infections (SSIs), urinary tract infections, acute myocardial infarction, brain damage (eg, delirium and stroke), prolonged hospital stays and overall negative impacts on patient outcomes.8 Therefore, effective blood glucose management is key to reducing postoperative glucose-related complications. Based on blood glucose management targets, management can be categorised as tight or conventional glycaemic control. In 2001, a milestone study revealed that maintaining strict blood glucose levels (80–110 mg/dL) in surgical intensive care unit (ICU) patients facilitated a reduction in the incidence of complications and mortality.9 This finding has increased interest in blood glucose control in surgical patients and sparked several related studies. However, subsequent large-scale randomised controlled trials on strict glycaemic control failed to replicate these benefits, indicating a significant increase in the risk of hypoglycaemia.10 11 It is speculated that the main reasons for this discrepancy in results are the inclusion of non-surgical patients, inconsistencies in blood glucose targets and variations in treatment protocols.12 A meta-analysis of perioperative blood glucose control in patients with DM showed that strict glycaemic control reduced the risk of infectious complications (risk ratio (RR), 0.35; 95% CI, 0.19, 0.63), as well as the risk of renal dysfunction (RR, 0.38; 95% CI, 0.15, 0.95). However, strict glycaemic control was also associated with a higher risk of hypoglycaemia (RR, 3.00; 95% CI, 1.97, 4.55),13 potentially resulting in cardiovascular complications, neurocognitive dysfunction and even death.14–16
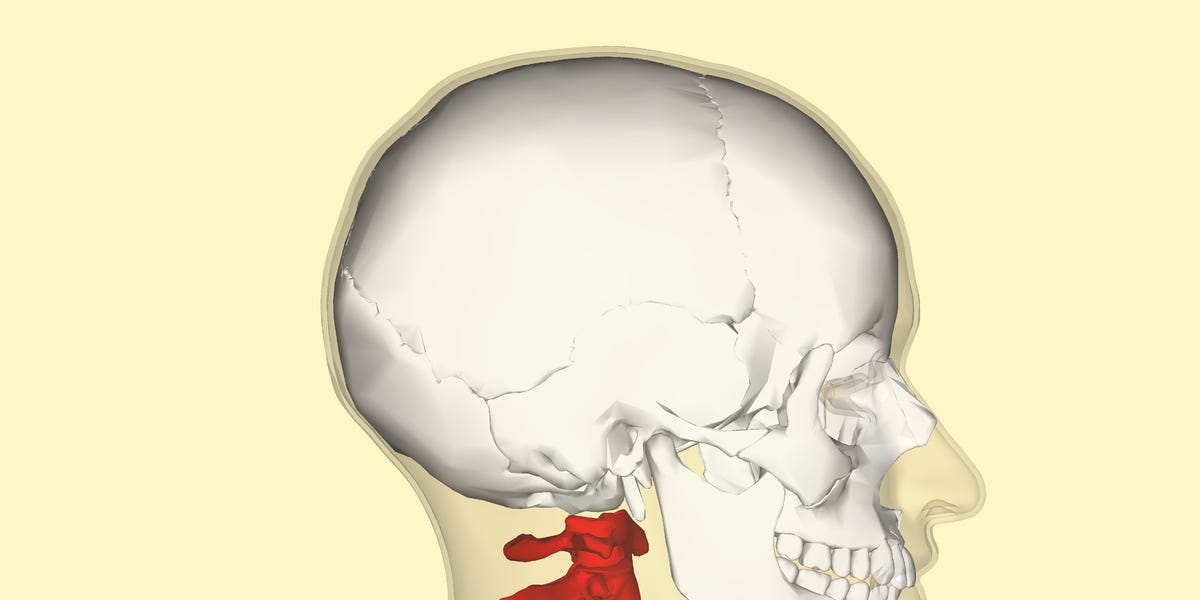
Regarding the high risk of hypoglycaemia associated with strict glycaemic management, one consideration is that current clinical practice still relies principally on traditional intermittent arterial blood gas, venous or fingertip blood tests for perioperative blood glucose monitoring. These monitoring methods are not continuous and can lead to missed information and a lack of predictive ability for hypoglycaemia or hyperglycaemic risks. Furthermore, frequent monitoring not only increases personnel and resource costs but also adds to patient discomfort. Since the American Diabetes Association first introduced continuous glucose monitoring (CGM) into clinical practice in 2018,17 the accuracy of these devices has gradually improved, creating an exciting new research area. Considering the risk of hypoperfusion affecting subcutaneous flow, CGM devices do not fully reflect blood glucose levels. The mean absolute relative difference for current personal CGM systems is approximately 10.4%,18 which remains within the clinically acceptable range. CGM devices monitor interstitial fluid glucose levels every 5 min, providing real-time glucose readings. They used analysis software to transform these data into continuous visual glucose concentration maps, providing more detailed glucose information. These data reflect the direction and speed of glucose changes, enabling patients and healthcare professionals to respond immediately to mitigate or prevent acute glucose events.
The clinical efficacy and safety of CGM in patients with DM have been confirmed in numerous studies. In a randomised controlled trial, researchers demonstrated that CGM increased the time spent by patients with type 1 DM who had impaired awareness of hypoglycaemia in the normal glucose range and reduced the frequency of severe hypoglycaemia.19 For type 2 DM receiving insulin, Beck et al found that CGM could improve glycaemic control and may benefit these patients.20 Similarly, an umbrella review revealed that CGM could also lead to better clinical outcomes than self-monitoring of blood glucose (SMBG), and it was recommended that the introduction of CGM into standard care alongside SMBG for type 2 DM.21 Furthermore, while the accuracy of CGM devices may vary, their sensor survival rates exceed 80%, indicating a high level of technical reliability. Adverse effects are minimal, primarily involving mild erythema.22
The studies reported thus far have primarily focused on the use of CGM in the management of nonsurgical patients with DM. Carlsson et al used CGM for perioperative glucose monitoring in patients undergoing major surgery and found that despite standardised perioperative glucose management, the frequency and duration of both hyperglycaemia and hypoglycaemia remained high, particularly in patients with DM.23 Therefore, CGM-driven perioperative glucose management has the potential to benefit patients with DM.24 Some researchers have suggested that CGM enables intensive glucose monitoring, significantly reducing the average intraoperative blood glucose levels, glycaemic variability, postoperative C-reactive protein (CRP) levels and incidence of SSIs compared with traditional glucose management protocols during the perioperative period.25 26 Although CGM provides reliable technological support for precise glucose management and shows great potential for perioperative glucose management, these studies had relatively small sample sizes, industry sponsorship and short durations, which may affect the accuracy of the results.27 In addition, given the potential limitations of CGM, there is a paucity of comprehensive perioperative data on the use of CGM technology to enhance perioperative care.28
Furthermore, with the introduction of diagnosis-related groups (DRGs), the quality control of surgery has become increasingly important. The DRG encompasses the total cost of care (including postoperative nursing), and complications are the biggest drivers of cost increases. In 2013, Graf et al29 introduced a Comprehensive Complication Index (CCI) that integrates the number and severity of postoperative complications into a single score. Compared with the classical Clavien-Dindo classification (CDC) for postoperative complications, the CCI provides a better assessment of the overall burden of complications, allowing for a more objective evaluation of surgical quality. Several subsequent studies validated its effectiveness.30–32 However, no real-world research has reported the impact of CGM-driven perioperative glucose management on CCI. Therefore, we will herein determine the impact of CGM on the prognosis and CCI improvement in patients with DM (type 1 or type 2) or impaired glucose tolerance (IGT) when used for perioperative glucose monitoring in a real-world setting.
Our primary objective is to observe the improvement due to the application of CGM on the CCI of individuals with type 1 or 2 DM or IGT. Our secondary objective is to analyse the improvement in surgical outcomes of the study population with CGM based on different factors such as age, surgical type, type of DM, preoperative haemoglobin A1c (HbA1c) level and preoperative blood glucose variability within a 24-hour range. Our exploratory objective is to evaluate the difference in overall postoperative infection rate, major adverse cardiovascular event (MACE) rate, brain damage (eg, delirium and stroke) and shortened postoperative hospital stay within 30 days after surgery between the two groups.
This is a multicentre, two-parallel-arm, randomised pragmatic study initiated by the researchers with a 1:1 allocation ratio. The research protocol for this study was developed according to the Standard Protocol Items: Recommendations for Interventional Trials recommendations for interventional trials33 and has been registered at https://www.clinicaltrials.gov (NCT06331923). Beijing Tsinghua Changgung Hospital serves as the leading centre for this project. The study is planned to be conducted in 50 secondary or tertiary hospitals in China (online supplemental material 1). These hospitals include both traditional Chinese medicine and Western medicine hospitals, as well as specialised and comprehensive hospitals. Hospitals are distributed across 19 provinces and cities in China and provide a wide range of medical services for patients with DM or IGT.
The study consists of a screening period of 1–3 days before surgery, an intervention period of 7 days and a final evaluation performed on the 30th day. The researchers will make every effort to conduct the necessary observations and evaluations of the participants who withdraw from the study to complete the specified early termination visits. This study does not include any replacement for withdrawal.
This study will focus on patients with type 1 or 2 DM or IGT who underwent major thoracic/abdominal surgery (excluding cardiac surgery), open orthopaedic surgery or neurosurgery. The inclusion, exclusion and withdrawal criteria are presented in table 1.
Table 1
Inclusion, exclusion and withdrawal criteria
The required sample size will be estimated using pragmatic tests. A 10-point difference in the CCI is analogous to a one-grade shift in the CDC.34 This difference can be illustrated by comparing a urinary tract infection requiring antibiotics (CDC Grade II) to a transient elevation of serum creatinine (CDC Grade I) or a transient ischaemic attack requiring anticoagulation therapy (CDC Grade III) to transient confusion without the need for therapy (CDC Grade II). Based on this, we consider a decrease of 12 points in the CCI as clinically significant. According to domestic and international literature surveys, it is estimated that the CCI of patients with DM within 30 days after major surgery is approximately 27.93±16.50 points.35 36 According to the preliminary results from Beijing Tsinghua Changgung Hospital, we hypothesise that CGM-driven glucose management will reduce the CCI of patients with DM within 30 days after surgery to 14.93±11.10 points.
Group sample sizes of 4067 in the CGM group and 4067 in the control group will achieve 90% power to detect superiority using a one-sided two-sample t-test (online supplemental material 2). The margin of superiority is −12.0. The true difference between the means is assumed to be −13.0. The significance level (alpha) of the test is 0.025. The data will be drawn from populations with SD of 11.1 and 16.5, and to allow for 20% attrition, we will include 10 168 patients, with 5084 patients in each group.37 38
Extensive stratification could introduce logistical challenges and potentially compromise feasibility and quality control in a large-scale multicentre trial. Our study prioritises stratification by HbA1c levels due to its direct impact on glycaemic control, a central factor in our research question. Patients who fulfil our enrolment criteria will be randomly assigned to receive CGM or conventional glucose monitoring according to a centralised randomisation schedule in blocks of 10, stratified by HbA1c level at baseline (≥6.5% vs <6.5%), to achieve between-group balance at baseline. Subjects will be assigned the next available treatment number within the block. The absence of block size information in the protocol is intentional to ensure that any investigator involved in the study cannot predict the allocation of participants to the treatment group. The follow-up assessors, statistical experts and safety committee will be unaware of the results of the randomisation process until the completion of the data analysis. However, the investigators involved in implementing the intervention measures and perioperative care, as well as the study participants, will not be blinded.
This intervention involves the application of CGM to manage perioperative blood glucose levels, which will be compared with conventional glucose management methods.
CGM group: CGM (RGMS-III, Huzhou Meiqi Medical Equipment) prescriptions will be issued by the attending physician at least 6 hours before surgery. The primary nurse in charge informs the patients and their family members of how to properly wear the CGM device. Glucose information will be transmitted to attending physicians every 3 min via handheld devices or smartphones. The calibration frequency and interval of the preoperative and postoperative glucose monitoring devices will be determined based on the institutional diagnostic and treatment guidelines of each centre and the requirements of the monitoring device used. Intraoperative glucose calibration will be performed immediately on admission, immediately after surgical incision, every 2 hours after surgical incision and after wound closure.
Control group: Perioperative glucose monitoring will be conducted based on the institutional diagnostic and treatment guidelines of each centre.
Glucose/blood glucose monitoring will be continued in both groups until postoperative day 7 or until discharge. The effects of glucose and insulin will be observed for 15 min before administering another dose. Perioperative glucose management in both groups will be as follows:
Postoperatively: The target range for early postoperative blood glucose management is 4.5–7.8 mmol/L. Based on institutional diagnostic and treatment guidelines and the clinical experience of the attending physician, if the blood glucose level is ≤4.5 mmol/L, glucose infusion will be administered to raise the blood glucose level. If the blood glucose level is ≥7.8 mmol/L, insulin will be administered to lower the blood glucose level. In the intervention group, if it is found that the blood glucose variability is excessively high (including a coefficient of variation (CV) ≥36%, LAGE ≥4.4 mmol/L, postprandial glucose excursions of three meals ≥2.2 mmol/L, SD of blood glucose ≥2.0 mmol/L or time in range ≤70%), an endocrinology specialist will assist in adjusting the blood glucose management plan.
Eligible participants will be enrolled between April 2024 and October 2025 (the participant timeline is illustrated in figure 1). During the screening period of 1–3 days and before randomisation, baseline information will be collected during ward visits. This information will include demographic information, diagnosis, medical history, comorbidities, existing symptoms and signs, physical examinations, laboratory parameters, auxiliary examinations and disease severity (including New York Heart Association (NYHA) classification, Charlson comorbidity index and American Society of Anesthesiologists (ASA) classification). After the participants have signed the informed consent form (online supplemental material 3), they will be informed about precautions and potential adverse events associated with wearing the CGM device. The research intervention will be implemented before the surgery (visit 0). During each visit for assessor blinding and follow-up (visits 1–8), outcomes and adverse events (AEs) will be assessed accordingly. The inclusion, intervention and assessment timelines are presented in online supplemental material 4.
The CCI score within 30 days postoperatively is the primary endpoint measure. The CCI is a validated prognostic assessment tool that calculates the total score of all complications weighted by severity, ranging from 0 (no complications) to 100 (death) for each patient.29 39 In this study, the cumulative CCI values of all postoperative complications within 30 days postoperatively for each patient will be calculated using the CCI Online Calculation Tool (www.assesssurgery.com).
Secondary outcomes are postoperative complications (classified based on CDC grades) at 1–7 days postoperatively and the 30-day follow-up,40 mortality at 30-day follow-up, perioperative glucose levels (assessed from the day of enrolment to 7 days postoperatively), length of stay in the ICU and overall hospitalisation cost.
Exploratory outcomes are overall postoperative infection rate, MACE rate, brain damage (eg, delirium and stroke) and length of hospital stay within 30 days after surgery. Brain damage will be assessed through clinical manifestations, auxiliary examinations and relevant scales, such as Richmond Agitation-Sedation Scale (RASS), Confusion Assessment Method (CAM) and National Institute of Health Stroke Scale (NIHSS). When the participant is discharged from the hospital, the length of stay in the ICU and hospital as well as the cost will be evaluated.
Analysis sets
All randomised participants will be analysed to describe the distribution of the baseline data.
All analyses of efficacy endpoints, also known as the full analysis set, will be conducted based on the intention-to-treat principle.41 42 This includes all randomised patients who had evaluable baseline information, received at least 3 days of glucose monitoring (CGM or conventional monitoring) and had at least one visit with assessable follow-up data.
The per-protocol population of this study will consist of participants who have completed relevant observations as required by the study protocol and meet the following criteria: (1) use of glucose monitoring (CGM or conventional monitoring) for 7 days, (2) meet the inclusion criteria and (3) complete all planned visits and fulfil the required data in the Electronic Data Capture (EDC) system.
Safety evaluations will be performed on all participants who undergo glucose monitoring (CGM or conventional monitoring) and have available follow-up information for safety analyses. All safety information recorded by the study participants, including AEs and laboratory parameters, will be evaluated.
Statistical analysis plan
Continuous variables are presented as mean±SD, conforming to the normal distribution, and median (IQR; or minimum, maximum) for skewed distribution data. Categorical variables will be expressed by the number and percentage of occurrences. The group t-test and Wilcoxon rank-sum test will be used to test the differences in continuous variables, where appropriate. Differences between the two groups will be compared using the χ2 tests or Fisher’s exact probability test for categorical variables.
The primary outcome measure is the CCI score within 30 days of surgery. Between-group comparisons will be conducted using the aforementioned statistical methods for continuous variables. After adjusting for baseline and centre effects, a covariance model will be used to compare the difference in CCI within 30 days postoperatively between the two groups and to calculate between-group differences in the least square mean and 95% CI. Furthermore, the consistency of treatment effects across study centres will be examined by adding an interaction term for the study centre and treatment group in the covariance model.
Time-to-event endpoints of secondary outcomes will be analysed using Kaplan-Meier survival analysis and compared using the log-rank test.
We will implement a Cox proportional hazards regression model to calculate the hazards risk (HR) between the two groups and its 95% CI. Subgroup analyses will be performed in the following subgroups: age (<65 years vs ≥65 years), high glycaemic variation (yes vs no), HbA1c (<6.5% vs ≥6.5%), type of DM (type 1 vs type 2) and type of surgery for all the efficacy endpoints. We will use SAS software (V. 9.4) to conduct all analyses.
Participants who do not complete the study or are lost to follow-up will be coded as having treatment failure, and missing values will be handled using the multiple imputation method under the missing-at-random assumption.43
We define AEs as any unexpected and unfavourable medical event related to any medical intervention in the study, regardless of whether it is associated with the use of the CGM device. Adverse events include unexpected or inappropriate signs (including abnormal laboratory findings), symptoms or transient illnesses related to the use of the product. We define a serious AE as an adverse event that meets at least one of the following criteria: death, hospitalisation or prolongation of existing hospitalisation, life-threatening or severe disability, or medical intervention to prevent any of the above-mentioned outcomes. If a potential endpoint occurs, a committee meeting will be convened to assess whether such events can be classified as a primary endpoint.
All AEs will be monitored from the time of randomisation until the last visit (day 30). The researchers will be responsible for assessing the severity of all AEs and their causal relationships with the study intervention. The start date, duration and treatment measures for each AE will be recorded.
During the assessor-blind period, we will evaluate compliance based on the dropout rate caused by AEs, where a lower dropout rate indicates higher compliance.
Baseline information will be collected during ward visits. This information includes age, sex, body mass index, educational level (in years), medical history, family history, medication review, diagnosis, physical examination, laboratory parameters, auxiliary examinations, NYHA classification, Charlson Comorbidity Index and ASA of Anesthesiologists classification.
During the baseline survey and the first seven follow-up visits (at least three visits) after randomisation, the following indicators will be recorded: medication review (including types and doses for medications, such as antibiotics, corticosteroids and immunosuppressants), physical examination, laboratory parameters, auxiliary examinations and pain management.
During the postoperative follow-ups at 1–7 and 30 days, postoperative complications, CCIs, treatment failures, dropouts and AEs will be evaluated. At the 30-day follow-up, ICU stay, hospital stay and total treatment cost will be recorded. A summary of the EDC system for data collection and management is presented in the Assessment section of online supplemental material 4. The investigators will receive EDC training before randomisation.
After each visit, all data will be recorded in the EDC system and then entered into SAS software (V. 9.4) by an independent data administrator. Participants’ identification information will be de-identified using the SAS database.
The Data Safety and Monitoring Board (DSMB) for this study consists of professionals and an independent statistician. The DSMB plans to hold meetings every 6 months to review the progress of the study, ensure compliance with ethical standards and ensure the safety of all enrolled patients. After each DSMB meeting, members will generate a report that includes all recommendations, which will be promptly submitted to the steering committee. To ensure that the collected data adhere to the protocol as stated, each centre in this study will undergo regular monitoring, and data consistency will be confirmed by comparing the data in the EDC system with the data in the source documents. An authorised representative of the sponsor will conduct regular online monitoring to review, audit and download copies of study-related documents. If necessary, the representative will meet with the investigators on-site to discuss any issues related to the study.
None.
This trial is in compliance with the principles of the Declaration of Helsinki and Good Clinical Practice. This trial has been approved by the Ethics Committee of Beijing Tsinghua Changgung Hospital (No. 23684-0-02) and its corresponding branch centres. Participants or their authorised surrogates will provide informed consent (online supplemental material 3) to participate in the study before it begins. Free medical services will be provided by the study sites to those who experience adverse effects resulting from trial participation. All modifications to the protocol will be submitted in consultation with the Institutional Review Board’s approval. Summaries of all relevant modifications will be disseminated to each centre and study investigator via email promptly.
Any identifiable information of the study participants will be de-identified, and the data will be archived using research identification numbers. All the data will be stored and managed by an independent investigator at a secure location. When data sharing is requested, the investigator will transfer the de-identified data files via an encrypted mobile storage device.
The primary trial results will be submitted for publication to a peer-reviewed journal. Findings will also be disseminated through abstracts, posters or presentations at local, national or international conferences. All investigators, including the project statistician, will have access to the final trial database after the publication of the study results. The data are not publicly available due to containing information that could compromise the privacy of research participants. The data that support the findings of this study will be available on request from the corresponding author. In addition, we will also establish a risk prediction model based on our findings, which will eventually be transformed into a risk-scoring system used for screening high-risk individuals with perioperative blood glucose disorders.
Blood glucose monitoring is essential for the effective management of diabetes. Currently, many monitoring methods are available, with the latest advances focusing on CGM technology. Numerous studies have shown that CGM can significantly improve blood glucose levels in patients with diabetes; however, most studies have been conducted on nonsurgical patients with diabetes.19 20 44–46
We conducted a retrospective analysis of 201 patients who underwent liver transplantation at Beijing Tsinghua Changgung Hospital between 2018 and 2020 and found that the incidence of SSIs in patients with diabetes was significantly higher than that in patients without DM (18.4% vs 8.9%, p<0.01). Patients with intraoperative blood glucose levels between 6.0 and 7.8 mmol/L manifested lower peak levels of CRP within the first 7 days after surgery (85.2±21.5 vs 127.7±23.3 µg/L, p<0.01) and a lower incidence of SSIs (75.68% vs 35.68%, p<0.01). We conducted a prospective randomised controlled study at Beijing Tsinghua Changgung Hospital from May 2021 to February 2023 based on the results of this retrospective analysis. This study included 164 patients who underwent elective orthotopic liver transplantation. Patients were randomly assigned to two groups: a strict blood glucose control group (6.0–7.8 mmol/L) and a liberal blood glucose control group (4.1–10 mmol/L). Glucose management during surgery was assisted by a real-time glucose monitoring system. Our study confirmed that using a real-time glucose monitoring system to assist in strict blood glucose control during surgery can reduce glycaemic variability, decrease the amplitude of blood glucose fluctuations and lower the incidence of early graft dysfunction and postoperative infections after liver transplantation. These findings are consistent with those of previous studies.25 26
Patients with DM are more prone to blood glucose dysregulation during the perioperative period owing to pre-existing abnormalities in glucose metabolism combined with stress-induced hyperglycaemia. Blood glucose dysregulation can lead to adverse outcomes, including increased complications, prolonged hospital stays and higher medical costs, significantly affecting surgical quality. Thus, objective assessment of postoperative complications is crucial for quality control during surgical procedures.47 48 The CCI is based on the CDC grading system and can be used to calculate cumulative postoperative complications (eg, at discharge or at 3 or 6 months after surgery), and its effectiveness has been duly recognised. The CCI has also shown a stronger correlation with the length of hospital stay.49 50 Therefore, it has become an internationally recognised measure for quantifying postoperative complications. Although a few studies have demonstrated that CGM aids blood glucose management and reduces postoperative complications in major surgeries, there is currently no large-scale real-world analysis available to establish its effectiveness in reducing CCI in patients with DM or IGT.
Continuous monitoring of key vital signs and goal-guided individualised precise control are gradually being incorporated into mainstream contemporary perioperative anaesthesia management. However, there is currently no management system in China that is based on continuous blood glucose monitoring for intraoperative blood glucose control. In this study, we proposed the adoption of a real-time, continuous and dynamic blood glucose monitoring system. This was combined with a goal-directed blood-glucose control process to form a semi-closed-loop precision dynamic control system. We will also use machine learning techniques to analyse and model intraoperative blood glucose changes to construct a risk-scoring system for high-risk individuals with blood glucose disorders. This is the first key technological innovation of this study.
Complete blood glucose management includes the prevention and control of hypoglycaemia, hyperglycaemia and high glycaemic variability. Currently, perioperative blood glucose management relies mainly on static blood glucose levels, which can only prevent the onset of hypoglycaemia and hyperglycaemia. However, proactive prevention of adverse postoperative reactions caused by increased glycaemic variability is lacking. In this study, real-time, continuous and dynamic glucose monitoring through CGM allows the incorporation of additional parameters related to glycaemic variability, which is beneficial for controlling glycaemic variability during the perioperative period and for optimising the current perioperative blood glucose management model. This is the second key technological innovation in our study.
Additionally, our previous study revealed that the intraoperative use of a real-time glucose monitoring system during liver transplantation surgery, in conjunction with strict blood glucose control, can significantly enhance patient outcomes. If the null hypothesis tested in this study proves to be true, that is, CGM reduces the overall postoperative infection rate, the occurrence of MACE and postoperative complication rate, it would greatly benefit a wider range of surgical patients beyond those undergoing liver transplantation surgery. Furthermore, it would provide stronger evidence-based clinical data to reduce postoperative complications in patients with DM or IGT. It would also contribute to promoting CGM as a technical standard and guideline for enhanced recovery after surgery in China and improve the long-term prognosis of individuals with DM or IGT. Such results provide significant direct social and indirect economic benefits.
This study has some limitations which should be considered. First, the researchers who implement the intervention measures and perioperative treatment, as well as the study participants, are not blinded, which may affect the clinical behaviour and treatment. Second, considering the risk of hypoperfusion affecting subcutaneous flow, the accuracy of CGM devices may be affected and may not fully reflect blood glucose levels. Therefore, many methods, such as fluid therapy and prophylactic vasoactive drugs, should be undertaken to alleviate the severity and duration of hypoperfusion. Further research specifically investigating the accuracy of CGM in the context of intraoperative hypoperfusion is warranted and represents a valuable direction for future studies. Third, even though the cost for patients is anticipated to be minimal, the requirement to pay for participation could still introduce bias, indirectly excluding those who are less fortunate. To alleviate the economic burden on these patients and ensure more equitable access to medical services, we can help these populations apply for financial assistance programmes.
The first patient inclusion occurred on 12 April 2024 at Beijing Tsinghua Changgung Hospital. The current protocol is V. 2.0, which was approved on 28 December 2023.
Consent obtained directly from patient(s).
We thank LetPub (www.letpub.com) for the linguistic assistance during the preparation of this manuscript.