BMC Psychiatry volume 25, Article number: 552 (2025) Cite this article
Depression and Type 2 Diabetes Mellitus (T2DM) represent significant public health challenges and share common pathogenic mechanisms. Previous studies have indicated a positive correlation between serum residual cholesterol (RC) and depression. However, further research is needed to understand the relationships between RC and depression, T2DM, and their coexistence. This study aims to assess the association between RC and depression, T2DM, and their comorbidities in a large sample of the U.S. population, while also exploring potential underlying mechanisms.
This is a cross-sectional study utilizing data from the National Health and Nutrition Examination Survey (NHANES) spanning from 2005 to 2018 (N = 11,193). Depression was assessed using the Patient Health Questionnaire-9 (PHQ-9). We employed weighted univariate and multivariate logistic regression models, considering sampling weights, to explore the associations between serum RC and depression, T2DM and their coexistence. To assess model stability, we calculated unmeasured confounder E values. Restricted cubic spline regression models were used to reveal dose–response effects, and subgroup analyses were conducted.
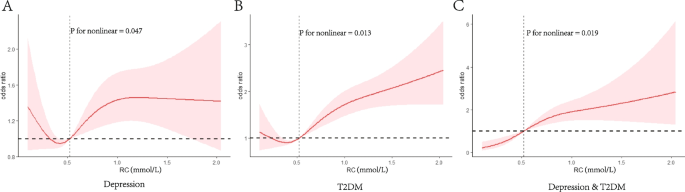
Among the 11,193 participants, the weighted mean age was 45.24 years, with 49.0% being male. The prevalence of depression, T2DM, and their coexistence was 6.9%, 14.0%, and 1.4%, respectively (weighted percentages). In the multivariate regression model, higher serum RC levels were associated with an increased risk of depression, T2DM, and their coexistence. The adjusted odds ratios (ORs) per unit increase in RC were 1.39(1.06,1.82), 2.26(1.79,2.83), and 3.07(2.08,4.52), respectively. When considering only depression without T2DM, the association was not significant (OR: 1.23; 95% CI: 0.87–1.73). This nonlinear correlation between RC and depression, T2DM, and their coexistence was consistent across various participant characteristics.
The findings from this extensive cross-sectional study offer compelling evidence linking RC to the risk of depression, T2DM, and their coexistence. This implies that directing attention towards residual cholesterol could enhance research pertaining to the comorbidities of depression and type 2 diabetes.
In recent years, the global prevalence of type 2 diabetes (T2DM) and depression has progressively increased, emerging as a critical public health challenge [1, 2]. Furthermore, its intricate pathogenic mechanisms involve a complex interplay of neurotransmitters, inflammation, and hormonal levels [3]. The escalating global challenge of comorbid diabetes and depression underscores the urgency of understanding their interconnectedness [4]. Epidemiological research [5, 6] consistently demonstrates that individuals with chronic conditions, notably diabetes, face a twofold increased risk of developing mental health comorbidities such as depression and anxiety [7, 8]. This heightened risk adversely affects both the quality of life and outcomes for individuals managing diabetes [9,10,11,12]. Thus, it becomes imperative to identify modifiable risk factors associated with the coexistence of depression, T2DM, and the concurrent manifestation of these two conditions.
Recent years have witnessed a growing body of research uncovering the intricate relationship between physical and mental health, especially concerning risk factors for psychiatric disorders like lack of exercise, overweight, and lipid abnormalities [13,14,15] and various conditions, including depression [16], cognitive impairment [17], frailty [18], as well as potential risk factors for hypertension [19] and T2DM [20]. Nonetheless, these relatively limited studies predominantly focus on individual diseases rather than considering the coexistence of two conditions. This prompted us to explore factors associated with depression, type 2 diabetes and their coexistence in a comprehensive, large-scale study.
In the study of cholesterol metabolism, serum residual cholesterol (RC), especially recent studies, not only plays a crucial role in the endocrine system [21,22,23,24,25], but also plays an important role in the nervous system [16,17,18]. Cholesterol serves as a vital component of neuronal cell membranes, and its variations may directly impact the stability and signal transmission of neurons. The levels of serum RC may be associated with the risk of depression by influencing the normal functioning of the nervous system. The potential mechanisms through which RC may contribute to depression in conjunction with T2DM remain unclear. Moderate evidence indicates the accumulation of RC in the vascular wall, activating monocytes and leukocytes, ultimately resulting in arterial wall inflammation and a multi-level cellular immune response [26]. Considering that inflammatory responses are generally considered foundational to the development of depression and diabetes [27,28,29], this study hypothesizes that RC may play a crucial role in the relationship between comorbidities like depression and type 2 diabetes.
Our study aims to utilize data from the National Health and Nutrition Examination Survey (NHANES) spanning 2005 to 2018. It delves deeply into the intricate connections among RC, depression, and T2DM. The overarching aim is to unveil innovative perspectives and insights conducive to preventing and treating the concurrent occurrence of depression and T2DM, thereby fortifying the underpinnings of clinical practice.
The datasets generated and analyzed during the current cross-sectional study are available on the NHANES website: https://wwwn.cdc.gov/nchs/nhanes/Default.aspx. Extensive household interviews were conducted, gathering population baseline information and health questionnaire data. Physical examinations and blood sample collection occurred at a mobile examination center (MEC), with serum specimens stored at −30 °C until transport to the Laboratory Sciences Division of the National Center for Environmental Health at the Centers for Disease Control and Prevention for testing. Detailed specimen collection and handling procedures are outlined in the NHANES Laboratory/Medical Technician Procedures Manual (LPM). The study population comprised adults (≥ 20 years old) from NHANES 2005–2018, all having completed interviews and assessments at the MEC. Selection criteria included availabilities of total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C) data, as well as comprehensive diagnostic information on depression and T2DM. Exclusions were made for patients with cancer (n = 1441) and those with a weight of 0 (n = 738). Participants with incomplete covariate data (n = 1977) were excluded. A total of 11,193 participants (5,696 female and 5,497 male) were included in the final analysis (Fig. 1). Post-weighting, these participants represent approximately 162,799,954 individuals in the United States. The NHANES survey protocol received approval from the National Center for Health Statistics Research Ethics Review Committee, and all participants provided written informed consent.
In NHANES, we utilized the Patient Health Questionnaire (PHQ-9), a 9-item screening instrument measuring the frequency of depressive symptoms in the past 2 weeks, to assess participants'depressive status [30]. Each of the 9 items employs a 4-point scale: 0 ("not at all"), 1 ("a few days"), 2 ("more than half the time"), and 3 ("almost every day"), yielding a total score ranging from 0 to 27. A cut-off score of ≥ 10 was employed for inclusion in the depression group, indicating moderate to severe depressive symptoms, with an 88% sensitivity and specificity for major depression [31]. Cases of T2DM were defined through self-reported questionnaires and the criteria established by the American Diabetes Association [32]. The criteria encompassed FPG ≥ 126 mg/dL, glycosylated hemoglobin (HbA1c) ≥ 6.5%, 2-h plasma glucose from an oral glucose tolerance test (OGTT) ≥ 200 mg/dL, current use of insulin or diabetes pills for glucose control, and self-reported questionnaire data indicating a physician diagnosis of diabetes.
Serum levels of TC, HDL-C, and LDL-C were evaluated in participants who had fasted for over 8.5 h but less than 24 h at the NHANES laboratory. Specifically, TC was determined through enzymatic assays, HDL-C through immunoassays, and LDL-C was derived using the Friedewald calculation: [LDL-C] = [TC]—[HDL-C]—[triglycerides/5]. Triglyceride concentration in serum or plasma was assessed using the timed-endpoint method. According to the 2019 guidelines from the European Society of Cardiology and European Atherosclerosis Society (ESC/EAS), RC is calculated by subtracting HDL-C and LDL-C from TC [33]. Normal blood lipid levels were defined as TC < 5.18 mmol/L, HDL-C ≥ 1.04 mmol/L, and LDL-C < 3.37 mmol/L [34].
The NHANES database encompasses lifestyle information and personal medical history obtained through standardized questionnaires. It includes data on age, gender, race/ethnicity, education level, marital status, poverty income ratio (PIR), body mass index (BMI), smoking status, drinking status, waist circumference, healthy eating index (HEI), dietary inflammation index (DII), as well as laboratory results, including TC, HDL-C, and LDL-C. In the collinearity analysis, we found that BMI and waist circumference were collinearity, so we did not consider waist circumference as one of the covariables that needed to be adjusted.
Race/ethnicity was classified as Mexican–American, non-Hispanic white, non-Hispanic black, other Hispanic, or other. Educational level was divided into not graduated from high school, graduated from high school, and college or higher. Following standardized protocols, BMI was calculated as weight in kilograms divided by height in meters squared and categorized as < 25.0, 25.0 ~ 30.0, and ≥ 30.0 kg/m2. Smoking status was defined as current (having smoked at least 100 cigarettes throughout their lifetime and continuing to smoke cigarettes currently), former (having smoked in the past but having quit at the time of the interview), never (having smoked fewer than 100 cigarettes in their lifetime). Drinking status was defined as current (having had at least 12 drinks per year during their lifetime), former (having had ≥ 12 drinks in 1 year and not drinking last year, or not drinking last year but having had ≥ 12 drinks in a lifetime), or never (having had < 12 drinks in a lifetime). HEI is a metric designed to evaluate whether a set of foods aligns with the Dietary Guidelines for Americans (DGA) and comprises 13 food components [35].The study utilized the most recent version of the DGA from 2015. DII is a dietary tool derived from literature, employed to gauge the overall inflammatory potential of an individual's diet [36].
The NHANES utilizes a complex multi-stage stratified sampling design. We applied weights employing the"Fasting Subsample 2 Year MEC Weight."Given that our data spanned seven cycles, we divided the weight value by 7 to establish sampling weights for the 7-year cycle combination [37].
Univariate and multivariate logistic regression analyses were employed to evaluate the independent association between RC and the risk of depression, T2DM, and their coexistence. An extended logistic model approach was applied for different covariates. Additionally, utilizing a multifactorial logistic regression with the reference group being individuals without both T2DM and depression, we assessed the risk associations of RC with only depression, only T2DM, and the comorbidity of both. Descriptive analyses were conducted for all participants based on RC tertiles. Categorical variables are presented as weighted frequencies (%). For continuous data, normal distributions were conveyed as mean ± standard deviation (SD), and skewed data were presented using median and interquartile range (IQR), as applicable. Variables were compared through one-way ANOVA (normal distribution) and Kruskal–Wallis (skewed distribution) tests, along with the chi-square test for categorical variables.
The relationships between RC and depression, T2DM, and their coexistence were investigated using a restricted cubic spline regression model. Additionally, subgroup analyses were stratified by relevant effect covariates, considering variables such as age (< 60 years vs. ≥ 60 years), gender (female vs. male), BMI (< 25, 25–30, or ≥ 30 kg/m2), smoking status (current, former, never), and drinking status (current, former, never). To further assess the stability of all logistic regression models, we computed the E-value defined as the minimum strength of association on the odds ratio scale that an unmeasured confounder must have with both RC and the dependent variable (depression, T2DM and their coexistence) to fully suppress the observed association, conditional on the measured covariates.
All analyses were conducted utilizing the statistical software packages R4.2.2 (http://www.R-project.org, The R Foundation) and the Free Statistical software version 2.0 [38]. A significance level of P < 0.05 was deemed statistically significant, employing a two-tailed test.
The age of all participants was 45.24 ± 0.27 years and 49.0% were male. the weighted median serum RC level was 0.52 (95% CI: 0.36, 0.75) mmol/L. Detailed characteristics of the population as determined by RC tertiles are shown in Table 1. Age, race/ethnicity, education level, marital status, BMI, waist circumference, HEI, DII, smoking status, drinking status, and concomitant disease such as depression, hypertension and T2DM were significantly different between the serum RC different groups. Those with older age and with a higher BMI and waist were likely to have higher RC levels, with males having somewhat higher RC levels. The prevalence of depression, T2DM, and their coexistence was 6.9%, 14.0%, and 1.4%, respectively (weighted percentages). The prevalence of T2DM, hypertension and depression &T2DM among participants increased relatively with increasing RC. In addition, baseline features were compared between excluded and included data (Supplementary Table S1) to assess the impact of lost follow-up and missing data on the results.
Univariate logistic regression analysis is presented in Supplementary Table S2. Using the variance inflation factor (VIF) method to test for multicollinearity, a VIF of two or higher indicates multicollinearity. All the variables have no multicollinearity in depression,T2DM and their coexistence (Supplementary Table S3). Table 2 showed that after adjusting for different confounders, RC was positively associated with depression, T2DM and their coexistence in all three models. In the non-adjusted model, RC was significantly associated with an increased risk of depression (OR, 1.68; 95% CI, 1.34–2.11), T2DM(OR, 3.28; 95% CI, 2.79–3.86) and their coexistence(OR, 4.30; 95% CI, 3.14–5.89). After adjusting for sociodemographic characteristics, including age and gender (model 1) and plus with education level, PIR, race/ethnicity, marital status (model 2), similar association patterns were observed. When further adjusted for BMI, smoking status, drinking status, DII, HEI, and hypertension (model 3), the adjusted ORs and 95% CIs for per unit increase in RC were 1.39(1.06,1.82), 2.26(1.79,2.83), and 3.07(2.08,4.52), for the risk of depression, T2DM and their coexistence. Additionally, as depicted in Fig. 2, there was a positive association between RC and the risks of depression, T2DM, and their coexistence (P for nonlinear < 0.05). We further adjusted the physical activity variable (Supplementary Table S4) and the results remained the same.
Restricted cubic spline curves of remnant cholesterol concentrations in NHANES 2005–2018 (N = 11,193). Notes: A Depression, B T2DM, C Depression and T2DM. Odd ratios were adjusted for age, gender, education level, PIR, race/ethnicity, marital status, BMI, waist circumference, smoking status, drinking status, DII, HEI, and hypertension
Simultaneously, we assessed the relationship between RC and the risk of depression only, T2DM only, and their comorbidities. This was done through multivariate logistic regression, utilizing a reference group comprising individuals without T2DM and depression (Table 3). RC was still significantly associated with risk in T2DM only (OR: 2.19; 95% CI: 1.72–2.79) and comorbid groups (OR: 3.78; 95% CI: 2.44–5.84), when considering only depression without T2DM, the association was not significant (OR: 1.23; 95% CI: 0.87–1.73) after full model adjustment.
As shown in Table 4, RC was significantly and positively associated with T2DM and depressive co-morbid T2DM when TC was less than 5.18 mmol/L, with adjusted ORs and 95% CIs of 2.47(1.89,3.22), 3.64(2.23,5.96), respectively, and not in depression (OR,1.19; 95% CI, 0.78–1.82). Positive correlations consistent with the above ranges persisted when HDL-C and LDL-C were at normal levels (HDL-C ≥ 1.04 mmol/L and LDL-C < 3.37 mmol/L), with adjusted ORs and 95%CIs of 2.42(1.82,3.21) and 2.14(1.69,2.72) in T2DM, and in both coexistence the adjusted ORs and 95%CIs were 3.56(2.06,6.14) and 3.08(1.90,4.98) respectively, and similarly the correlations were not significant in depression, where the adjusted ORs and 95%CIs were 1.31(0.92,1.86) and 1.29(0.93,1.79) respectively.
Subgroup analyses were performed to assess the effect of serum RC (per 1-unit increment) on depression, T2DM, and their coexistence which were stratified by different variables (Fig. 3). Although subgroup analyses were performed according to confounders such as age (< 60 or ≥ 60 years), gender (female or male), BMI (< 25, 25–30, or ≥ 30 kg/m2), smoking status (current, former or never), drinking status (current, former or never) and hypertension (no or yes), we did not observe interactions significantly associated with the risk of depression except for in the subgroup smoking status (all P values for interactions were > 0.05), serum RC and depression risk appear to be significantly associated in current and previous smokers. Meanwhile, we did not observe an interaction between RC and in the risk of T2DM except in gender, which seems to have a greater OR in female. We did not observe any interaction between RC and the risk of both co-morbidities (all P values for interactions were > 0.05).
In addition, in the sensitivity analysis, the E values were 2.13,3.95, and 5.59, respectively, suggesting that in order to explain the observed OR of 1.39, 2.26 and 3.07, unmeasured confounders need to be associated with RC and dependent variables (depression, T2DM, and comorbidities) with an OR of at least 2.13,3.95, and 5.59 (Supplementary Fig. 1).
Our study results demonstrate a significant association between RC and depression, T2DM, and the comorbidity of these two conditions, but not in depression only without T2DM. Even when TC, HDL-C, and LDL-C levels are within the normal range, the positive correlation between T2DM and the comorbidity with depression remains, although the relationship with depression risk is not significant.
Consistent with the majority of previous research, our findings indicate an increased risk of depression [16] and T2DM [39] with elevated RC levels. RC makes up a third of total cholesterol and 50% of the cholesterol in atherosclerotic plaques [40, 41], and is linked to several diseases [24, 42,43,44,45]. Elevated RC may contribute to depression by activating the HPA axis. It also makes the arteries more permeable, allowing RC to be absorbed by macrophages more easily than LDL [46]. These macrophages release IL-6, which stimulates the HPA axis [47] and is connected to depression. RC may also trigger inflammation [48] and damage to blood vessels [49], worsening depression [50]. Our study was not significant in depression risk alone, this may be related to the more complex association between lipids and depression, and we can further conduct Mendelian randomization analysis to see if there is a causal relationship.
In a nationwide population-based cohort study, RC was recognized as an independent predictor of T2DM [21]. The degradation and metabolism of RC by lipoprotein lipase can produce free fatty acids and monoacylglycerol, initiating an inflammatory response and thereby causing diabetes [51].The surplus residual lipoprotein in plasma has the ability to infiltrate the arterial wall and be assimilated by macrophages and smooth muscle cells, leading to foam cell formation and eliciting mild inflammation, thereby contributing to elevated blood glucose levels [52, 53]. Additionally, RC exhibits a close association with insulin resistance [54], wherein the arterial retention of residual lipoprotein isolates intensifies insulin resistance, resulting in hyperglycemia [55, 56].
Our findings suggest that elevated RC may increase the risk of the comorbidity of depression and T2DM. Growing evidence supports a shared biological origin between depression and T2DM, particularly related to congenital immune overactivation leading to cytokine-mediated inflammatory responses, possibly through HPA axis dysregulation [57]. Throughout the lifespan, these pathways may contribute to increased risks of insulin resistance, depression, T2DM, and elevated mortality rates. Patients with type 2 diabetes experience alterations in cerebral microcirculation, marked by increased blood–brain barrier permeability and changes in blood flow regulation. When depression is triggered, microvascular dysfunction may contribute to alterations in metabolic mechanisms [58]. Ultimately, deepening our understanding of the common origins of depression and diabetes may enable simultaneous treatment and improvement of both conditions.
Until now, the prevailing clinical indicators for assessing lipid levels have included total cholesterol, HDL-C, and LDL-C. Nevertheless, our study unveils that, despite these three indicators being within the normal range, RC remains linked to the risk of T2DM and its comorbidities, with the exception of the risk of depression. Some studies propose that the non-HDL-C index might be more efficacious in predicting the risk of diabetes compared to traditional cholesterol indices like LDL-C [23, 59, 60]. Moreover, heightened RC levels may instigate inflammation and contribute to coronary artery disease, whereas elevated LDL-C, in addition to contributing to coronary heart disease, may also be implicated in elevating the risk of depression in the T2DM population [61]. Hence, even with normal lipid levels, attention to RC is warranted for further prevention of associated comorbidities.
This study boasts several strengths, First, we employed a large, nationally representative sample of adults in US. Second, we took into account and adjusted for known and potential variables. Third, the researchers looked at relationships between RC and risk of depression, T2DM, and their coexistence. In addition, we also performed a dose–response analysis to assess the relationship between them. However, the study has certain limitations. First, we could not draw causal conclusions regarding the pathogenesis of RC with depression, type 2 diabetes, and their coexistence due to the cross-sectional nature of the study design. Second, the depression was scored using a PHQ-9, an interview questionnaire format that may limit the robustness and comprehensiveness of depression evaluations, although the PHQ-9 score is considered useful for standards-based diagnosis of depression and other mental disorders common in primary care [31]. Third, the effect of unmeasured covariates, such as dietary patterns, medication use, stress levels and the history of depression and diabetes treatment cannot be excluded and may bias the results, although we have adjusted for as many covariates as possible. Moreover, we computed E-values to demonstrate that unmeasured confounders are likely not able to offset the reported associations. Fourth, the cholesterol measurement methods used by private healthcare institutions may vary, and since the RC value is derived through calculation, it may be subject to potential overestimation or underestimation compared to direct measurement. Finally, the generalizability of these findings is likely limited to the U.S. population. Considering the characteristics of our study sample, caution is advised when applying these findings to younger populations, and future studies with broader samples are warranted. Although NHANES participants are selected using a multi-stage, multi-stratified probabilistic design, mitigating selection bias to some extent [62], additional prospective trials are indispensable to validate our findings in diverse populations.
This study demonstrates a substantial positive association between RC values and the risk of depression, T2DM, and their co-existence, although the relationship with the risk of depression alone is not significant. Notably, these positive associations persisted in T2DM and comorbidities even when TC, HDL-C, and LDL-C levels were normal. Our findings propose that RC can serve as a lipid predictor for depression, T2DM, and their comorbid conditions, offering novel insights into preventive strategies. Future prospective longitudinal studies are needed to investigate the relationship between RC and these comorbidities.
No datasets were generated or analysed during the current study.
- NHANES:
-
National Health and Nutrition Examination Survey
- Ref:
-
Reference
- OR:
-
Odds ratio
- IQR:
-
Interquartile range
- PIR:
-
The ratio of family income to poverty
- BMI:
-
Body mass index
- RC:
-
Remnant cholesterol
- DII:
-
Dietary inflammation index
- HEI:
-
Healthy diet index
- T2DM:
-
Type 2 diabetes
- TC:
-
Total cholesterol
- LDL-C:
-
Low-density lipoprotein cholesterol
- HDL-C:
-
High-density lipoprotein cholesterol
- MEC:
-
Mobile examination center
- HbA1c:
-
Glycosylated hemoglobin
- OGTT:
-
Oral glucose tolerance test
- VIF:
-
Variance inflation factor
We thank Jie Liu, PhD (Department of Vascular and Endovascular Surgery, Chinese PLA General Hospital & Physician-Scientist Center of China) for his helpful review and comments regarding the manuscript.
This work was supported by the Science and Technology Research Programme of the Health Commission of Hebei Province (No. 20231986) and the Science and Technology Research Programme of the Health Commission of Hebei Province (No. 20241385).
The survey protocol was approved by the Research Ethics Review Board of the National Center for Health Statistics (https://www.cdc.gov/nchs/nhanes/irba98.htm). The NCHS Research Ethics Review Board reviewed and approved.
NHANES, and all survey participants provided written informed consent. Therefore, no further ethical approval and informed consent were required.
NHANES 2017–2018 | Protocol #2018–01 (Effective beginning October 26, 2017) |
Continuation of Protocol #2011–17 (Effective through October 26, 2017) | |
NHANES 2015–2016 | Continuation of Protocol #2011–17 |
NHANES 2013–2014 | Continuation of Protocol #2011–17 |
NHANES 2011–2012 | Protocol #2011–17 |
NHANES 2009–2010 | Continuation of Protocol #2005–06 |
NHANES 2007–2008 | Continuation of Protocol #2005–06 |
NHANES 2005–2006 | Protocol #2005–06 |
Not applicable.
The authors declare no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Mao, Y., Zhao, R., Li, X. et al. Association of remnant cholesterol with depression, type 2 diabetes, and their coexistence. BMC Psychiatry 25, 552 (2025). https://doi.org/10.1186/s12888-025-06980-4