What the hospital reform means for digitalization in hospitals | heise online
The hospital reform passed at the end of the year is intended to "de-economize" the hospital system and improve the quality of care. In the past, there has been repeated criticism of the previous financing system, according to which the treatment of patients must be as profitable as possible.
In the future, hospitals will have to meet certain criteria to be allowed to provide services in various service groups – such as maternity or heart surgery. This should lead to a specialization of hospitals, which should increase the quality of treatment.
At the same time, hospitals will have to close because they no longer meet the criteria for providing certain services.
The hospital reform has been heavily criticized because, among other things, it entails more bureaucracy. In the past, various expert reports have been commissioned which declare at least parts of the hospital reform to be unconstitutional. The German Hospital Federation (Deutsche Krankenhausgesellschaft, DKG) fears that the reform could lead to a "cold market shakeout", with many hospitals having to close.
Another challenge for hospitals is likely to be the expiry of funding for digitization, which is already subject to sanctions. "As part of the Hospital Future Fund (Krankenhauszkunftsfonds, KHZF), the BMG is funding around 6,000 projects with a volume of three billion euros (plus the federal states' share of thirty percent). The KHZF is part of the so-called German Recovery and Resilience Plan (Deutscher Aufbau- und Resilienzplan, DARP), meaning that the funding is refinanced via the EU's Recovery and Resilience Facility (RRF) and an extension of the fund is ruled out," said a spokesperson for the Federal Ministry of Health when asked about this. However, digitization should not end there.
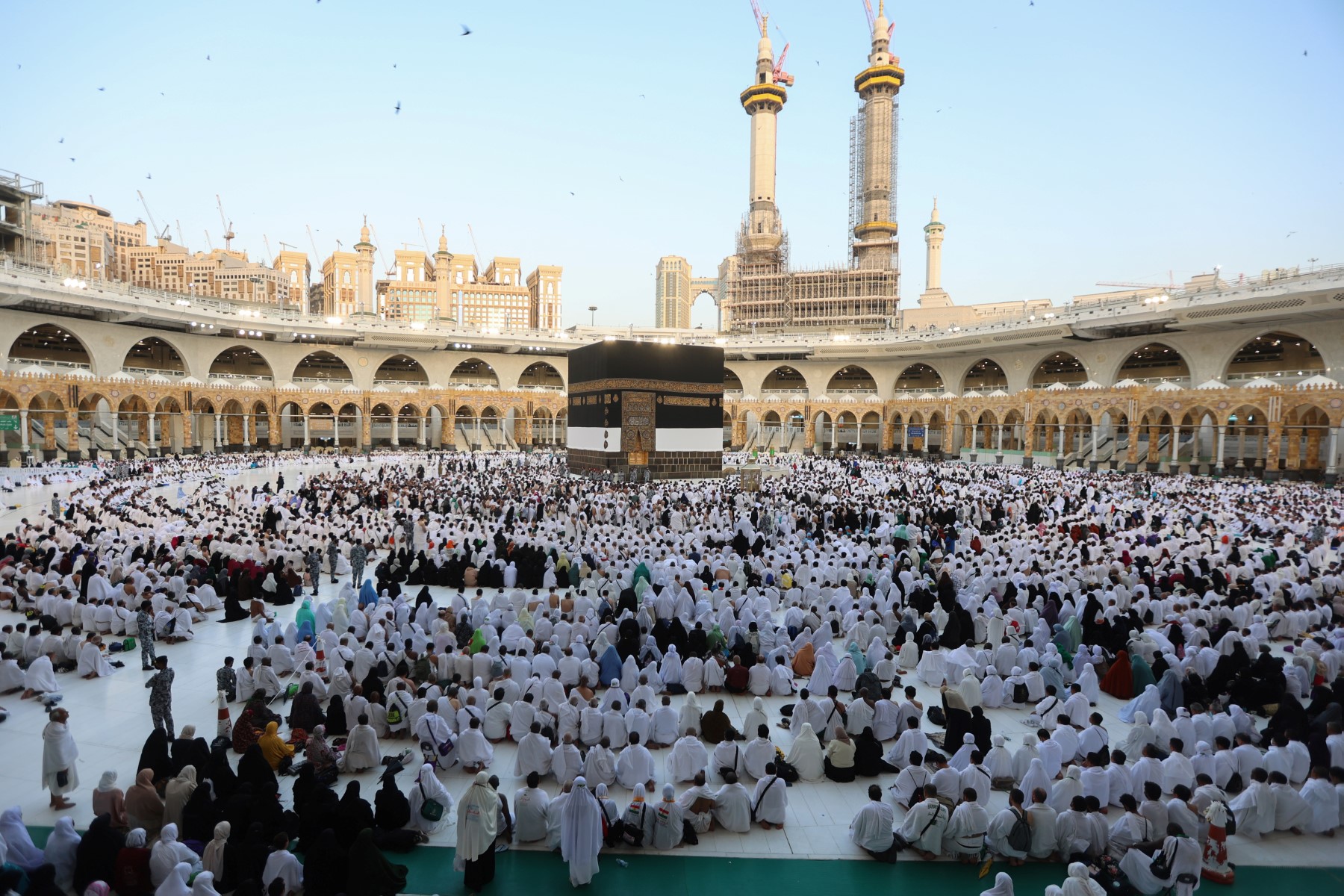
Computer scientist Markus Holzbrecher-Morys heads the "Digitalization and eHealth" division at the DKG.
(Image: DKG)
"Both the provision of a stable telematics infrastructure and the strengthening of binding standards and interoperability will further improve the framework conditions for digitization in the inpatient sector in the coming years," the BMG spokesperson continued. The transformation fund, which is to comprise 50 billion euros, is also an important building block. This is intended to provide funding to "harmonize information technology structures between hospital locations" or to ensure greater interoperability. "With the transformation fund, we are helping the federal states to invest in modern hospital structures," said Federal Health Minister Prof. Karl Lauterbach.
We spoke to Markus Holzbrecher-Morys about the Hospital Future Act and what the hospital reform means for digitalization. He is Head of Digitalization & eHealth at the DKG.
heise online: What will the hospital reform bring in terms of digitalization?
Holzbrecher-Morys: First and foremost, it brings significantly more bureaucracy, but overall it contains more individual regulations on digitalization. An overarching digitalization strategy –, which the BMG can certainly present –, was clearly not the focus of the legislative process. Above all, the reform ensures that hospitals have to provide even more data without any discernible benefit. During the development of the law, there was a failure to examine where digitization could really help and which existing information could be used to reduce bureaucracy.
This is particularly evident in the example of data transmission in accordance with Section 21 of the Hospital Remuneration Act. The InEK (Institut für das Entgeltsystem im Krankenhaus), the Institute for the Hospital Remuneration System, uses it to further develop the flat rate per case system every year.
So the DRG system?
Exactly that. The data deliveries that hospitals have to provide annually by March 31 are now just around the corner. Since the mid-2000s, the treatment data collected for the previous year has been transmitted to InEK in a specially structured form and evaluated there. InEK then uses this data to develop the DRG catalog for the following year. This is a very time-consuming, complicated process for everyone involved, but InEK has a great deal of experience with this and has been doing it for many years, which is stable.
The DRG system (Diagnosis Related Groups) is a flat-rate billing system that divides inpatient hospital treatments into groups with similar diagnoses and treatments. It is used for the performance-related remuneration of hospitals by calculating flat rates per case based on main diagnoses, secondary diagnoses, procedures, age, gender and other factors. The system was introduced in Germany in 2003 and is adjusted annually to ensure the medical and economic homogeneity of the case groups. Since his time in office, Health Minister Karl Lauterbach, who was jointly responsible for the introduction of the DRG system in 2003, has advocated a hybrid DRG system that is no longer profit-oriented. The hospital reform aims to bring about corresponding changes.
InEK also provides the data for the hospital atlas, right?
Exactly. Health Minister Karl Lauterbach had the idea of collecting even more hospital data for the hospital atlas. The task has been transferred to InEK.
Hospitals have to provide additional data to IneK every quarter. For example, information on medical and nursing staff is collected in a file for the hospital atlas. A hospital atlas that hardly covers any illnesses and that nobody needs because there are better databases. In another file, the staff at the locations must be assigned to the respective specialist departments. Even if this already causes enormous effort, it is at least still largely clear what is required. In a further file, the medical and clinical staff must then be assigned to the new service groups. The idea of hospital planning based on so-called service groups is at the heart of the hospital reform, but is a new instrument and is not yet established in practice – except in NRW. The allocation of medical staff to the new service groups poses considerable problems for hospitals.
Can you give an example of why this does not work?
The minute-by-minute allocation of medical staff to the service groups is not only bureaucratic madness, it also does not fit in with the case allocation system. If, for example, patients are assigned to a service group based on the length of stay in a specialist department, specialist departments with a systematically shorter length of stay typically fall through the cracks. For example, in gastroenterology or intensive care units. –.
Allow me to explain this using an example: An elderly person admitted to hospital dehydrated after a fall and with a fractured neck of femur is initially cared for briefly in an intensive care unit. This is followed by longer treatment in the geriatric ward, and the treatment case is assigned to the geriatric service group due to this longer treatment period. What informational value does it then have for the hospital atlas to assign the treating physicians from the intensive care unit to the geriatrics service group?
Hospitals must transmit this data to InEK every quarter –, i.e. also the allocation of the medical service to three decimal places. It must also be differentiated in which function the doctor worked if he has several specialist qualifications. Doctors can only estimate this at best. The bureaucratic effort is enormous and there are further challenges:
To be able to assign treatment cases to service groups at all, you need the service group group grouper – a software program that calculates the corresponding service group after the treatment information has been entered. Until now, hospitals have used the DRG grouper, which calculates a flat rate per case based on the ICD and OPS code – i.e. the disease and form of treatment – and other parameters.
Before the hospital reform, the primary function of the grouper was to group inpatient treatment cases into DRGs (Diagnosis Related Groups) in order to calculate hospital remuneration. This grouping was based on the ICD-10-GM diagnosis and operation and procedure codes (OPS) as well as other parameters such as length of stay. The grouper categorized the cases into DRGs, which in turn formed the basis for the flat rates per case that the hospitals received for their services.
In contrast to the new hospital reform, which introduces 65 service groups, the Grouper was not previously designed to promote hospital specialization or take into account quality criteria for specific service groups. Instead, the focus was on mapping treatment cases in DRGs to enable uniform remuneration.
In addition to the grouper software, there is now a new service group grouper. This also receives the treatment data and assigns the treatment case to a service group at the end – as in the example of geriatrics. The LG grouper is new software and is used in addition to the previous grouper. This software should be available to hospitals on September 30, 2024. However, due to the complexity of the process, the specification was not finalized until this year.
Did politicians set too tight a schedule?
Yes, and the manufacturers of the grouper software were generally only able to start implementation once the specification was available. This then went relatively quickly, but the rollout of this software in hospitals has only just begun.
Before software is used in a live environment in a hospital, it is usually tested in a test environment. This is where the hospitals check how the software behaves and whether there are any errors, which are then reported back to the manufacturer. The effort involved in software testing is considerable and continues to increase considering information security requirements. However, hospitals have to provide the data by March 31, even though the software is only partially available, let alone tested. We have contacted Mr. Lauterbach several times about this, but so far there has been no response.
The number and complexity of data reports has increased significantly in the context of the hospital reform. At the same time, hospitals that fail to provide the data must pay a fine of up to 50,000 euros per quarter. And that per location. These are the fines alone for not providing data for the hospital atlas.
This is perhaps a particularly clear example of the new bureaucracy and data transmission costs resulting from the hospital reform, where the costs and benefits are grossly disproportionate – if any benefit is recognizable at all. But the hospital reform also contains detailed bureaucratic regulations in other areas, for example in the planned form of reserve financing.
Why is this the case?
If anything, reserve financing increases the bureaucratic burden and does not provide sufficient security for hospitals. It also creates new disincentives and increases the risk of undersupply.
There are examples of how digital data transmission can improve care. The DEMIS interface, for example, has real advantages for hospitals. We can transmit reports on patients and on illness and vaccination data directly from the hospital information system to the Robert Koch Institute. Laboratory reports can also be transmitted automatically and since authentication also works via the telematics infrastructure, this is a real support –no longer having to send or sign anything by hand.
One problem for hospitals, however, is that the reporting software for addressing this DEMIS interface is not funded. Hospitals have to pay for this themselves, if they can, and these modules can be very expensive. The free version – the DEMIS reporting portal – is therefore the fallback solution for many hospitals. However, the complexity of data entry via the portal presents its challenges, for example when an error message appears at the end of a 12-minute entry marathon and the hospital has to start data entry all over again.
What could have been done better with the hospital reform?
There is a lot of room for improvement, but I'll limit myself to the digital aspect for now: even during the pandemic, we urged hospitals to first check what the routine data from the various data transmission processes already provided. The daily "bed notification" could have been derived – with a certain degree of imprecision – from the daily generated and automatically transmitted billing data, in compliance with data protection regulations. Without distracting nursing staff in particular from their actual work by recording this data. We already collect so much data in the standard procedures. In the interests of data economy and reducing bureaucracy, we should always first consider what data is already available before setting up a new data transmission procedure for every query.
This is a fundamental problem with current digitization efforts in the healthcare sector: Instead of efficient processes and support in their core activities, we are seeing more and more bureaucracy due to more and more data being demanded. This leads to a lot of frustration for everyone involved.
What has the Hospital Future Act (KHZG) achieved so far?
The KHZG has given hospitals a massive boost towards digitalization. However, the market was not prepared for the KHZG at the time. The industry did not have the capacity to handle all digitization projects in 1,700 hospitals at the same time. And some hospitals were also caught cold by the "windfall".
We now know from many conversations that hospitals that had to submit their applications to the respective federal state without a completed digitalization strategy often applied for funding. This was either not sustainable in the long term or should have been postponed in favour of other projects. The total of 4.3 billion euros – 3 billion euros of this from the EU – was an important boost for digitization in hospitals. This can be seen on the one hand in the results of the "Digital Radar", a nationwide survey of the current digital status of hospitals, but also in the increasingly specific questions on digitization from hospitals. While hospitals scored an average of 33 points out of 100 in the Digital Radar 2021, this figure had risen to more than 40 points by 2024.
The digitization of patient files, the paperless hospital, was a utopia back then. Today, many hospitals are saying: "Yes, we're on the right track" or "We've already implemented this in many areas", for example digital treatment documentation. Many things have progressed here and I am very glad that the KHZG has been introduced. There is no question that mistakes were made along the way. Nevertheless, the KHZG was enormously important.
You said earlier that there is no funding for the DEMIS interface. What is the situation regarding the financing of the software acquired to date within the framework of the KHZG?
This is actually the biggest concern for us at the moment. We could fall behind again with the next digital radar query, or the one after that at the latest, because the operating costs for digitalization in hospitals are not being financed anywhere today. At the same time, the framework conditions have changed considerably. Everyone is familiar with this: you used to buy software. At some point, you bought the new version, usually with a discount for the upgrade. Nowadays, the market is predominantly focused on software-as-a-service –, i.e. "subscription" models. This is no different in hospitals. The ongoing operating costs for subscription licenses are much higher than the one-off purchase of software, something that has not yet been taken into account anywhere. Let's say 10 million was invested, then the operating costs usually amount to 2.5 to 3 million – sometimes even annually. This is not refinanced and the hospitals have no reserves to pay for it.
We fear that – as soon as the KHZG funding expires at the end of 2025 – many hospitals will have to shut down the digitization projects they have already set up overnight because they simply cannot pay their bills. This prospect – that the plug will be pulled on the digitization projects that have been painstakingly set up – is currently the great sword of Damocles for our efforts to increase digitization in hospitals.
Will there be savings with digitization, as calculated by consulting firms?
In my opinion, it is simply nonsense to assume that we are already saving money with digitalization. From an overall economic perspective, the efficiency gains associated with digitalization will certainly result in savings. For the individual hospital, however, it will be more expensive at the moment. We need to become more efficient and must not stumble over digitalization.
However, it must also be acknowledged that in the transition to the use of new digital processes, the previous, often analog systems will still have to be used, at least in part. Or appropriate replacement systems will have to be kept available in the long term. This means that there will be no cost savings, at least in the short term. In addition, we are currently still experiencing a great deal of frustration with the development of new processes, such as the telematics infrastructure. Costs are not the only success factor for digitalization – Acceptance by users –, both patients and, for example, medical and nursing staff, is at least as important.
A lot has happened in terms of digitalization with the KHZG, but it is currently primarily costing hospitals money and threatens to be slowed down again soon – The lack of operating cost financing is an enormous problem. There are, of course, ideas about the transformation fund and the planned special fund, but these ideas are still completely unfinished. And even if we support the idea of the transformation fund in principle, we do not think it is right to pay half of it from the contributions of those with statutory health insurance.
What is the point of the additional costs involved in geocoding hospital outpatient departments? The existing information in the location directory is already very detailed.
The location directory in accordance with Section 293 (6) SGB V is a nationwide database that records the locations of hospitals licensed in accordance with Section 108 SGB V and their outpatient clinics. It is maintained by InEK on behalf of the German Hospital Federation (DKG) and the National Association of Statutory Health Insurance Funds (GKV-Spitzenverband).
The directory has been in regular operation since January 1, 2020 and can be viewed online via the krankenhausstandorte.de website. Hospitals can register there, record their locations and apply for the corresponding identifiers. The contents of the directory are publicly accessible if you register as a user. The data of all hospitals can be viewed online and downloaded in XML format.
The location directory is used, among other things, for billing services, quality assurance and data transfer to the data office in accordance with Section 21 (1) KHEntgG. It contains information such as the geodata of the hospital operators, location codes, institution codes and addresses of the hospitals and outpatient clinics.
The directory of hospital locations in Germany has existed since 2017 and has now become established in many areas. The regulations of Section 2a of the Hospital Financing Act are decisive for this, which stipulates, for example, that buildings at a hospital site may not be more than 2,000 meters apart. Accordingly, the site must be divided into two locations – including the duplication of all reporting obligations. This site directory – a publicly available XML file – also lists the hospitals' outpatient clinics. The legislator has now demanded that the geocoordinates of each individual outpatient clinic be entered in the directory. Irrespective of the fact that many hospitals had already recorded this information in previous years –, this does not result in any real added value, for example for patients.
What is the benefit of entering a geocoordinate in the directory?
For patients, the geocoordinate is completely irrelevant. People don't come to the hospital with a GPS tracker and enter the coordinates of an outpatient clinic from an XML file on the Internet. They usually go to the main entrance and either look at the signpost or ask for directions at the central information desk.
Whether the information in the directory is relevant for the health insurance companies, which carry out plausibility checks based on the directory as part of the billing check, can at least be assumed. If it is then necessary to negotiate which geo-coordinate is to be specified for a telemedicine outpatient clinic as part of the self-administration's specifications, the bureaucracy becomes clear once again.
You mentioned the topic of telemedicine earlier. What is the situation here?
Fortunately, there are fewer and fewer technical hurdles when it comes to telemedicine. The recently published report by the Bundestag Committee on Education, Research and Technology Assessment on telemedicine (printed matter 20/15069) sees telemedicine on the right track here. Appropriate remuneration is important. If there is no refinancing for these topics, they simply cannot be offered. And that is a shame because there are still many opportunities to improve care in this area in particular and to respond to the challenges of our time with the possibilities of digital innovation.
(mack)