BMC Cancer volume 25, Article number: 927 (2025) Cite this article
To evaluate the effects of individualized PEEP on pulmonary function, cerebral blood flow, and postoperative cognitive function in patients undergoing laparoscopic radical resection of rectal cancer.
100 patients who underwent laparoscopic radical rectal cancer surgery at our hospital between August 2021 and May 2023 were randomized into two groups: the DP group (optimal PEEP group oriented to driving pressure) and the Cdyn group (optimal PEEP group oriented to pulmonary compliance). Anesthesia was induced in both groups with 0.3 mg/kg of remizolam + 0.15 mg/kg of CIS atracurium + 0.5 ug/kg of sufentanil. Lung ultrasound score (LUS), peak and plateau airway pressures (PEAK, PLAT), oxygenation index (OI), driving pressure (DP), and pulmonary dynamic compliance (Cdyn) were measured at different time points. Cerebral blood flow and cognitive function were also assessed. T0: before induction of anesthesia; T1: before postoperative extubation of the tracheal tube; T2: 1 h after extubation; T3: on the third postoperative day; T4: 5 min after determining the optimal PEEP; T5: 1 h after the establishment of pneumoperitoneum; T6: 2 h after the establishment of the pneumoperitoneum; T7: 20 min at the end of pneumoperitoneum.
There were no significant differences in general information between the two groups, P > 0.05. Compared with the DP group, the Cdyn group had lower LUS at T3, higher PEAK at T5, T6, and T7, lower PLAT and OI at T6 and T7, lower DP at T4, T6, and T7, and lower Cdyn at T6 and T7, P < 0.05. The Cdyn group had lower cerebral blood flow at T4 and T6, P < 0.05. The Cdyn group had higher cognitive function at stage T3 as assessed by MMSE, P < 0.05.
PEEP guided by lung compliance improves pulmonary function, cerebral blood flow, and cognitive function, offering clinical benefits.
Colorectal carcinoma is a common pernicious tumor with high morbidity and mortality. The clinical characteristics of the disease mainly include the depth of invasion, lymph node metastasis, organ metastasis, vascular invasion, etc. [1]. With the continuous progress of clinical medical technology, laparoscopic technology is more and more widely used in clinics, especially for patients with colorectal carcinoma, which has the advantages of good safety and low trauma [2–3]. However, due to the special anatomical location of colorectal cancer, carbon dioxide gas needs to be injected into the intra-abdominal cavity during surgery in order to form a pneumoperitoneum so as to ensure a clear surgical field and full exposure. This operation leads to an increase in intra-abdominal pressure, which causes the diaphragm to shift upward and the volume of the chest cavity to decrease, ultimately leading to a decrease in the compliance of the lungs. Studies have shown that pneumoperitoneum can result in a 1 to 3 cm shift of the diaphragm and a reduction in lung volume [4]. At the same time, the increase in intra-abdominal pressure causes an increase in intrathoracic pressure, which in turn affects the mechanics of the respiratory system, resulting in a significant increase in peak and plateau airway pressures [5]. This pathophysiologic change may not only trigger an increase in intracranial pressure, but also negatively affect lung function, leading to an increased risk of complications such as pulmonary atelectasis [6–7]. In this context, the use of PEEP protective ventilation strategy is particularly important, which can effectively improve ventilation, reduce the probability of local alveolar collapse caused by compressed air tissue in the lungs, provide the necessary compensatory pressure for collapsed alveoli, promote alveolar re-expansion, optimize pulmonary hemodynamics, and reduce the phenomenon of pulmonary vascular shunting. However, due to the limitations of research and individualized differences in clinical practice, the fixed PEEP setting is often not suitable for all patients. Compared with fixed PEEP, individualized PEEP has significant advantages in improving respiratory mechanics and reducing the frequency and severity of atelectasis [8]. At present, there are many ways to set individualized PEEP in the clinic. Studies have shown that PEEP guided by lung compliance can greatly improve respiratory mechanics, increase oxygen supply, and help reduce ventilator-associated lung injury and postoperative atelectasis [9–10]. Nowadays, the two methods have not been studied simultaneously in clinics. Based on this, this study applied the two different methods to With the continuous progress of clinical medical technology, laparoscopic technology is more and more widely used in clinics, especially for patients with colorectal carcinoma, which has the advantages of good safety and low trauma undergoing laparoscopic radical resection of rectal carcinoma, in order to provide a more optimized scheme for guiding the best positive end expiratory pressure in clinical practice, so that patients can obtain lung protection to the greatest extent, and better improve patients’ postoperative lung function.
All of 100 patients who underwent laparoscopic radical resection of rectal carcinoma in our hospital from August 2021 to May 2023 were regarded as the study objects. The sample size used in this study was determined based on the expected effect size, significance level, statistical power, and available resources. Based on previous experiments and literature review, the expected effect size was estimated to be medium, the significance level was set at 0.05, and the statistical power was set at 0.80. Using the G*Power software, it was calculated that a minimum of 45 participants were needed for each group. To enhance the robustness of the study, the final sample size for each group was set at 50 participants. This sample size was considered statistically sufficient to detect a medium effect. The patients were randomly divided into two groups: DP group (the best PEEP group guided by driving pressure) and Cdyn group (the best PEEP group guided by lung compliance). Inclusion criteria: ① Patients who aged 60–80; ② ASA classification was class II-III; ③ Patients with complete clinical data; ④ Patients with normal pulmonary function before operation. Exclusion criteria: ① Patients with respiratory illnesses (chronic obstructive pulmonary illness, asthma, pulmonary bullae, recent upper respiratory tract infection, previous history of chest surgery); ② Patients with obstructive sleep apnea syndrome; ③ Patients with serious liver and kidney illnesses; ④ Patients with atelectasis and conversion to laparotomy before operation. This study was conducted in accordance with the ethical regulations of the Declaration of Helsinki. The study was approved by the Ethics Committee of Zhangjiakou First Hospital (approval number: 2023-KY-48). Written informed consent was obtained from all patients before their participation in the study.
Guidance method
In the DP group, driving pressure was used to guide the best PEEP: PEEP was increased from 2cmH2O in steps (2, 3, 4,5, 6, 7, 8, 9, 10 cm H2O). After each PEEP level was maintained for 10 respiratory cycles, the airway plateau pressure of each PEEP level in the last respiratory cycle was recorded in turn, and the driving pressure was calculated. The best individualized PEEP was determined by selecting the PEEP value corresponding to the lowest driving pressure [11].
In the Cdyn group, lung compliance was used to guide the best PEEP: PEEP decrement titration was performed under the guidance of lung compliance [12]: After PEEP = 16cmH2O was set to maintain five ventilation cycles, PEEP was down regulated with 2 cmH2O as a step until PEEP = 0, and each PEEP level was maintained for five ventilation cycles and then lung compliance was recorded; the PEEP value corresponding to the maximum lung compliance was set as the optimal individualized PEEP for patients. Lung compliance: VT/ (PEAK-PEEP).
The different time intervals for maintaining PEEP in the two groups were based on the following considerations: In the DP group, a longer time was needed to accurately calculate the driving pressure and find the PEEP level corresponding to the lowest driving pressure. In the Cdyn group, the maximum lung compliance could be quickly reached and recorded after starting from a higher PEEP level and reducing it stepwise, so a shorter time interval was sufficient.
Anesthesia method
Anesthesia induction: It was performed by Remifentanil of 0.3 mg/kg + CIS atracurium of 0.15 mg/kg + sufentanil of 0.5ug/kg; anesthesia maintenance: It was performed by Remifentanil of 0.1~0.2ug/kg/min + CIS atracurium of 1~2ug/kg/min + remidazolam of 1~3mg/kg/h.
Observation indexes
The lung ultrasound scores (LUS) were detected before anesthesia induction (T0), before tracheal catheter withdrawal after surgery (T1), 1 h after extubation (T2), and the third day after surgery (T3), and the levels of peak airway pressure (PEAK), plateau airway pressure (PLAT), oxygenation index (OI), driving pressure (DP), and pulmonary dynamic compliance (Cdyn) were detected at 5 min after the determination of the best PEEP (T4), 1 h after the establishment of pneumoperitoneum (T5), 2 h after the establishment of pneumoperitoneum (T6), and 20 min at the end of pneumoperitoneum (T7);observation of T0, T4, and T6 middle cerebral artery flow velocities in two groups of patients; the points of Mini Mental State Examination (MMSE) at T3 were observed in the two groups.
Scoring criteria
Lung ultrasound was performed by using an eub-5500 ultrasound machine. The patient’s chest was divided into 12 lung areas by the anterior axillary line, the posterior axillary line, and the 1 cm line on the double nipples. The LUS of each lung area was 0–3 scores, and the scores of 12 examination areas accumulated into the whole lung LUS, with a full points of 0–36 scores. The larger the point, the more serious the atelectasis was; the MMSE scoring included 30 items, including language, memory, calculation, attention, memory and orientation, with a total score of 30 points. Cognitive impairment was defined as MMSE score ≤ 23 points.
SPSS 22.0 statistical software was used for processing and statistically analyzing the experimental data. The measurement data were expressed in the form of mean ± standard deviation (‾χ ± s), and the independent sample t-test was used for comparison between the two groups; count data were expressed in the form of percentage (%), and conducted with χ2-test. P < 0.05 was set as the distinction with statistical significance.
It had no obvious distinction in the general data of age, gender and BMI between the 2 groups, with P > 0.05, see Table 1.
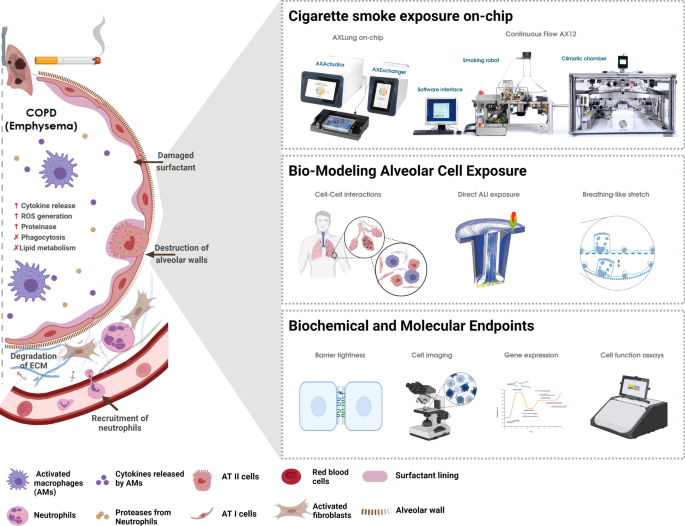
① In the comparison of LUS between the two groups, the difference between the T1 and T2 time periods was not statistically significant, P > 0.05, and in the T3 time period, the Cdyn group was lower than the DP group, P < 0.05, as shown in Table 2; Fig. 1A. This suggests that PEEP settings guided by pulmonary compliance are more effective in reducing pulmonary atelectasis, and that they contribute to improved patient oxygenation status and a lower incidence of postoperative pulmonary complications. ② In the comparison of PEAK between the two groups, the difference between the T4 time period was not statistically significant, P > 0.05, and in the T5, T6 and T7 time periods, the Cdyn group was was higher than the DP group, P < 0.05, see Table 3; Fig. 1B. This may be due to the improved lung tissue recuperation and compliance in the Cdyn group after optimization of PEEP, which resulted in relatively higher airway pressures at the follow-up stage. And this higher airway pressure did not lead to significant lung injury, but instead may have helped to maintain the open state of the alveoli. ③ In the comparison of PLAT between the two groups, the difference in the T4 and T5 time periods was not statistically significant, P > 0.05, and in the T6 and T7 time periods, the Cdyn group was lower than the DP group, P < 0.05, see Table 4; Fig. 1C. This suggests that the PEEP settings in the Cdyn group were able to better balance alveolar expansion and pressure distribution. The lower plateau pressure helps to reduce the risk of alveolar over-expansion and decreases the probability of ventilator-associated lung injury. ④ In the comparison of OI between the two groups, the difference in the T4 and T5 time periods was not statistically significant, P>0.05, in T6 and T7 time period, the Cdyn group was lower than the DP group, P<0.05, see Table 5; Fig. 1D. This suggests that the PEEP setting in the Cdyn group can improve oxygenation more effectively. Good oxygenation status is crucial for postoperative patient recovery, which can reduce the incidence of postoperative hypoxemia and decrease multi-organ dysfunction due to hypoxia. ⑤ In the comparison of DP, the difference between the two groups was not statistically significant in T5 time period, P>0.05, and in T4, T6 and T7 time period, the Cdyn group was lower than the DP group, P<0.05, see Table 6; Fig. 1E. This suggests that the PEEP settings in the Cdyn group were able to lower the driving pressure more effectively. Lower driving pressures help to reduce the cyclic opening and closing of the alveoli, reducing the risk of lung injury, as well as improving ventilation efficiency. ⑥ In the comparison of Cdyn in the two groups in the T4 and T5 time periods, the difference was not statistically significant, P > 0.05, and the Cdyn group was lower than the DP group in the T6 and T7 time periods, P < 0.05, see Table 7; Fig. 1F. This suggests that the PEEP settings in the Cdyn group were better able to maintain lung compliance. Higher lung compliance helps to reduce respiratory work, increase ventilation efficiency, and improve patients’ respiratory function.
The lung function compared between the 2 groups. Note: A is LUS scoring, B is PEAK, C is PLAT, D is OI, E is DP, and F is Cdyn
In the comparison of middle cerebral artery flow velocities between the two groups, the difference in the T0 time period was not statistically significant, P > 0.05, and in the T4 and T6 time periods, the Cdyn group was lower than the DP group, P < 0.05, as shown in Table 8; Fig. 2. This may be because the PEEP settings in the Cdyn group improved the regulatory mechanisms of cerebral blood flow. Appropriate PEEP optimizes the balance between intracranial pressure and cerebral perfusion pressure and reduces the impact of increased intracranial pressure on cerebral blood flow caused by laparoscopic surgery. This optimized cerebral blood flow state helps to reduce the incidence of postoperative cognitive dysfunction.
In the comparison of MMSE in T3 time period between the 2 groups, the Cdyn one was greater than the DP one, with P < 0.05, see Table 9; Fig. 3. This suggests that the PEEP settings in the Cdyn group can better protect the cognitive function of postoperative patients. Postoperative cognitive dysfunction is one of the common complications after laparoscopic surgery, and by optimizing PEEP settings, the incidence of postoperative cognitive dysfunction can be reduced and the quality of life of patients can be improved.
Laparoscopic surgery is one of the treatment methods for the late stage of rectal cancer. For the therapy of patients with advanced colorectal carcinoma, radical surgery is currently the preferred method [13–14]. According to the researches, the use of PEEP protective ventilation strategy can effectively improve ventilation, so at present, many foreign scholars are committed to the research of PEEP protective ventilation strategy [15–16]. As we all know, due to the differences of bodies, the situation of each patient is different, so fixed PEEP cannot be applied to all people [17–18]. Compared with the fixed PEEP, individualized PEEP can improve patients’ lung compliance during surgery. This is because individualized PEEP selects the best PEEP according to the patients’ respiratory system and other competitive physiological factors. It is more in line with the physiological characteristics of the body, resulting in higher compliance of the lungs and the balance between alveolar collapse and expansion, thereby improving oxygenation and reducing the probability of local collapse caused by compressed air tissues of the lungs [19–20]. Therefore, this study focuses on the effects of individualized PEEP on patients undergoing laparoscopic radical resection of rectal carcinoma. The results of this study showed that individualized PEEP guided by lung compliance had a positive impact on cerebral blood flow. In the comparison of middle cerebral artery flow velocities between the two groups, the Cdyn group was lower than the DP group in the T4 and T6 periods. This may be because appropriate PEEP can improve intrathoracic pressure, thereby affecting cerebral blood flow dynamics. However, the specific mechanism needs further research.
At present, different scholars have studied the different ways to guide the best positive end expiratory pressure, and the researches have shown that [21,22,23] lung compliance is used to determine the appropriate PEEP for patients in lumbar fusion surgery. The results have shown that individualized PEEP guided by lung compliance can effectively improve the local collapse caused by the compressed lung air tissues, reduce the release of inflammatory factors caused by mechanical ventilation, and improve the body’s inflammatory response. And some researches have found [9, 24, 25] that the application of lung compliance-guided individualized PEEP titration during robotic-assisted radical prostate cancer surgery can reduce alveolar overexpansion while attenuating lung injury, protect the alveolar capillary barrier, prevent damage to alveolar epithelial cell integrity, improve lung compliance, and make a lower concentration of inflammatory factors, which then attenuates the inflammatory response. Other scholars have shown that [26–27] the research on the impact of individualized PEEP under the guidance of lung compliance on adverse reactions and complications in obese patients after laparoscopic surgery shows that compared with fixed PEEP, individualized PEEP can reduce intraoperative driving pressure, improve oxygenation, and will not affect the hemodynamic stability. In addition, PEEP individualized titration guided by driving pressure could decrease the incidence of LUS and atelectasis in elderly patients undergoing laparoscopic radical resection of colorectal carcinoma, improve respiratory mechanics and oxygenation function, and the lung protective effect will not disappear immediately after extubation. However, compared with fixed PEEP, single individualized PEEP optimization does not significantly reduce lung function injury [28–29]. Based on this, in order to provide a more optimized scheme for guiding the best positive end expiratory pressure in clinical practice, the following experiments were carried out on patients: first, the clinical data of the 2 groups were observed, and the outcomes showed that there was no obvious distinction in the general data of age, gender and BMI between the 2 groups. This shows that the two groups of patients are comparable, and the accuracy of the results is strong. In addition, this study also observed LUS scores, the levels of PEAK, PLAT, OI, DP, and Cdyn in different time periods; the VM, RI and MMSE scores of the 2 groups at distinct time periods were observed. The results showed that: in the comparison of LUS between the 2 groups, the Cdyn one was lower than the DP one in T3 time period; in the comparison of PEAK between the two groups, the Cdyn group was higher than the DP group in the T5, T6, and T7 periods; in the comparison of PLAT between the 2 groups, the Cdyn one was less than the DP one at T6 and T7 periods; in the comparison of OI between the 2 groups, the Cdyn one was less than the DP one at T6 and T7 periods; in the comparison of DP between the 2 groups, the Cdyn one was less than the DP one at T4, T5, T6 and T7 periods; in the comparison of Cdyn between the 2 groups, the Cdyn one was greater than the DP one at T6 and T7 periods; in the comparison of middle cerebral artery flow velocities between the two groups, the Cdyn group was lower than the DP group in the T4 and T6 periods; in the comparison of MMSE in T3 time period between the 2 groups, the Cdyn one was greater than the DP one. The above results indicate that PEEP guided by lung compliance can improve patients’ lung function, cerebral blood flow and cognitive function. Therefore, this study applied two different ways to patients undergoing laparoscopic radical resection of rectal carcinoma, explored the impacts of the two ways in guiding individualized PEEP on lung function of patients undergoing laparoscopic radical resection of rectal carcinoma, and applied lung ultrasound to evaluate the lung condition of patients during operation, which is technically innovative. In this study, the two methods were simultaneously applied to guide the best PEEP for patients undergoing laparoscopic radical resection of rectal carcinoma. By comparing the intraoperative and postoperative pulmonary ultrasound scores and respiratory mechanics indexes of the two groups of patients, it was concluded that the PEEP guided by lung compliance had a better effect on patients and could improve their quality of life.
In conclusion, PEEP guided by lung compliance can reduce atelectasis, increase pulmonary oxygenation, improve postoperative pulmonary function and cognitive function, and accelerate the rehabilitation of patients. Nevertheless, this research also has some shortcomings. First, the sample size was relatively small and it was a single-center study, which may limit the generalizability of the results. Second, the follow-up period was relatively short, and the long-term effects of individualized PEEP on patients’ pulmonary function and cognitive function remain to be further studied. Third, although the risks associated with the temporary increase in PEEP were monitored, the sample size may not be sufficient to fully evaluate the incidence and impact of rare adverse events. Future studies should address these limitations by conducting multicenter trials with larger sample sizes, longer follow-up periods, and more comprehensive risk assessments.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
We thank the members of Zhangjiakou First Hospital for helpful discussions. We apologize to the scientists whose work could not be cited due to space limitations.
Zhangjiakou City 2023 Municipal Science and Technology Plan Self raised Fund Project 2322185D. Zhangjiakou City 2023 Municipal Science and Technology Plan Self funded Project 2322089D.
This study was conducted in accordance with the ethical regulations of the Declaration of Helsinki. The experiments were admitted to the Zhangjiakou First Hospital Ethics Committee. The number of the Ethics Committee’s acceptance is: (2023-KY-48).
All patients signed the informed consent form.
The authors declare no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Zhang, X., Zhang, J., Zhao, C. et al. Effects of individualized PEEP on pulmonary function, cerebral blood flow and postoperative cognitive function in patients undergoing laparoscopic radical resection of rectal cancer. BMC Cancer 25, 927 (2025). https://doi.org/10.1186/s12885-025-14321-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-025-14321-7