BMC Research Notes volume 18, Article number: 141 (2025) Cite this article
To assess the patterns and determinants of harmful first aid practices in children with acute poisoning, and identify factors influencing caregivers' pre-hospital management.
This study included 384 children under 12 years, with 29.4% receiving harmful first aid measures. The most common poisoning agents were household chemicals (31.5%), followed by medicines (29.2%). First aid was provided to 29.4% of children, with water and coconut milk being the most common remedies. Harmful first aid was more likely in household chemical poisoning (p = 0.046). Univariate analysis revealed associations between harmful practices and factors such as low maternal education (p = 0.002), remote healthcare access (p = 0.0001), and cultural beliefs (p = 0.003). Multivariate analysis identified remote healthcare access (p = 0.001), low socio-economic status (p = 0.001), low maternal education (p = 0.03), and cultural beliefs (p = 0.05) as significant determinants. Qualitative findings revealed knowledge gaps, financial constraints, and cultural beliefs influencing first aid decisions, highlighting the need for targeted interventions.
Acute poisoning is a significant public health issue in children, especially in low- and middle-income countries, where exposure to toxic substances is often unintentional and preventable [1]. The administration of first aid by caregivers in the event of poisoning can significantly impact the outcome of the poisoning episode [2]. First aid, as defined by the International Liaison Committee on Resuscitation (ILCOR), is the immediate assistance provided to a sick or injured person until professional help arrives [3]. Despite the critical role of timely and appropriate interventions, caregivers often rely on home remedies or traditional practices, some of which may be harmful and delay proper medical treatment [4]. These harmful first aid practices can exacerbate the victim's condition and lead to complications, making it essential to understand the patterns and determinants influencing caregivers' decisions during such emergencies [5].
Traditional and culturally influenced first aid practices were frequently observed, with caregivers responding to poisoning by ingestion or inhalation by washing the affected area with water and soap or water alone. In cases of poisoning and bites, interventions such as rubbing metal on the bitten area, applying turmeric powder, and engaging in spiritual activities were commonly practiced, reflecting the strong influence of local beliefs on first aid responses [6]. The harmful effects of improper first aid, particularly gastric lavage, have been well-documented in resource-limited settings, with studies highlighting its association with increased risks of aspiration and other complications [7]. A study from India showed that potentially harmful first-aid practices were associated with an approximately five-fold increase in the risk of pulmonary aspiration [5]. In rural Sri Lanka, approximately one-third of caregivers have been reported to employ potentially hazardous first aid measures, such as inducing vomiting or administering substances such as coconut milk, which can exacerbate the child's condition and delay access to appropriate medical care [8]. Studies assessing first aid interventions by laypeople for acute oral poisoning emphasized the importance of effective measures to limit or delay toxin absorption before professional help arrives, whilst noting that inappropriate actions can exacerbate patient outcomes [2].
In this background, the current study aimed to assess the patterns and potential determinants of harmful first aid practices in children with acute poisoning in Sri Lanka. By identifying the types of first aid commonly administered and the factors that contribute to the choice of these practices, we aimed to highlight the gaps in caregivers' knowledge and the broader social, cultural, and systemic factors that influence their actions. The study also explored the association between caregiver education, access to healthcare, and the use of potentially harmful interventions.
This prospective observational cross-sectional study was conducted at the Anuradhapura Teaching Hospital, Sri Lanka, over a two-year period, including all children under 12 years presenting with acute poisoning, excluding food poisonings and snake/insect bites. Ethical approval was obtained from the Faculty of Medicine, University of Kelaniya, and Faculty of Medical and Allied Health Sciences, Rajarata University of Sri Lanka, with written informed consent from caregivers.
A structured data collection tool was developed, covering demographic characteristics, types of poisons, first aid practices, and potential determinants of first aid practices. The tool was created through collaboration with paediatricians, toxicologists, and public health experts to ensure content validity. Pretesting (n = 10) assessed tool clarity, feasibility, and relevance. Based on feedback, minor adjustments were made to improve clarity and comprehensiveness.
To ensure reliability, a single investigator collected all data throughout the study. This minimized variability and ensured consistent interpretation of clinical presentations and first aid practices. Inter-rater reliability was assessed during pretesting, with two independent investigators comparing their findings, resulting in high agreement (kappa > 0.85), confirming good tool reliability.
Based on the findings from G.N. Lucas’s study on plant poisoning in Sri Lankan children, which reported that approximately 29% of parents practiced harmful first-aid measures, the required sample size for the study was calculated [9]. Assuming a 95% confidence level, a proportion of 0.29, and a 5% margin of error, the minimum sample size needed for the study was 317 participants. First aid practices were classified as beneficial or harmful according to clinical guidelines, and caregivers' actions were cross-checked for consistency with best practices. Several variables were defined for the study. Low parental education was defined as an education level below grade 8, and low socioeconomic status was defined as a monthly income of less than 100 USD. Data were collected by interviewing the parents during their hospital stay. Statistical analysis was performed using Chi-square tests to explore associations between types of poisons, and first aid practices. Association between potential factors influencing administration of harmful first-aid was verified by logistic regression. This analysis aimed to identify determinants of potentially harmful first aid practices and assess the relationship between caregiver education, socio-economic status, and healthcare access with appropriate first aid administration. Data were analysed using SPSS 22.0.
Additionally, 40 parents participated in focused group discussions, guided by a theme guide. Parents were selected through a purposive sampling approach, aiming to ensure that participants had relevant experience regarding administering first-aid measures among children following the poisoning event. Specifically, parents of children who were exposed to potentially harmful first-aid measures were targeted to provide insights based on their lived experiences. To ensure diverse perspectives, we aimed to include parents from various socio-economic and educational backgrounds and rural settings. The sample size for the qualitative study was determined based on data saturation, where no new themes were emerging from the focus group discussions after a predetermined number of interviews. A total of seven focus group discussions were conducted, with an average of six parents per group, which allowed the investigator to reach a saturation point in the data analysis.
Qualitative data were analyzed to provide insights into caregivers’ beliefs, practices, and challenges related to first aid in poisoning cases. To enhance the rigor of the analysis, we employed a second-order thematic analysis, that involved the interpretation and contextualization of the initial themes generated during the data analysis process. The approach was grounded in the work of Braun and Clarke (2006), who described thematic analysis as a flexible, yet systematic method for identifying patterns within qualitative data [10]. Second-order analysis allowed for deeper insights by moving beyond surface-level themes to explore the underlying meanings and implications of the data. Furthermore, the validity and trustworthiness of the findings were ensured by adhering to the principles of transparency, consistency, and reflexivity in qualitative research [11].
During the two-year study period, 384 children presented with poisoning incidents, comprising 224 males (58.4%) and 160 females (41.6%). The majority of the children (308, 80.2%) were aged under four years. The types of poisons encountered were diverse, with household chemicals being the most common (121 cases, 31.5%), followed by medicines (112 cases, 29.2%), plants (65 cases, 16.9%), agricultural chemicals (37 cases, 9.6%), and miscellaneous substances (49 cases, 12.8%). The most common poisonous substances in each type of poisoning were kerosene oil (79 cases), paracetamol (39 cases), Jatropha curcas (22 cases), organophosphate insecticides (17 cases), and mosquito coils (15 cases). Among the 384 children, 234 (60.9%) developed symptoms following the poisoning event. The most frequently reported symptoms were gastrointestinal (96 cases, 25.0%) and respiratory (78 cases, 20.3%), highlighting the significant clinical burden of poisoning in this population.
There were 19 children (4.94%) with intentional poisoning. The mean ages of children with accidental and intentional poisoning were 3.2 and 10.1 years, respectively. All children with intentional poisoning were reported to have experienced acute psychological distress, and one child had a previous diagnosis of depression. Two children were diagnosed with attention deficit hyperactivity disorder. Low maternal education was associated with intentional poisoning (odds ratio = 3.46, p = 0.001).
First aid measures were administered by caregivers to 113 children (29.4%) following the recognition of a poisoning incident. The most common intervention was the administration of large amounts of water to induce vomiting, observed in 53 cases (13.8%). The second most frequent measure was the serving of coconut milk, which was used in 34 cases (8.9%). Other first aid practices included giving milk, soapy water, lime water, inserting a finger into the child's throat to induce vomiting, and thumping the child on the back. Table 1 displays the patterns of first aid measures used by caregivers after the poisoning event.
Ingestion of household chemicals was more likely to result in the administration of harmful first aid by caregivers (p = 0.046). Harmful first aid practices were notably less common in cases of medicine poisoning compared to other types of poisoning (p = 0.009). However, plant poisoning and pesticide poisoning individually did not show any significant difference compared to other types of poisons. Table 2 presents the Chi2 p-values for each type of poison, which were derived by comparing first aid versus no first aid for each type of poison separately, using individual 2 × 2 tables for each.
Complications of first aid practices included four cases of aspiration after drinking coconut milk following kerosene oil ingestion. Additionally, two children who were given large amounts of water after organophosphate ingestion developed pneumonia due to aspiration. In all these incidents, the caregivers were unaware of the potential harmful effects of the first aid measures they had administered.
Univariate analysis revealed significant associations between the administration of harmful pre-hospital first aid measures and potential determinants such as the child's asymptomatic status, low maternal education, limited access to remote healthcare, low socio-economic status, cultural beliefs, and transportation difficulties. No significant association was observed with intentional poisoning (p = 0.643) and low paternal education (p = 0.056) (Table 3).
Multi-variate analysis revealed that remote health care facilities (p = 0.001), low socio-economic status (p = 0.001), low maternal education (p = 0.03) and strong beliefs regarding cultural practices for cure (p = 0.05) as significant determinants of the practice of harmful first aid measures by caregivers following acute poisoning events.
Thematic analysis revealed several key themes. First, knowledge gaps emerged, with many parents unaware of the proper steps to take in case of poisoning and a reliance on traditional remedies. Second, perceived barriers to accessing healthcare included the distance to medical facilities and financial constraints. Third, cultural beliefs influenced parental decision-making, with some parents prioritizing home-based interventions over seeking professional medical treatment. Finally, a theme of emotional responses was evident, with parents often feeling panic and uncertainty during poisoning incidents, leading to delayed or inappropriate first-aid practices. The findings emphasized the need for targeted educational interventions to improve first-aid knowledge and promote timely medical attention in rural communities.
Harmful first aid practices in rural areas were deeply intertwined with accessibility challenges, cultural beliefs, and systemic inequalities. One caregiver explained, “We live in a remote area where transport is not available after 6 pm due to threats from elephants.” This statement highlights how environmental barriers, such as wildlife threats and poor infrastructure, exacerbate delays in accessing emergency care. Another mother recounted giving her child mashed nutmeg seeds to counteract the effects of Jatropha poisoning, guided by her own mother’s advice: “We did not know it can also be poisonous.” Such instances underline the reliance on traditional practices when professional help is out of reach, driven by a combination of panic, cultural norms, and the absence of formal first aid education.
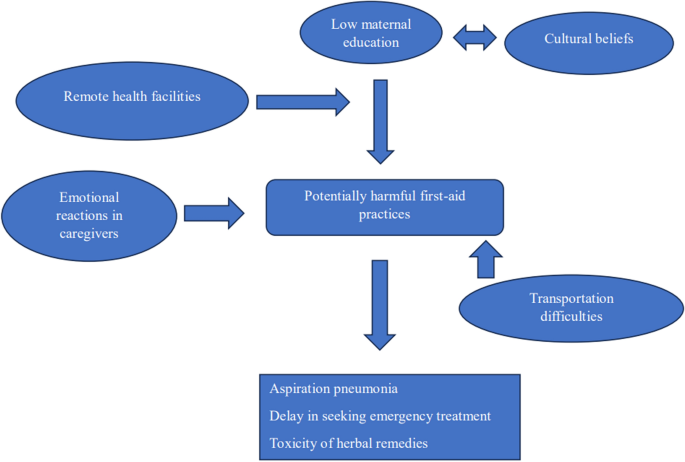
Social and educational factors also played a critical role in shaping these practices (Fig. 1). Caregivers with lower levels of education often misinterpreted symptoms and rely on anecdotal knowledge. One participant noted, “We thought giving something natural would reduce the effect of the poison.” However, harmful outcomes from such interventions are more common in households with limited health literacy. Additionally, the lack of social support networks further isolates families in emergencies, as illustrated by the infrequent transport services and poor road conditions in these areas. Addressing these challenges requires a multi-faceted approach that integrates cultural sensitivity, improved accessibility, and targeted education.
Cause-and-effect relationships in the practice of home remedies by caregivers for acute poisoning in children
Our study reveals several key patterns of harmful first aid practices among caregivers of children with acute poisoning. The most common interventions included administering large amounts of water to induce vomiting (13.8%) and offering coconut milk (8.9%), both of which have no proven therapeutic benefit and can lead to further complications such as aspiration and choking. These practices are often influenced by cultural beliefs and traditional remedies that have been passed down through generations [12]. For instance, coconut milk is commonly perceived as a "natural" antidote, despite its ineffectiveness in treating most poisons [13]. Similarly, caregivers often resort to inducing vomiting by finger insertion, unaware of the risks of aspiration, especially in children with compromised airways due to poisoning [14].
The findings of this study regarding first-aid practices for pediatric poisoning align with several previous studies conducted in similar settings, yet also highlight important differences. For instance, our results indicate a significant reliance on household remedies, which has been observed in other low-resource contexts5,6. However, while some studies from urban Sri Lanka have shown a lower prevalence of such practices [15], our study in rural settings demonstrates that the lack of access to formal healthcare options and the limited awareness of correct first-aid procedures contribute to these practices. Additionally, the influence of community norms and familial practices, identified in our study, aligns with findings from other qualitative studies, suggesting that social and cultural factors play a central role in health-related decision-making [16]. This comparison underscores the importance of context when developing educational interventions for poisoning management, highlighting the need for tailored approaches that address local beliefs and resource availability.
The study identified several determinants that were significantly associated with the administration of harmful first aid practices. One of the most striking findings was the strong correlation between low maternal education (less than grade 8) and the use of harmful first aid (p = 0.001). Caregivers with lower educational levels were more likely to rely on traditional and anecdotal knowledge, often misinterpreting symptoms and opting for potentially harmful remedies [17]. This underscores the need for targeted educational interventions that address gaps in knowledge and provide clear guidance on appropriate first aid for childhood poisoning [18].
Another key factor influencing harmful first aid practices was geographic location. Caregivers from remote areas, where access to healthcare facilities is limited, were more likely to administer inappropriate first aid (p < 0.0001). Delays in seeking professional care due to transportation difficulties, particularly in rural areas where roads are poor and transportation services are infrequent, exacerbate the reliance on home remedies[19]. One caregiver’s statement—“We live in a remote area where transport is not available after 6 pm due to threats from elephants”—highlights the environmental and logistical challenges faced by families in rural settings.
In this study, cultural beliefs surrounding caregiving and first aid practices played a significant role in shaping the way parents and caregivers responded to poisoning incidents. The integration of qualitative findings with quantitative results provide valuable insights into how local traditions, cultural norms, and societal practices influenced caregivers' understanding and management of poisoning events in children. For example, in many rural Sri Lankan communities, there was a belief that home remedies, such as administering herbal concoctions or using traditional methods such as rubbing the affected area with certain oils, could help alleviate symptoms of poisoning. These cultural practices may often be prioritized over evidence-based medical interventions, potentially delaying proper treatment. Additionally, the perception that poisoning was caused by supernatural forces or bad omens in certain communities could lead caregivers to hesitate in seeking medical attention, relying instead on spiritual or community-based solutions. The qualitative data from focused group discussions revealed that caregivers, particularly those with low education, were unaware of the potential dangers of certain home remedies. As one mother explained, “We thought giving something natural would reduce the effect of the poison,” reflecting the widespread misconception that natural substances are inherently safe and beneficial. The observations further highlight the need for targeted educational interventions that address both medical knowledge and cultural practices to improve outcomes in poisoning management.
These findings emphasize the importance of improving caregiver education and access to reliable medical information. Health promotion programs that address cultural beliefs, educate caregivers on safe first aid practices, and improve healthcare accessibility could significantly reduce the incidence of harmful first aid practices [20, 21]. Additionally, efforts to enhance the transportation infrastructure in remote areas could facilitate quicker access to medical care, thus preventing the need for home-based remedies. Further, it is important to recognize that children who experience intentional poisoning may require mental health support due to the psychological distress associated with such incidents. A more detailed analysis of the mental health needs of these children is crucial for informing appropriate interventions and providing holistic care.
This study has several limitations that should be considered when interpreting the findings. First, the study focused on children under 12 years of age, which excludes adolescents and may not fully capture the broader patterns of poisoning and first aid practices. The reliance on caregiver self-reporting for data collection could also introduce recall bias, as caregivers may not accurately remember or may underreport harmful first aid practices. Furthermore, the study did not explore the long-term outcomes or follow-up of children after receiving harmful first aid, which would be valuable for understanding the full impact of such practices. These limitations suggest the need for further studies with larger, more diverse samples and long-term follow-up to better understand the broader implications of harmful first aid practices in childhood poisoning cases.
This study highlights the prevalence of harmful first aid practices in children with acute poisoning, particularly in rural areas of Sri Lanka, where caregivers face challenges such as low education, limited access to healthcare, and reliance on traditional remedies. Significant associations were found between harmful first aid practices and factors such as low maternal education, remote healthcare access, and cultural beliefs. To mitigate these risks, we recommend implementing culturally appropriate educational interventions tailored to caregivers in rural communities. Community-based workshops, school-based awareness programs, and the integration of first aid training into maternal and child health initiatives could significantly improve caregivers' knowledge and practices. Additionally, strengthening the role of public health midwives in disseminating accurate first aid information and ensuring the availability of simplified, evidence-based guidelines in local languages could enhance awareness and adoption of safe practices. Future research should explore the long-term health outcomes of children exposed to harmful first aid measures, evaluating potential complications and healthcare utilization patterns. Additionally, studies assessing the effectiveness of various educational interventions in changing caregiver behaviors could provide valuable insights into optimizing preventive strategies. Addressing systemic barriers such as healthcare accessibility and emergency transportation challenges in remote areas should also be a priority for future policy initiatives. By combining education, community engagement, and systemic improvements, we can reduce the burden of harmful first aid practices and ensure that children with acute poisoning receive timely and appropriate care.
The data that support the findings of this study are available from the authors but restrictions apply to the availability of these data, which were used under license from Anuradhapura Teaching Hospital, sri Lanka for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request.
The authors of this study acknowledge the director of Anuradhapura Teaching Hospital, Sri Lanka included in this study for granting permission for data collections.
No funding was received.
Permission to carry out the study was obtained from the Ethics Review Committee, Faculty of Medicine, University of Kelaniya and Faculty of Medical and Allied Health Sciences, Rajarata University of Sri Lanka. Written informed consent was obtained from parents of all children prior to recruitment of children in the study. The study procedures were done in accordance with the Declaration of Helsinki.
Not applicable.
The authors declare no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Dayasiri, K. Patterns and determinants of potentially harmful first aid practices in children with acute poisoning. BMC Res Notes 18, 141 (2025). https://doi.org/10.1186/s13104-025-07234-y