Archives of Public Health volume 83, Article number: 169 (2025) Cite this article
Stroke is the leading cause of mortality in Indonesia, with hypertension and diabetes mellitus (DM) recognized as well-established risk factors. Moreover, recent epidemiological studies have documented rising incidence, morbidity and mortality of these conditions. Understanding their spatial distribution and interrelationships is crucial for developing targeted public health interventions. This study aims to analyze the geographic distribution of stroke, DM, and hypertension across Indonesia’s provinces, evaluate their spatial correlations, and explore their interconnections using advanced spatial modeling techniques.
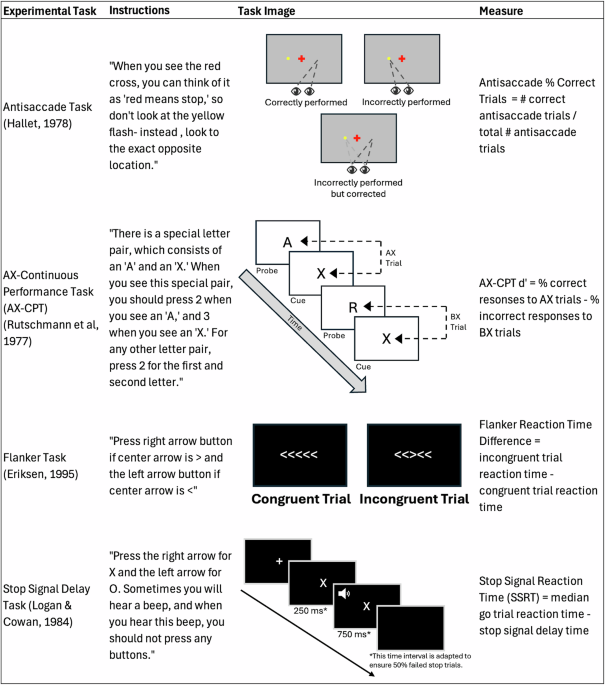
The data were collected from the Social Health Insurance Administration Body, which manages Indonesia’s universal health coverage, between 2017 and 2022. Crude incidence rates for the diseases were calculated and spatial distribution patterns were analyzed using Global and local Moran analysis. A spatial autoregressive (SAR) model was employed to assess the spatial dependence and interrelationships between these diseases.
The crude incidence rates of stroke, hypertension, and DM were 158.47, 2716.34, and 1503.06 per 100,000 population, respectively. Significant spatial heterogeneity was observed, with certain provinces consistently appearing as high-risk areas across all three diseases. Through SAR analysis, our study identified a significant positive spatial association between DM and stroke incidence, indicating that provinces with higher DM rates also tend to experience elevated stroke burden.
This study mapped the geographical and spatial distribution of stroke, DM, and hypertension across Indonesia and found the pivotal role of DM in driving stroke incidence. By prioritizing high-incidence regions and addressing specific risk factors, targeted interventions can significantly reduce stroke cases and enhance public health outcomes in Indonesia.
Text box 1. Contributions to the literature |
|---|
• Stroke is the number one cause of death in Indonesia, and to date, no geospatial map of this disease has been developed. This study fills that gap by providing the first comprehensive geospatial analysis of stroke, diabetes mellitus (DM), and hypertension across all 34 provinces. |
• By utilizing advanced spatial modelling techniques, this study found the significant role of DM in determining stroke incidence. |
• The identification of high-risk geographic clusters, along with the recognition of DM as a critical determinant of stroke incidence, offers valuable insights for shaping public health policy and guiding targeted interventions to reduce stroke incidence in Indonesia. |
Non-communicable diseases (NCDs) represent a critical health challenge on both national and global scales. Among these, stroke is a leading cause of mortality and disability in Indonesia, with its prevalence and mortality rates demonstrating a consistent upward trend over recent years [1]. In the South East Asia, Indonesia ranks second in stroke incidence and prevalence, reporting 642,943 new cases and 4,918,487 individuals living with stroke, surpassed only by India, which records 1,291,245 new cases and 9,650,716 prevalent cases. Bangladesh follows in third place with 182,856 new cases and 1,417,979 individuals affected [2]. Furthermore, Indonesia exhibits one of the highest age-standardized stroke mortality rates in this region, estimated at 19.3 per 1,000,000 population, significantly exceeding rates in neighbouring countries such as the Philippines (10.96), Malaysia (8.43), and Singapore (4.79) [3, 4]. In addition, the data released by the Social Health Insurance Administration Body (BPJS) in 2016 exhibited that stroke costs for service fee was almost $1 million [5]. Apart from this medical expenses, non-health costs which related to the consumption of non-healthcare resources such as transportation, household expenses, relocation, and productivity loss were also severe, which accounted for more than half of the medical costs [5, 6].
Diabetes mellitus (DM) and hypertension are identified as the top two major risk factors for stroke, contributing significantly to its global burden [7, 8]. In Indonesia, approximately 10% and 30% of the population suffer from DM and hypertension, respectively, with these figures expected to rise in the coming years [9, 10]. These two diseases also been reported as the top 10 cause of death in Indonesia [11]. Hypertension increases stroke risk by exerting constant high pressure on arterial walls, leading to their weakening and potential rupture [12]. Similarly, DM contributes to stroke risk by accelerating the development of atherosclerosis and increasing the likelihood of clot formation due to poor blood glucose control [13]. The interplay between DM and hypertension might further compounds the risk, as individuals often suffer from both conditions simultaneously, leading to a synergistic effect that greatly amplifies their cerebrovascular risk [14]. However, the interplay between these risk factors and their spatial distribution in a geographically diverse country like Indonesia remains underexplored.
Understanding the spatial patterns is crucial, as it can reveal regions where public health interventions may be most needed and effective [15]. Furthermore, spatial analysis can provide insights into the environmental and socio-economic factors that contribute to the clustering of these diseases [16, 17], thereby offering a more comprehensive understanding of the epidemiology of NCDs in Indonesia.
This study aims to fill this gap by conducting a detailed spatial analysis of stroke, DM, and hypertension across Indonesian provinces. Using spatial autocorrelation techniques, we assess the clustering of these diseases and identify specific regions where the incidence is significantly higher or lower than expected. We further employ a spatial autoregressive model to examine the strength and direction of the relationships between DM, hypertension, and stroke, with a particular focus on understanding how these conditions interact spatially.
By integrating spatial analysis with traditional epidemiological approaches, this study seeks to provide a deeper understanding of the geographic distribution and spatial interplay between stroke, DM, and hypertension in Indonesian provinces. The findings are intended to guide public health strategies aimed at reducing the burden of these diseases, ultimately contributing to improved health outcomes and reduced health disparities across the country.
The data used in this study refer to health insurance participants who diagnosed with stroke, DM, and hypertension from 2017 to 2022, across all 34 provinces in Indonesia. In this research, each province represents a spatial unit of analysis. The dataset was obtained from the Social Health Insurance Administration Body (BPJS Kesehatan), a government organization responsible for administering Indonesia’s universal health coverage system, which encompasses approximately 95% of the population. The data submitted through the BPJS health system originates from hospitals and clinics and undergoes a tiered verification process. Initially, the data is verified by auditors within each hospital or clinic to ensure accuracy and compliance with established standards. Subsequently, the data is further audited by verifiers at the BPJS branch offices in each city or district. This multi-level verification process ensures the reliability and trustworthiness of the data. To comprehensively capture the incidence of these diseases, we included all new reported cases, irrespective of follow-up status, including those lost due to death, withdrawal, or other reasons during the study period. Population data were sourced from the Central Bureau of Statistics (Badan Pusat Statistik, BPS), a non-departmental government agency in Indonesia tasked with conducting statistical surveys.
The daily data on stroke, DM, and hypertension used in this study were processed to determine the crude incidence rates of these diseases as reported by BPJS Kesehatan. Crude incidence rates were calculated per 100,000 individuals for each year, considering the annual population figures reported by BPS to ensure the rates were adjusted for yearly variations in population size. The crude incidence rate was calculated using the following formula:
$$\begin{array}{l}\:{\rm{Crude}}\,{\rm{incidence}}\,{\rm{rate}}\,\left( i \right)\,{\rm{ = }}\\\frac{{The\:number\:of\:new\:disease\:at\:province - i}}{{The\:number\:of\:population\:at\:province - i}}\:x\:100.000\end{array}$$
Additionally, we also computed the minimum, maximum, mean, and standard deviation of the crude incidence rates for each disease to provide a comprehensive statistical overview (Supplementary Table 1).
The map [18] was generated by using R Basic version: 4.2.2 (https://cran.r-project.org/bin/windows/base/) and R Studio Desktop version: 2022.07.2 + 576 (https://posit.co/download/rstudio-desktop/) for windows operating system. We also used some packages to generate the figure such as sf package (https://r-spatial.github.io/sf/) [19], dplyr package (https://github.com/tidyverse/dplyr) [20], rgdal package (http://rgdal.r-forge.r-project.org/), tmap package (https://github.com/r-tmap/tmap) [21] and leaflet package (https://rstudio.github.io/leaflet/) [22].
The natural break method is a quantitative technique used to identify clusters of values within a dataset that are distinct from each other. This method employs a Jenk algorithm designed to minimize variance within groups while maximizing variance between them [23]. The results of the natural break algorithm are often visualized in a map using a gradient of colors.
Correlation network analysis was determined using the Gaussian Graphical Models (GGM) method. Partial correlations are estimated as the correlation between two variables after adjusting for the linear influence of one or more other variables. In this regard, correlation tests refer to statistical methods designed to measure the relationships between variables within the GGM framework. Specifically, robust correlation estimators were employed to ensure resilience against outliers or extreme data points, which can significantly affect conventional methods such as Pearson correlation. These estimators are particularly advantageous when analyzing data with unusual distribution patterns, as they provide a more reliable measure of association [24]. Correlation tests were then conducted after partitioning the dataset, separately from the original dataset. In other words, this approach considers partitioning as an independent step that produces a different dataset, rather than deriving from the same model. Conceptually, GGM encompasses a set of variables depicted as circles (“nodes”) and a series of lines visualizing the relationships between these variables as edges, with the thickness representing the strength of the association [25]. GGM estimates a large number of parameters, which likely results in several edges or associations. Therefore, GGM is typically regularized through graphical lasso [26]. The correlation image [27] was generated by using R Basic version: 4.2.2 (https://cran.r-project.org/bin/windows/base/) and R Studio Desktop version: 2023.12.1 + 402 (https://posit.co/download/rstudio-desktop/) for windows operating system. We also utilized several packages to produce this figure such as igraph package (https://github.com/igraph/rigraph/) [28] and ggraph package (https://github.com/sbma/qgraph/) [29].
The Spatial autoregressive model (SAR), also known as the spatial lag model (SLM), is a spatial modeling approach that considers the spatial lag effect on the dependent variable only. This model is also referred to as a Mixed Regressive-Autoregressive model because it combines a standard regression model with a spatial lag regression model for the dependent variable [30].
The analysis process begins with data exploration to gain an initial understanding of the response variable’s spatial characteristics using thematic maps with Natural Breaks. Next, a spatial weight matrix is determined to identify the proximity between regions. The spatial weight matrix used is the inverse distance weight.
To identify spatial autocorrelation effects, Global Moran’s I is applied to both the response and predictor variables. Further, to detect specific units of observation, Local Moran and Getis-Ord Gi* Statistics are utilized. Both Local Moran and Getis-Ord Gi* measure local spatial association, although with slightly different applications. Local Moran is used to describe the relationship between individual observations and their neighbors, identifying spatial clusters (high-high, low-low) and spatial outliers (high-low, low-high). Meanwhile, Getis-Ord Gi* specifically identifies clusters, highlighting areas of high-high (hot spots) and low-low values (cold spots). The computation of Getis-Ord Gi* yields a Gi* statistic for each observation and assesses statistical significance with a 95% confidence level.
The model then assesses spatial heterogeneity effects using the Breusch-Pagan test and evaluates data distribution across observations with the Shapiro-Wilk test. The parameters of the Spatial Autoregressive model are determined using the Maximum Likelihood method using the following formula:
$$\:y = \rho \:Wy + X\beta \: + + \epsilon $$
The model is then tested for the significance of parameters both simultaneously and partially. Finally, the model is interpreted by explaining the impact of each variable based on marginal effects. Marginal effects are divided into direct and indirect effects, with the total effect being the sum of both direct and indirect effects.
We utilized the following package for SAR analysis: sf: https://github.com/r-spatial/sf [19], tidyverse: https://github.com/tidyverse/tidyverse [31], spatialreg: https://github.com/cran/spatialreg [32], readxl: https://github.com/tidyverse/readxl [33], spdep: https://github.com/r-spatial/spdep [34], tigris: https://github.com/USCensusBureau/tigris [35], nortest: https://github.com/cran/nortest [36].
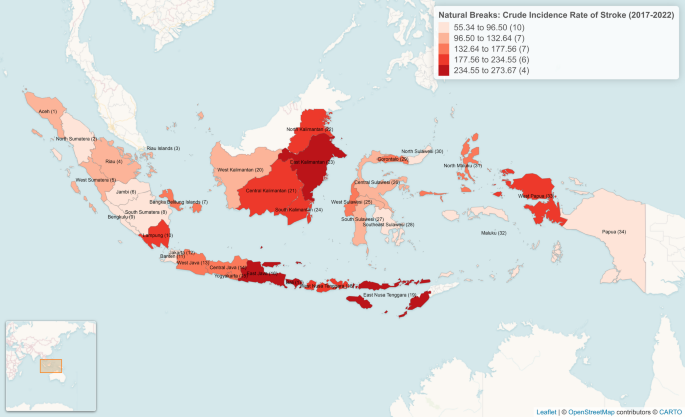
Data from BPJS for the study period indicated the incidence rates of 158.47, 2716.34, and 1503.06 per 100,000 population for stroke, hypertension, and DM, respectively, across Indonesia (Table 1). Spatial analysis revealed significant heterogeneity in the distribution of these conditions. Provinces subsequently are stratified into five clusters based on the incidence of stroke, DM, and hypertension, with Cluster 1 representing the lowest incidence and Cluster 5 the highest. For stroke, Banten, Bengkulu, Jakarta, Jambi, Maluku, Papua, Southeast Sulawesi, North Sulawesi, South Sumatera, and North Sumatera are the provinces classified in Cluster 1, indicating a relatively low burden of cerebrovascular events in these areas (Fig. 1). In contrast, Bali, East Java, East Kalimantan, and East Nusa Tenggara fall into Cluster 5, pointing to a significantly higher stroke incidence (Supplementary Table 2).
Stroke incidence across Indonesia from 2017–2022. Aceh (1), North Sumatera (2), Riau Islands (3), Riau (4), West Sumatera (5), Jambi (6), Bangka Belitung Islands (7), South, Sumatera (8). Bengkulu (9), Lampung (10), Banten (11), Jakarta (12), West Java (13), Central Java (14), Yogyakarta (15), East Java (16), Bali (17), West Nusa Tenggara (18), East Nusa, Tenggara (19), West Kalimantan (20), Central Kalimantan (21), North Kalimantan (22), East Kalimantan (23), South Kalimantan (24), West Sulawesi (25), Central Sulawesi (26), South Sulawesi (27), Southeast Sulawesi (28), Gorontalo (29), North Sulawesi (30), North Maluku (31), Maluku (32), West Papua (33), Papua (34)
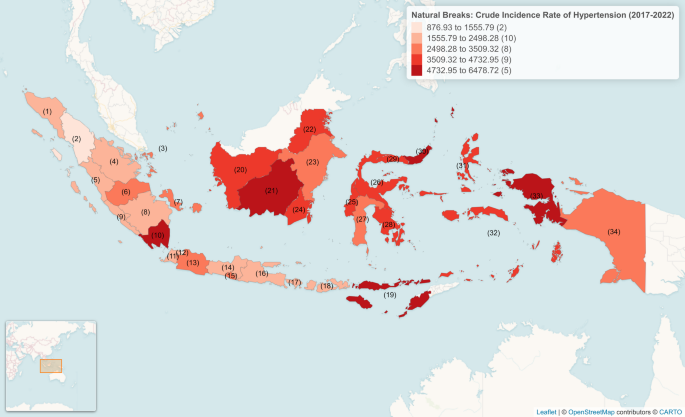
Hypertension data similarly reveal a broad range of incidence, with provinces such as Jakarta and North Sumatera being in Cluster 1, which has the lowest hypertension rates (Fig. 2). On the other hand, Central Kalimantan, East Nusa Tenggara, West Papua, and North Sulawesi, appears in Cluster 5, marking these provinces as high-incidence areas for hypertension (Supplementary Table 3).
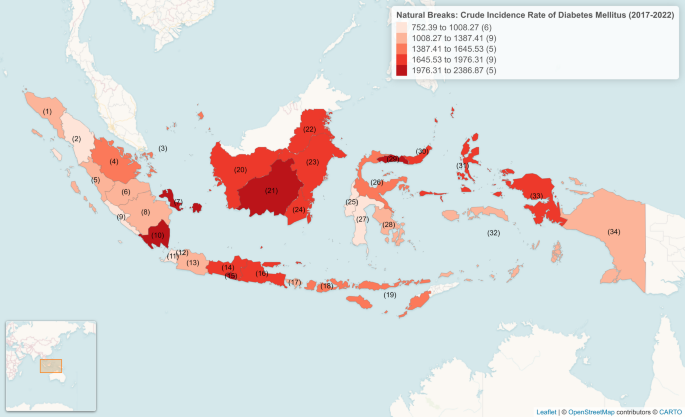
When examining DM incidence, the clustering reveals another dimension of the NCD landscape in Indonesia. Banten, Bengkulu, Jakarta, West Sulawesi, South Sulawesi, and North Sumatera are in Cluster 1 (Fig. 3). In contrast, Yogyakarta, Gorontalo, Central Kalimantan, Bangka Belitung Islands, and Lampung are found in Cluster 5, highlighting regions with a high burden of DM (Supplementary Table 4). Notably, Central Kalimantan’s consistent presence in the high cluster across all three diseases underscores its status as a critical area in need of targeted interventions.
Analysis of age-standardized incidence and stratifications by gender revealed significant temporal trends and demographic disparities in stroke, hypertension, and DM from 2017 to 2022 (Supplementary Fig. 1). For stroke, males consistently exhibited higher incidence rates than females, particularly in the 40–65 years age group, where incidence peaked in 2020 (604.95 per 100,000 population) before experiencing a sharp decline in 2021 (0.66 per 100,000 population). A similar drop was observed across all age groups in 2021, likely due to disruptions in healthcare access and reporting during the COVID-19 pandemic [37]. Among individuals aged > 65 years, stroke incidence was highest in 2020 (279.06 per 100,000 population) but declined in subsequent years.
Hypertension and DM demonstrated higher incidence rates in females across most years and age groups. In the 40–65 years group, hypertension incidence increased in 2020 (10,046.23 per 100,000 for females; 6243.52 for males) before declining sharply in 2021 (20.35 per 100,000 for females; 8.1 for males). A similar pattern was observed for DM, with the highest incidence in 2020 (5,805.58 per 100,000 for females; 4,070.9 for males), followed by a marked decline in 2021. The < 40 years age group exhibited the lowest incidence rates for all conditions, with relatively stable trends except for a slight decrease in 2021.
The high incidence of stroke, hypertension, and DM in the 40–65 age group, often regarded as the productive age, is particularly concerning. This age group is a vital segment of the workforce, and the high disease burden could lead to significant economic and societal impacts, including reduced productivity, increased healthcare costs, and premature morbidity or mortality. These findings underscore the urgent need for targeted preventive measures and healthcare interventions aimed at this demographic to mitigate long-term consequences.
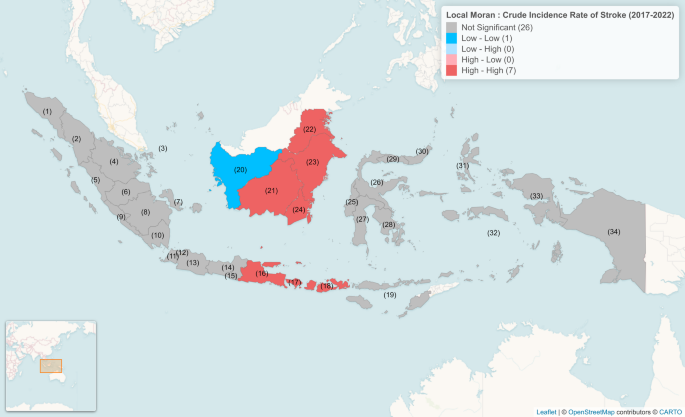
To assess the spatial distribution patterns of stroke, DM, and hypertension across Indonesian provinces, a spatial autocorrelation analysis using Global Moran’s I was conducted. The analysis revealed significant spatial autocorrelation for all of these diseases (Table 2), indicating that these diseases exhibit clustering, where provinces with high or low incidence are geographically close to other provinces with similar incidence rates. We subsequently performed local Moran analysis to identify the specific geographical location of diseases incidence with similar rates. We categorized the local Moran distribution into 4 categories (Supplementary Table 5) including low-low, also called as coldspot (a cluster of low incidence surrounded by low incidence), low-high (a low-incidence area surrounded by high incidence), high-low (a high- incidence area surrounded by low incidence), and high-high, also called hotspot (a cluster of high incidence surrounded by high incidence).
For stroke incidence, the analysis identified West Kalimantan as coldspots (Fig. 4). Conversely, hotspots were found in Bali, East Java, South Kalimantan, Central Kalimantan, East Kalimantan, North Kalimantan, and West Nusa Tenggara (Supplementary Table 5). Notably, apart from East Java, no other areas on Java Island were identified as hotspots or coldspots, suggesting that stroke incidence across the rest of the island is relatively uniform.
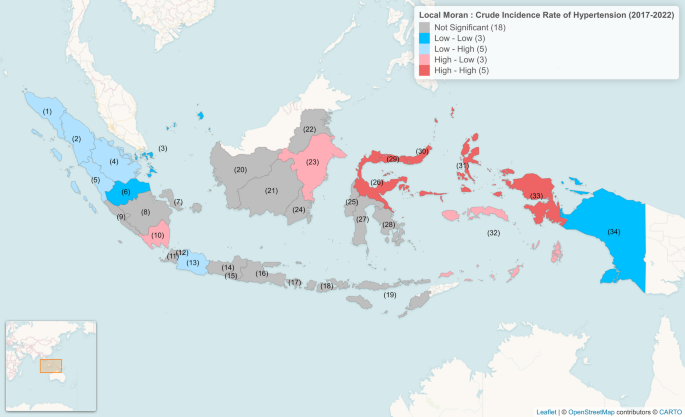
Hypertension incidence shows a slightly different spatial pattern, with Jambi, Riau Islands, and Papua identified as coldspot (Fig. 5). However, the hotspot, identified in Gorontalo, North Maluku, West Papua, Central Sulawesi, and North Sulawesi, highlight regions where hypertension incidence is notably higher, surrounded by similarly high-incidence areas.
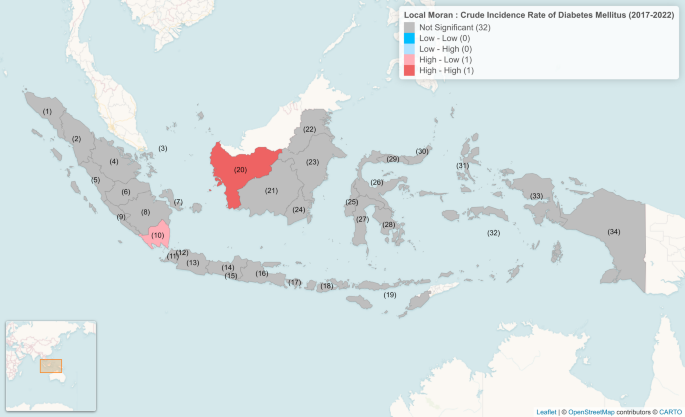
In terms of DM incidence, no coldspots were identified, while Lampung was the only area classified as hotspot (Fig. 6). The current study highlights that the clustering of hotspots for DM and hypertension outside of Java island, particularly in eastern Indonesia, suggests regional challenges in managing these diseases, which may be related to factors such as healthcare access, socioeconomic conditions, or genetic predispositions [38, 39].
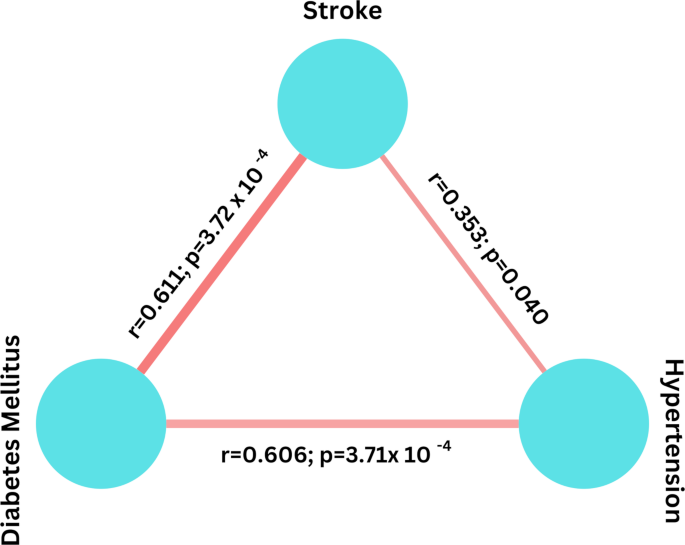
Experimental, clinical, and epidemiological evidence has consistently implicated both DM and hypertension as primary risk factors for stroke [40]. Our network correlation analysis using Gaussian graphical model further supports this association, revealing significant correlations between both diseases and stroke (Fig. 7). It is noted also here that the correlation between DM and stroke was found to be more pronounced than that between hypertension and stroke in this archipelago nation, as observed by the lower p and higher r value.
The Gaussian model of stroke, hypertension, and DM incidence across Indonesia revealed a strong correlation between both DM and hypertension with cerebrovascular diseases
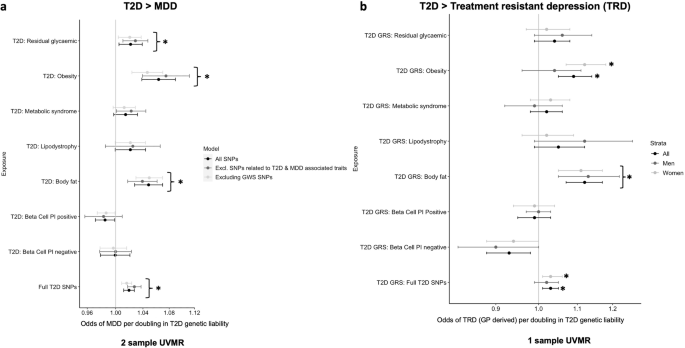
To capture the strength and direction of the spatial dependence of stroke, hypertension, and DM, and considering the significant global Moran’s p value, we employed a spatial autoregressive model. Prior to conducting this analysis, we performed normality and Breusch-Pagan tests to ensure the validity, efficiency, and reliability of the model’s results, which showed a significant value for both test (Supplementary Table 6). Our spatial analysis then revealed a significant positive association between DM and stroke incidence in Indonesia, suggesting that areas with high DM rates also tend to have high stroke rates (Table 3). Interestingly, the model did not show a statistically significant spatial relationship between hypertension and stroke incidence. The discrepancy between the Gaussian model and SAR model results might be attributed by the ability of SAR model to capture spatial dependencies and identify localized patterns, which are often overlooked by the global correlations assessed in Gaussian models.
The marginal effect subsequently confirmed the SAR model as observed by an increase of one unit in the incidence of DM in the same region raises the incidence of stroke across all regions by an average of 0.079 units (Table 4). This finding indicates that an increase of 100 people with DM could lead to an increase of 7.9 people with stroke in the same province. Conversely, an increase of one unit in the incidence of DM in different regions increases the incidence of stroke by an average of 0.104 units, meaning 100 additional DM cases could result in 10.4 more stroke cases in different provinces. If the incidence of DM increases across all regions, the incidence of stroke will rise by an average of 0.183 units, or 18.3 additional stroke cases per 100 DM cases throughout Indonesia. In short, our data showed that the incidence of DM significantly contributes to an increase in stroke cases across Indonesia.
This study analyzed the incidence and spatial distribution of stroke, hypertension, and DM across Indonesian provinces using BPJS data. These diseases demonstrated significant regional variability, with certain provinces, such as Central Kalimantan, consistently exhibiting high incidence across all three conditions. Spatial autocorrelation analysis revealed clusters of high and low incidence areas, with most located in provinces outside Java Island. The spatial autoregressive model confirmed a significant positive association between DM and stroke incidence, suggesting that regions with higher DM rates also experience higher stroke rates. This finding underscores the critical importance of addressing DM as part of targeted interventions to reduce stroke incidence.
The integration of spatial analysis in epidemiological studies is pivotal for tackling disease burden and enhancing healthcare systems. By uncovering geographic patterns and clusters of disease incidence, spatial studies enable the identification of high-risk areas and localized disparities in health outcomes [41]. This approach provides actionable insights for policymakers to design targeted interventions, allocate resources efficiently, and implement region-specific health programs. Furthermore, spatial studies offer a deeper understanding of the interplay between geographic, demographic, and health system variables, facilitating a comprehensive assessment of healthcare accessibility and equity [15]. In the context of this study, the geospatial identification of stroke, DM, and hypertension hotspots underscores the need for tailored public health strategies to address regional disparities and optimize the delivery of health services in Indonesia.
Building on the significance of geospatial analysis, it is also crucial to position Indonesia’s stroke burden within a broader regional and global framework to contextualize its public health impact. The South East Asia region, comprising only 11 countries, accounts for over 40% of global stroke mortality, a striking statistic that underscores the region’s disproportionate stroke burden [2]. Within this context, Indonesia ranks second in both stroke incidence and prevalence. Notably, Indonesia also has the highest age-standardized stroke mortality rate in the region and ranks second in morbidity [2, 4]. Unlike countries such as India and Thailand, which have a National Stroke Registry Program and a database for stroke epidemiology, Indonesia lacks a national stroke surveillance system [42]. This limitation not only challenges efforts to accurately quantify the stroke burden but also highlights the critical role spatial studies play in bridging these data gaps. By mapping disease incidence and clustering patterns, spatial studies can complement the absence of systematic stroke surveillance, facilitating better resource allocation and targeted interventions. Moreover, inadequate healthcare infrastructure and limited public awareness exacerbate delays in treatment in Indonesia compared to other countries in the region [43].
The spatial analysis of stroke, DM, and hypertension incidence across Indonesian provinces highlights significant clustering patterns, reflecting the complex interplay of socioeconomic, environmental, and regional characteristics [44]. The identification of coldspots, such as that observed in West Kalimantan for stroke, suggests the presence of protective factors, including potentially higher hospital utilization number and healthier regional practices, that contribute to lower incidence rates [45, 46]. In contrast, hotspots for these diseases are predominantly located outside Java, underscoring the pronounced regional disparities in healthcare access and socioeconomic conditions.
Java, as the economic and administrative center of Indonesia, enjoys superior infrastructure, education, and healthcare access compared to other regions [47,48,49]. This concentration of resources likely contributes to the relatively uniform distribution of NCDs on the island, as evidenced by the absence of significant spatial clustering. Java’s well-established healthcare infrastructure, higher density of healthcare professionals, and robust public health programs facilitate more effective prevention, diagnosis, and management of diseases like stroke, DM, and hypertension [50]. Additionally, higher educational attainment on Java fosters better health literacy, enabling individuals to adopt healthier lifestyles and seek timely medical care [51, 52].
In contrast, hotspots in provinces outside Java, particularly in Eastern Indonesia, reflect systemic challenges such as inadequate healthcare infrastructure, limited access to specialized services, and lower socioeconomic development [45, 53]. These disparities hinder disease prevention and management efforts, compounding the burden of NCDs [54]. Moreover, it is plausible that genomic factors may contribute to the observed clustering of stroke, DM, and hypertension in eastern Indonesia [55]. Certain indigenous populations in these regions could harbor unique genetic predispositions that influence their susceptibility to these NCDs [56,57,58]. However, direct evidence supporting this hypothesis remains limited, as genomic studies in these populations are scarce [59]. Future research integrating genomic and environmental data is essential to unravel the potential role of genetic factors in shaping disease prevalence in these areas.
In addition to this, while observing the distribution of hotspots predominantly in rural provinces outside Java, we also noted some coldspots in these same regions, such as Jambi and Riau Islands for hypertension. Additionally, Bali, an urbanized region, and East Java (the only province in Java classified as a hotspot) emerged as a hotspot for stroke. We speculate that metabolic syndrome, which has a widespread incidence across a diverse range of areas, from densely populated provinces to remote regions, may play a critical role in shaping these patterns [60, 61]. This complex interplay of regional characteristics, healthcare access, and metabolic factors warrants further investigation to better understand the disparities in disease incidence across Indonesia.
The network correlation analysis using Gaussian graphical model showed significant correlation of DM and hypertension with stroke. However, it is important to note that this model primarily identifies conditional dependencies among variables and does not establish causal relationships. We therefore performed spatial autoregressive model which subsequently confirms the significant role of DM as a key driver of stroke in Indonesia, with a strong positive association between DM incidence and stroke. This association, where an increase in DM incidence leads to a substantial rise in stroke cases within the same region and across neighboring regions, aligns with existing experimental and epidemiological evidence that underscores the role of hyperglycemia, insulin resistance, and associated vascular complications in increasing stroke risk [62, 63]. Notably, while hypertension is globally recognized as a major risk factor for stroke [64, 65], our findings indicate that DM exerts a stronger spatial influence on stroke incidence in Indonesia. The robust link between DM and stroke risk has been further substantiated by large-scale cohort data showing that DM independently doubles the risk of stroke, even in the absence of coronary artery disease [66].
A unique combination of genetic, behavioral, and environmental factors within the Indonesian population that amplifies the vascular damage caused by DM might explain this spatial pattern [38, 39]. For instance, the insulin receptor substrate-1 gene polymorphism Gly972Arg has been identified as a significant genetic risk factor for stroke among Indonesian individuals, supporting the hypothesis that insulin resistance–related genetic variation contributes to increased stroke susceptibility in this context [67]. Marriage between close relatives, which is still practiced in many parts of Indonesia [68, 69], may increase the likelihood of inheriting genetic risk factors for diabetes, including the Gly972Arg polymorphism [70, 71]. Additionally, elevated blood glucose levels, driven in part by dietary patterns such as high consumption of rice and sugary foods, have been shown to be significantly associated with stroke in the Indonesian population [72]. Moreover, emerging evidence highlights the association between DM, rather than hypertension, and the number and function of stem cells that influence stroke incidence and severity [73], further reinforcing this observation.
To effectively tackle the rising incidence of stroke, DM, and hypertension in Indonesia, particularly in high-risk areas identified in the study, the government should implement a multi-faceted public health strategy that includes enhancing healthcare access, promoting preventive health measures, and fostering community engagement. First, increasing the availability of healthcare facilities and services in provinces with high disease burdens, particularly those located in outside of Java Island is crucial. This could involve establishing mobile health clinics and telemedicine services to reach remote populations, as these approaches have been shown to successfully reduce all-cause mortality in several rural areas in Indonesia [74].
Additionally, the government should invest in public health campaigns focused on education about lifestyle modifications, including healthy eating and physical activity, to combat the risk factors associated with stroke. Collaborating with local communities and organizations to promote health literacy can empower individuals to make informed choices about their health. For instance, the implementation of Posbindu PTM, a community-based healthcare initiative, has significantly contributed in reducing the burden and increasing survival rate of NCDs in several cities in Indonesia by enhancing early detection efforts and fostering active community participation [75, 76]. Collaboration with local community nurses has been reported to effectively increase the knowledge and behavior of high-risk pregnant women and positively impact the rate of health care utilization [77]. Furthermore, establishing partnerships with non-governmental organizations and private sectors can enhance resource mobilization and create comprehensive health promotion initiatives tailored to the specific needs of each region [78].
Given the strong link between DM and stroke identified in this study, targeted interventions to manage DM must be prioritized [79]. These should include expanding access to DM screening programs, ensuring the availability of affordable medications such as insulin, and integrating DM management into primary healthcare services [80]. Moreover, implementing structured self-management education programs for DM patients, focusing on blood glucose monitoring, diet, and exercise, can significantly reduce complications, including stroke [10].
In high-incidence provinces such as Central Kalimantan, tailored interventions are urgently needed. Notably, participation in Prolanis (the Chronic Disease Management Program), a national initiative by BPJS Kesehatan to support chronic disease care, is significantly lower in regions outside Java, including Central Kalimantan [81]. This highlights the need for expanded access to Prolanis and other chronic care services in this province, particularly through mobile clinics and community-based outreach models. Given the widespread geographic barriers and limited availability of specialist care in many rural areas of Central Kalimantan, telemedicine presents a promising solution to improve access to consultations, follow-up care, and disease monitoring [82]. Furthermore, self-medication remains a common practice, particularly among the Dayak Ngaju, the largest ethnic group in Central Kalimantan [83]. To address this, targeted efforts to promote engagement with formal healthcare services should be prioritized through culturally appropriate health education, public awareness campaigns, and collaboration with local leaders and health workers.
This study has several limitations. First, while the use of nationwide data from BPJS Kesehatan provides comprehensive coverage of Indonesia’s population, the study is inherently limited to individuals registered as members of this insurance program. This exclusion of uninsured individuals or those using private insurance may result in an incomplete representation of the true burden of stroke, hypertension, and DM across the country. Additionally, some BPJS members might not utilize their insurance benefits for healthcare services, further contributing to potential underreporting of disease incidence.
Second, the reliance on population-level data from BPJS Kesehatan and BPS may introduce reporting biases or inaccuracies, particularly in regions with limited healthcare access or incomplete health records. These disparities could affect the spatial clustering and incidence estimates. Furthermore, while geospatial methods identified significant patterns and clusters, the influence of unmeasured socioeconomic, environmental, or genetic factors on disease incidence could not be fully accounted for in the analysis [84, 85]. Such unmeasured variables might confound the observed spatial associations and limit the generalizability of the findings.
In conclusion, our study highlights the critical role of spatial analysis in understanding the distribution and determinants of NCDs in Indonesia. The strong spatial association between DM and stroke underscores the urgent need for targeted public health strategies to combat the rising burden of these diseases. By focusing on regions with the highest incidence and addressing the unique risk factors within each, Indonesia can make significant strides in reducing the incidence of stroke and improving overall public health outcomes.
No datasets were generated or analysed during the current study.
We thank the BPJS Kesehatan and BPS for providing the data used in this study.
This study was funded by Hasanuddin University under grant number 00309/UN4.22/PT.01.03/2024.
This study was reviewed and approved by Ethics Committee of Hasanuddin University (869/UN4.6.4.5.31/PP35/2024). Informed consent was waived by the Ethics Committee.
This manuscript has been approved by all authors and is solely the work of the authors named.
The authors declare no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Zainuddin, A.A., Kadir, R.R.A., Kuswanto, H. et al. The major risk factor of stroke across Indonesia; a nationwide geospatial analysis of universal health coverage program. Arch Public Health 83, 169 (2025). https://doi.org/10.1186/s13690-025-01613-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13690-025-01613-4