BMC Psychology volume 13, Article number: 618 (2025) Cite this article
To evaluate the effectiveness of Culturally Adapted Cognitive-Behavioral Therapy (CA-CBT) compared to standard CBT in alleviating depression in college students.
A randomized trial was conducted on college students with mild to moderate depression. The CA-CBT group (21 students) received a group CA-CBT intervention incorporating idioms, while the standard CBT group (20 students) received a standard group-based CBT intervention. Both group interventions were conducted once a week, with each session lasting one and a half hours, for a total duration of eight weeks. Eighteen students from the standard CBT group and 12 from the CA-CBT group completed the trial. Depressive symptoms, cognitive distortions, emotional regulation, and CBT understanding were assessed at baseline, week five, post-treatment, and three months after post-treatment using validated scales. Data were analyzed using repeated measures ANOVA, t-tests, and chi-square tests via SPSS 26.0.
The repeated measures ANOVA results for the pre-treatment and post-treatment showed a significant interaction effect of time and intervention and a significant main effect of time for the sleep disturbance factor of the Hamilton Depression Rating Scale. However, only the main effect of time was significant for all other variables. T-tests indicated that the CA-CBT group had significantly lower Hamilton scores at follow-up compared to the standard CBT group. Meanwhile, the standard CBT group had significantly better CBT understanding post-treatment. Except for the above two items, no other significant difference were found by T-test.
Compared with standard CBT, the CA-CBT group that incorporates idioms is beneficial for college students with depressive symptoms to continue to achieve relief for a certain period of time after the end of treatment. Specifically, this relief may be reflected in the improvement of sleep problems. However, CA-CBT did not better improve participants’ emotion regulation, understanding of cognitive behavioral therapy, or reduction of cognitive distortions.At the same time, the CA-CBT group did not perform better than the standard CBT group in terms of dropout rate, treatment satisfaction, recommendation, and re-use rate.
The trial was registered on the Chinese Clinical Trial Registry (No. ChiCTR2300074752||http://www.chictr.org.cn/) on August 15, 2023.
Cognitive Behavioral Therapy (CBT) is a pivotal, evidence-based psychological intervention in current use, combining the principles of behavioral and cognitive therapies. Its behavioral framework is grounded in three prominent learning theories: classical conditioning, operant conditioning, and social learning theory, while cognitive therapy, as described by Beck [4], fundamentally emphasizes the role of dysfunctional thought patterns that negatively influence clients’ emotional states and behaviors. Thus, the core objective of CBT is to address these dysfunctional cognitions and assist clients in cultivating more adaptive ways of thinking [6].
Most contemporary psychotherapeutic techniques were originally developed by Western scholars for use in the Western context, and thus many psychologists have subsequently sought to tailor these approaches to other cultural contexts. This necessity arises from research indicating that cultural variances can affect both the therapeutic relationship and the efficacy of treatments [32, 46].
Culturally Adapted Cognitive Behavioral Therapy (CA-CBT), as described by Naeem et al. [33], involves the modification of CBT through the addition of culture-specific knowledge, insights, and skills, while retaining its foundational principles. The framework for culturally adapting psychotherapy was first introduced by Bernal et al. [8], prompting a surge of studies exploring how CBT can be tailored for minority populations [17]. This led to a gradual revolution in CA-CBT research worldwide. Scholars have identified several reasons for the need to culturally adapt CBT. First, the core of CBT intervention lies in adjusting clients’ maladaptive core beliefs, intermediate beliefs, and automatic thoughts, and the content of these three components may vary across different cultures. Recognizing these cultural nuances can thus result in more effective interventions [49, 43]. Second, using non-adapted CBT (i.e. standard CBT) may increase the likelihood of dropout rates and adverse treatment outcomes [31, 37]. For example, according to a meta-analysis by Ng and Wong [34], although standard CBT has a moderate short term effect in treating depression/well-being (Hedges’g = 0.53) in Chinese individuals, this effect is lower than what has been reported in previous studies on depression(Hedges’s g = 1.58 for BDI, Hedges’s g = 1.69 for HRSD, [22]). Furthermore, their study revealed that the effect was stronger when the CBT treatment was culturally adapted (g = 0.60) than when the CBT treatment was not culturally adapted (g = 0.44). Third, CBT’s focus on individual relationships often clashes with Eastern cultural values that prioritize family and community perspectives [40]. In light of these considerations, numerous studies have advocated for the cultural adaptation of CBT [1, 36]. Recent years have witnessed significant global advancements in research on the cultural adaptability of CBT, but Chinese studies in this area remain in their infancy. Although some researchers have investigated overseas Chinese populations, there are still few studies on how CBT can be adapted to Chinese culture [29]. A review of existing CA-CBT studies shows that many begin by using traditional cultural resources, highlighting elements that align with CBT principles to modify its application [28]. For example, several studies have integrated metaphors and proverbs from traditional culture into CBT.
Chinese culture is vast and deep, with idioms serving as distinctive linguistic constructs. These idioms, typically formed with four characters, originate from mythology, folklore, poetry, and music and serve to effectively convey life experiences and philosophies. When compared to other cultural expressions such as poetry, idioms prove to be characteristically concise yet dense with meaning. Their appeal lies in their broad acceptance, reaching wide audiences and promoting cultural flexibility. Prior studies connecting idioms with psychology have uncovered significant psychological insights embedded within them. For example, Li [25] highlighted idioms illustrating the relationship between cognition and emotion, such as “心烦意乱” (“uptight”) and “情急智生” (“desperate wisdom”). In terms of cognition and behavior, phrases like “行成于思” (“action follows thought”) and “知行并举” (“unity of knowledge and action”) stand out. Such interaction of cognition, emotion, and behavior aligns well with the foundational principles of Cognitive Behavioral Therapy (CBT), indicating a very promising opportunity to integrate Chinese idioms into CBT practices. Hwang, Wood, et al. [19] noted the value of idioms in connecting CBT concepts to Chinese cultural contexts for Chinese Americans. In addition, researchers in China aiming to adapt CBT for cultural relevance have similarly emphasized the importance of idioms [45, 48]. Moreover, numerous studies on CA-CBT have consistently regarded proverbs as essential for cultural adaptation [18, 21].
Depression is currently a significant global mental health challenge. A systematic review conducted in 2017 found that depressive disorders are the predominant mental health concern worldwide, ranking among the top five contributors to years lived with disability [51]. Depression adversely affects individuals’ psychological well-being and social functionality [23], while also imposing considerable financial and emotional strains on their families [50]. In China, depression ranks high among mental health issues, and incidence rates have risen over recent decades [14]. Notably, college students are known to be a high-risk demographic for depression. Research by Wang et al. [53] found that the prevalence of depressive symptoms in college students was 24.71%, underscoring the urgent need to prioritize the mental health of that population. A meta-analysis contrasting the effectiveness of cognitive-behavioral therapy (CBT) in China against that in other nations found that CBT offers remarkable advantages for the Chinese student cohort [26]. In addition, the aforementioned meta-analysis by Ng and Wong reported a Hedges’ g effect size of 0.53 for CBT’s impact on depression in Chinese individuals. This effect size is notably lower than the 1.02 as observed by [41] and the 0.82 as reported by Gloag [13]. Of the various therapeutic modalities, group CBT has demonstrated efficacy in alleviating depressive symptoms in college students and mitigating their depression risk [2, 35].
Given these facts, we assert that modifying Cognitive Behavioral Therapy (CBT) using idioms as a focal point and researching university students who exhibit depressive symptoms is worthwhile.
This study aims to assess the efficacy of a CA-CBT treatment program as compared to standard CBT. We hypothesize that CA-CBT will more effectively reduce depressive symptoms in Chinese college students than standard CBT. In addition, we expect the CA-CBT to correct cognitive distortions more significantly, improve emotional regulation skills more efficiently, and enhance the understanding of CBT to a greater degree. Furthermore, we predict higher acceptance rates and lower dropout rates for the CA-CBT group compared to the standard CBT group.
This study focuses on college students with mild to moderate depression symptoms, as these individuals can receive psychological treatment without a need for medication. The inclusion criteria for participants were thus as follows: 1. current college or graduate students; 2. age between 18 and 30 years; 3. Beck Depression Inventory score ranging from 5 to 20, and Hamilton Depression Rating Scale score between 7 and 24; and 4. willing to participate in the study. The criteria for exclusion were: 1. presence of suicide risk; 2. currently using psychiatric medication; and 3. a history of mental health issues. The criteria for withdrawal were: 1. presence of suicide risk and 2. initiation of psychiatric medication. The trial was registered on the Chinese Clinical Trial Registry (No.ChiCTR2300074752||http://www.chictr.org.cn/) on August 15, 2023.
First, the Beck Depression Inventory (BDI) was used as a tool for subject recruitment and preliminary screening [42], with questionnaires distributed through outreach to various university psychological centers and online platforms. Based on the scoring guidelines of the Beck Depression Inventory, a score ranging from 5 to 15 was taken to be indicative of mild to moderate depressive symptoms. Due to the challenges in subject recruitment during the initial phase, the upper threshold for inclusion was revised to a score of 20, as this was one standard deviation above the mean of the collected data. Consequently, scores between 5 and 20 were deemed acceptable for progression to the subsequent stage, while individuals scoring above 20 were deemed to have depressive symptoms too severe for participation and thus were advised to seek for other professional assistance. For applicants who passed pre-screening and were interested in participation, the researchers then conducted online assessments via video or audio, using the Hamilton Depression Rating Scale (HAMD) alongside established exclusion criteria. According to the Chinese version of the psychiatric rating scale manual compiled by Zhang and He [57], participants with Hamilton scores between 7 and 24 are classified as experiencing mild to moderate depressive symptoms and did not meet the exclusion criteria were invited to take part in the formal experiment. Those who consented to participate were required to sign an informed consent form and were assigned a registration number in the online database.
Once participant recruitment was completed, a randomization procedure was used to assign participants to either the CA-CBT or standard CBT group, as well as to determine the corresponding treatment schedules. According to sample size, the participants were planned to divided into two groups: a CA-CBT group and a standard CBT group, each ideally comprising 18 participants, with 9 for every small group within the CA-CBT group and the standard CBT group. A randomization website (www.random.org) was used to randomly generate a sequence of numbers. For example, in response to the input “1–36”, the website will generate a random sequence such as “3, 8,11,…,15”, which was evenly divided into two halves. A random person was then invited to decide whether the first or second half of the sequence would participate in the CA-CBT group or the standard CBT group. The randomization procedure for the treatment time was the same. Following the randomization process, participants were notified of the treatment location and schedule. The treatment spanned a total of eight weeks, with one session conducted each week, administered by a senior cognitive-behavioral therapy (CBT) therapist affiliated with a specialized mental health institution.
A pre-treatment assessment was administered prior to the initiation of the first treatment session (T1). A mid-treatment evaluation was conducted during the fifth week of treatment (T2), which exclusively used the Beck Depression Inventory and the Hamilton Depression Rating Scale. To mitigate potential experimenter bias, the Hamilton scale was administered by two other members of the research team (who were unaware of the group allocation), as well as a psychology graduate student who was unaware of the group allocation.
At the conclusion of the eight-week treatment period (T3), a post-treatment assessment was conducted, incorporating the same assessments as used at T1. At that time, the participants were invited to provide feedback regarding their satisfaction with the treatment program, their likelihood of re-engaging with the treatment, and their propensity to recommend it to others. The same evaluators who administered the Hamilton questionnaire also administered the mid-treatment assessment. Participants who successfully completed all eight treatment sessions were eligible to receive a transportation subsidy of one hundred yuan.
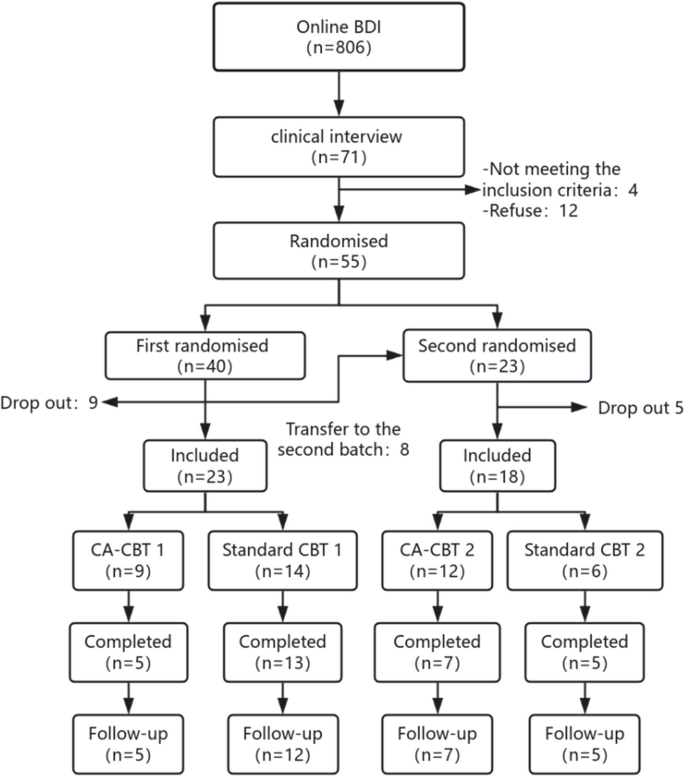
A follow-up assessment was scheduled to take place three months post-treatment (T4), using the same questionnaire as was used in T1. This follow-up measurement was administered online, with researchers distributing the electronic version of the questionnaire to each of the participants, who were asked to complete and return it within one week. Additionally, the Hamilton questionnaire was administered by the same two members of the research team who administered it in prior assessments. The participation of subjects at each stage of the study is shown in Fig. 1.
The CA-CBT group participated in a treatment program that used idiomatic expressions, which were selected based on the results of prior experimental studies. The main screening structure can be found in Xu et al. [56]. In this earlier investigation, a three-phase screening process was used to identify idioms from an idiom dictionary that corresponded with the principles of Cognitive Behavioral Therapy (CBT). These idioms were subsequently validated through assessments conducted with approximately 900 college students, who evaluated their familiarity, comprehensibility, and other attributes. The idioms that received favorable ratings were used to develop the treatment program of the current study, which comprises eight distinct modules.
The standard Cognitive Behavioral Therapy (CBT) group participated in a conventional CBT treatment program with 8 modules that did not use idiomatic expressions. The comparison between the CA-CBT group and the standard CBT group is shown in Table 1.
Beck depression inventory 13-item version (BDI-13)
The Beck Depression Inventory (BDI), created by Aaron Beck, is a self-assessment tool based on Beck’s theory of depression [5]. The original version comprised 21 items, but a shortened form with 13 items was developed in 1972 [3]). Each item is scored on a four-point Likert scale from 0 to 3, for a total range of 0 to 39, with scores of 0–4 indicating no symptoms, 5–7 suggesting mild depression, 8–15 denoting moderate depression, and 16 or higher signifying severe depression. Higher scores indicate more severe depressive symptoms. The Chinese BDI-II has a Cronbach’s α of 0.9 [54], item correlations from 0.18 to 0.71, and individual item correlations with the overall scores ranging from 0.56 to 0.82. Test–retest reliability is satisfactory, with a correlation coefficient of 0.55 (p < 0.05). The correlation between the BDI-13 and BDI-II is also strong, at 0.96. In this study, the Cronbach’s α of this scale was 0.863.
Hamilton Depression Rating Scale (HAMD) [16]
Hamilton created this scale in 1960 as an essential tool for the clinical assessment of depression. This study used the 17-item version, with most items scored on a 5-point scale (0 to 4) and some items scored on a 3-point scale (0 to 2). The assessment generates a total score and five factor scores: Anxiety/Somatization, Weight, Cognitive Impairment, Retardation, and Sleep Disturbances. Higher scores reflect more severe depression. Inter-rater reliability for this scale ranges from 0.88 to 0.99 (p < 0.01), with a validity coefficient of 0.92, indicating strong reliability and validity (Zhang & He). In this study, the Cronbach’s α of this scale was 0.655.
Cognitive Distortion Questionnaire (CDQ) [30]
This scale comprises 15 items on cognitive distortions, evaluated by the Cognitive Therapy Society. These items reflect negative thought patterns that are similar to Beck’s concepts. Each item is scored using a matrix table, with frequency on the horizontal axis and intensity on the vertical axis. The scale of each of these two dimensions is 0–3 points, but the score range of each item is 0–5 points, with 0 = never or don’t believe, and 3 = always or very much believe. Thus, total frequency and intensity scores range from 0 to 45, with an overall score from 0 to 75, and higher scores indicating more severe distortions. The scale shows high internal consistency, with a Cronbach’s α of 0.85. The alpha coefficients for the three factors are 0.84, 0.62, and 0.58. The test–retest reliability (ICC) for the total scale is 0.85, with factor ICCs of 0.83, 0.86, and 0.92, reflecting strong reliability and validity [39]. In the current study, the Cronbach’s α of this scale was 0.947.
Short version of the difficulties in emotion regulation scale (DERS-16)[10]
This scale, created by Gratz and Roemer, comprises 16 items measuring five dimensions: emotional clarity, goal-directed behavior, impulsive control, emotion regulation strategies, and emotional acceptance. Each dimension features two, three, three, five, and three items, respectively, making it ideal for clinical trials requiring repeated assessments. All items are scored on a five-point Likert scale, with higher scores reflecting greater emotion regulation difficulty. Reliability and validity testing indicate internal consistency reliability at 0.91 and test–retest reliability at 0.90. Item-total correlations range from 0.51 to 0.72 (p < 0.01), with factor analyses confirming the five-dimensional structure of the scale [52]. The Cronbach’s α of this scale in this study was 0.937.
Self-administered CBT Comprehension Questionnaire
There is currently no effective questionnaire for measuring an individual’s understanding of CBT, and so we developed a new questionnaire for this study. Grounded in Beck’s theory, it includes six questions covering two dimensions: recognition of core CBT concepts and daily application frequency. Higher scores indicate better understanding of CBT This non-standardized tool evaluates participants’ CBT use. The Cronbach’s α of this scale was 0.58.
To determine the necessary sample size, Gpower was used with the following parameters: repeated measures ANOVA, between factors, effect size = 0.5, α = 0.05, power = 0.95, number of groups = 2, number of measurements = 4, and a correlation of 0.5 among repeated measures. According to Cohen [11], an effect size of 0.5 is considered medium.That explains why we choose 0.5 as the effect size. Meanwhile, also according to Cohen [11], while a power of 0.80 is generally considered sufficient for most behavioral research, a higher power value of 0.95 can be used in certain studies where a higher degree of precision is required to reduce Type I errors.The results indicated a necessary total sample size of 36 individuals.
This study compared the demographic information and pre-treatment scores on each scale between the two groups using independent samples t-tests, to ensure that the CA-CBT and standard CBT groups were balanced at baseline.
In addition, repeated measures ANOVA was conducted on the total and subscale scores of all questionnaires to assess the within-group, between-group, and interaction effects of time x group. Independent samples t-tests were performed to compare the mean scores between the CA-CBT and standard CBT groups at each time point. All analyses were conducted using SPSS 26.0.
Concurrently, the reliable change index (RCI) was calculated for the BDI scores of the CA-CBT group and standard CBT group at pre- and post-treatment time points, to ascertain whether the treatment had had a clinically significant effect. In accordance with the criteria set forth by Jacobson and Truax [20], a participant was deemed to have achieved a clinically significant improvement if their RCI value exceeded 1.96. In accordance with the findings of Seggar et al. [44], a difference of 8.46 between pre- and post-treatment BDI scores was considered to be indicative of a clinically significant change (either improvement or worsening) in depression. Consequently, the proportion of subjects in the CA-CBT and standard CBT groups exhibiting clinically significant improvement (defined as a decrease in BDI scores of ≥ 8.46 and post-treatment BDI scores of < 14), improved but not significantly (defined as a decrease in BDI scores of < 8.46), no significant change (defined as no change in BDI scores), and aggravated (defined as an increase in BDI scores) were calculated to ascertain the clinical treatment effect of CA-CBT.
This study was approved by the Ethics Committee of Nanjing Brain Hospital (No. 2023-KY043-01) and registered with the Chinese Clinical Trial Registry (Registration No. ChiCTR2300074752).
The demographic information of the subjects is presented in Table 2. Analysis of this data indicated no significant differences between the two groups on the Beck Depression Inventory, Hamilton Depression Inventory, Cognitive Distortions Questionnaire, Short Version of the Difficulties in Emotion Regulation Scale, and CBT Comprehension Questionnaire, as shown in Table 3 (p > 0.05). Besides, during the entire intervention period, no participant reported receiving other therapies or medications, and therefore none of the participants dropped out of the intervention for the above reasons.
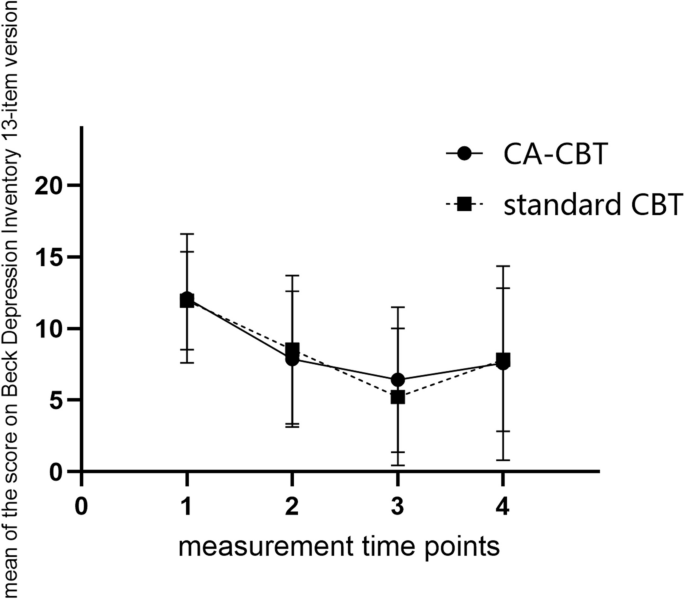
With regard to the Beck Depression Scale total score, time had a significant main effect (ηp2 = 0.37; p < 0.001), whereas more details can be found in Table 5. Similarly, with regard to the Hamilton Depression Scale total score, the effect of time was found to be significant (ηp2 = 0.73; p < 0.001), whereas more details can be found in Table 5. The changes in the total scores of the subjects on the Beck Depression Inventory and the Hamilton Depression Rating Scale are shown in Figs. 2 and 3.
With regard to the Hamilton Depression Scale factor scores, the time effect was found to be significant for Anxiety/Somatization (ηp2 = 0.62; p < 0.001), Cognitive Impairment (ηp2 = 0.60; p < 0.001), and Retardation (ηp2 = 0.69; p < 0.001), whereas the time effect on the weight was not significant. In particular, for the Sleep Disorder subscale, the group effect was not significant, the time effect was significant, and the time x group interaction effect was significant (ηp2 = 0.12; p = 0.031). Subsequent simple effects analysis found that there were no statistically significant differences between the scores of the CA-CBT and standard CBT groups at any of the four time points (p > 0.05). Significant differences were found in the scores of the CA-CBT group between the pre-treatment and mid-treatment timepoint (p < 0.05) and between the pre-treatment and 3-months follow-up timepoint (p < 0.01). The standard CBT group exhibited significant differences between pre- and mid-treatment (p < 0.01), pre-and post-treatment (p < 0.01), mid-treatment and follow-up (p < 0.05), and post-treatment and follow-up (p < 0.01) time points.
There were no significant differences between the two groups’ total scores of BDI at any of the four time points (p > 0.05). A comparison of the Hamilton Depression Scale total scores revealed a significant difference between the two groups only at the follow-up (t(29) = −2.56, p < 0.05, Cohen’s d = −0.93) but not the other three assessment timepoints, as illustrated in Table 3. This, when considered alongside the descriptive data, indicates that the CA-CBT group had significantly lower Hamilton Depression Scale scores than the standard CBT group at the follow-up.
The sample size of the CA-CBT group at the post-treatment stage was 12. Of these, four participants (33.3%) demonstrated a clinically significant improvement, five (41.7%) showed an improvement that was not statistically significant, two (16,7%) showed no significant change, and one (8.3%) experienced a deterioration in depressive symptoms. The sample size of the standard CBT group at post-treatment was 18, of whom seven (38.9%) achieved clinically significant improvement, nine (50.0%) improved but not significantly, one (5.6%) experienced no significant change, and one (5.6%) experienced a worsening of depression. The results of the chi-square test were not statistically significant (χ2 = 0.00, p > 0.05) (see Table 4.)
With regard to the Cognitive Distortions Questionnaire total score and each subscale, time exerted a significant main effect, whereas the other effects were not significant (more details can be found in Table 5).
The total Cognitive Distortions Questionnaire scores of the two groups at the pre-treatment, post-treatment, and follow-up time points were compared using an independent samples t-test. The total scores of the two groups were not significantly different at any of the three time points (p > 0.05) (see Table 3).
Repeated-measures ANOVA was conducted with group conditions as the between-group variable, time as the within-group variable, and the Short Version of the Difficulties in Emotion Regulation Scale total score and each subscale score as the dependent variables. The results showed that, with regard to the total score and each factor score, time exerted a significant main effect, whereas the remaining variables did not (more details can be found in Table 5.) The results revealed no significant differences between the total scores of the two groups at any of the three time points (p > 0.05) (see Table 3.)
Time exerted a significant main effect on the CBT comprehension questionnaire’s total score and each subscale score, more details can be found in Table 5..The results also indicated that the total scores of the two groups diverged to a statistically significant degree solely at the post-treatment (t(28) = −2.44, p < 0.05, Cohen’s d = −0.91). And the CA-CBT group had inferior CBT comprehension questionnaire scores at the post-treatment in comparison to the standard CBT group(see Table 3). No significant differences were observed between the two groups at any of the remaining time points (p > 0.05) (see Table 3).
The scores of the CA-CBT group and the standard CBT group on the three questions regarding treatment satisfaction, the possibility of using CBT again, and the possibility of recommending CBT were compared using an independent samples t-test. The results demonstrated no significant differences between the two groups (p > 0.05) (see Table 3).
The CA-CBT group comprised 21 individuals, of whom 12 completed the treatment program, resulting in a shedding rate of 42.9%. The standard CBT group comprised 20 individuals, of whom 18 completed the treatment program, resulting in a shedding rate of 10.0%. The CA-CBT group thus exhibited a higher shedding rate than the standard CBT group. However, the chi-square test indicated that this difference was not statistically significant (χ2 = 0.00, p > 0.05) (see Table 4.)
The purpose of this study is to determine whether CA-CBT with idioms is more effective than standard CBT in use with college students with depressive symptoms. With regard to the depression scale scores, our findings suggested that both CA-CBT and standard CBT can effectively alleviate depressed symptoms in college students. However, the between-group and interaction effects were not significant, indicating that there was no significant difference in effectiveness between CA-CBT and standard CBT in alleviating college students’ depressed symptoms. Thus, our hypothesis was not supported regards depressive symptom part.
The depressive symptoms at each timepoints were compared between the CA-CBT and standard CBT groups which revealed that subjects in the CA-CBT group had significantly lower Hamilton Depression Scale scores than the standard CBT group at follow-up. This suggests that culturally adapted CBT may be more effective than standard CBT in terms of its long-term effect of alleviating depressive symptoms. These results are consistent with those of a randomized controlled trial conducted by Ward et al. [55] with African Americans. In their experiment, the researchers provided two groups of subjects, all of whom suffered from major depressive disorder, with either a culturally adapted cognitive-behavioral intervention or an un-adapted cognitive-behavioral intervention. The former one incorporated cultural adaptations by integrating African American beliefs, risk factors, preferred coping styles, and clinicians into the intervention. They found that the subjects in the cultural adaptation group had less severe depression symptoms at the three-month follow-up, but the authors did not report any significant differences between the two groups. The reason for the superior long-term outcomes observed in the CA-CBT group may be attributed to the same mechanism described above, namely the brief and readily recallable nature of idioms. In light of these characteristics of idioms, subjects may find it easier to recall the idiom-based treatment content subsequent to the conclusion of the treatment, thereby sustaining the effects of the intervention, including the continued application of acquired CBT knowledge. In a meta-analysis conducted by Benish et al. [7], the cultural adaptation of mythological stories used to explain the creation of illness was found to be a significant contributor to the effectiveness of culturally adapted psychotherapy. Furthermore, they also found that the use of mythological stories was the only moderator of the phenomenon of culturally adapted psychotherapies being more effective than un-adapted therapies (d = 0.21). The main cultural adaptation used in this study was the use of idiomatic stories in the CBT psychoeducational component. This may also partially explain the greater improvement seen in the CA-CBT group over the standard CBT group at follow-up.
A detailed analysis of the Hamilton factor scores revealed that, in addition to a significant main effect of time, there was also a significant interaction effect (group × time) on the Sleep Disturbance score. A further simple effects analysis, combined with descriptive statistics, showed that the CA-CBT group’s average Sleep Disorder score declined significantly from the pre-treatment to mid-treatment and then again at the follow-up. By contrast, the standard CBT group’s score continued to decline, but then exhibited a sudden increase to a level approximately equivalent to that observed prior to treatment at the follow-up assessment. This suggests that subjects in the CA-CBT group experienced sustained improvement in their sleep after the intervention, whereas subjects in the standard CBT group experienced a rebound in sleep disturbances at follow-up. Thus, the effects of standard CBT treatment may not be long-lasting. By contrast, the results of a randomized controlled trial conducted by Zhou et al. [58] with Black women yielded inconsistent results. In this trial, Black women were randomly assigned to receive either standard insomnia cognitive behavioral therapy (CBT), culturally adapted insomnia CBT, or insomnia-specific patient education. At the six-month follow-up, both the standard CBT and culturally adapted CBT groups demonstrated significant reductions in sleepiness scale scores, and both outperformed the education group. However, with regard to the mean decline score, the standard CBT group exhibited a higher mean decline score (−10.0 points, 95% CI, −11.2 to −8.7) than the culturally adapted CBT group (−9.3 points, 95% CI, −10.4 to −8.2). This discrepancy in results may be attributed to the fact that the current study did not adhere to the cultural adaptation methodology used by Zhou et al..Zhou et al. conducted a more comprehensive cultural adaptation, involving revisions to the visual content and the cultural context of insomnia in black women, whereas this study simply introduced the idioms and their allusions. In a separate, single-arm study of Chinese participants [9], culturally adapted CBT for insomnia was also demonstrated to be effective for improving sleep in patients with insomnia disorders. It is regrettable that that study did not include a comparison between culturally adapted CBT and standard CBT.
It is noteworthy that no significant difference was observed on the Beck Depression Scale between the CA-CBT and standard CBT groups at follow-up. However, the mean score of the CA-CBT group was found to be lower than that of the standard CBT group in terms of descriptive statistics. This discrepancy may be attributed to the different methodologies used for the rating of the two scales. The Beck Depression Scale is a self-rated scale, which may result in individuals exaggerating or concealing their symptoms. By contrast, the Hamilton Depression Scale is a physician-rated scale, and thus its results may be influenced by factors such as the rater’s expertise [15]. Furthermore, a comparison of the results of a physician-rated scale and a self-rated scale for patients with major depressive disorder by Lin et al. [27] found that the effect size of the physician-rated scale was greater than that of the self-rated scale. In addition, the physician-rated scale was found to be more sensitive than the self-rated scale to symptomatic and functional changes. A longitudinal study similarly showed that the Hamilton Depression Scale is a more sensitive measure of symptom change than the Beck Depression Scale [12]. These findings may account for the inconsistencies observed between the results for the Hamilton Scale and the Beck Depression Scale in the present study. Moreover, a study by Lambert et al. [24] indicated that the Hamilton Depression Scale is primarily concerned with somatic and behavioral symptoms, whereas the Beck Depression Scale places greater emphasis on subjective symptoms. This discrepancy may have also contributed to the disparate outcomes for the two scales in the present study.
Furthermore, the results of the repeated measures ANOVA and the independent samples t-test indicated that there were no significant differences between the performance of the two groups of subjects on either the Cognitive Distortions Questionnaire or the Short Version of the Difficulties in Emotion Regulation Scale. This may be because the two versions of the intervention program in this study were not sufficiently differentiated. Although no significant difference in improvement was observed between the two groups, a significant reduction in cognitive dissonance was evident in both groups with regard to within-group outcomes. One potential explanation for this is the fact that idioms represent only a minor aspect of the vast Chinese culture, and thus are not necessarily an optimal means of conveying that culture. It is possible that a more comprehensive and thoroughly culturally adapted intervention program, incorporating Confucianism, Taoism, and other elements of Chinese culture might have yielded significantly different results.
The present study did not find that CA-CBT incorporating idioms was superior to standard CBT with regard to acceptance, comprehension, or dropout. The initial proposal to culturally adapted psychotherapy was made with the purpose of increasing the use of psychotherapy by ethnic minorities and those from non-Western countries, with the consideration that culturally non-adapted CBT was underutilized. (Organista et al.; Sue). The results of this study, however, did not support the hypothesis and appear to challenge the necessity of acculturation. Nonetheless, the sample size of the present study was relatively small, and to fully explore this issue would require empirical studies with larger sample sizes to provide more compelling evidence. Moreover, studies have shown that not all individuals require acculturation and that the efficacy of acculturation varies among individuals, with those exhibiting lower levels of acculturation deriving the greatest benefit from it [38, 47]. The subjects in this study belong to the younger group of the population, and thus they may have already been influenced by more Western ideas since childhood and thus did not require as much acculturation. In other words, the effectiveness of acculturation may have been diminished in this population relative to other populations, such as middle-aged and older individuals and those with lower levels of literacy. Moreover, this study exclusively employed idioms for the purpose of acculturation. However, idioms may not be an adequate representation of traditional culture. Consequently, the culturally adapted version of the intervention program may not have been sufficiently differentiated from the standard version, resulting in no significant difference in outcomes.
The sample size of this experiment was ultimately rather small due to the shedding of participants, and thus the results of this study must be interpreted and applied with caution. Since there were only 30 samples included in the statistical analysis, the individual random factors of the subjects may have caused greater interference to the experiment, resulting in certain errors. Alternatively, the small sample size may have rendered the observed effect too small to be significant.
In addition, the subjects in this study were college students with depressive symptoms. As this was a limited group, future studies may consider using other, different populations as intervention subjects. Another limitation of this study is that, although available data from all participants were included in the analysis, outcome measures were only available for participants who had completed the post-intervention assessment. This means that, for example, participants who dropped out before the final assessment still contributed their pre-intervention and mid-intervention data but not their post-intervention data. Therefore, the study results may be affected by the missing data for the final time point, and this could affect the final results. Future studies could consider strategies such as multiple imputation or sensitivity analysis to address the impact of missing outcome data.
Finally, the treatment programs between the CA-CBT and standard CBT groups may not have been sufficiently differentiated by the use of idioms as the sole element of cultural adaptation. When developing culturally adapted intervention programs in the future, consideration could be given to deeper exploration of traditional Chinese ideas, such as Confucianism and Taoism, and attempting to use other cultural vectors, such as poetry, to create treatment programs that are more characteristic of Chinese culture.
In conclusion, this study found that the use of idiomatic adaptations to CBT, as compared to standard CBT, helped college students with depressive symptoms to continue to gain relief for a period of time after the end of treatment. Specifically, there was a trend toward improvement in the total score on the Hamilton scale and its individual factors at follow-up, although that improvement was not statistically significant. However, CBT with idioms was not found to improve subjects’ emotion regulation and understanding of CBT more than standard CBT, nor was it found to correct subjects’ distorted cognitions significantly more effectively. Similarly, the present study did not find that the incorporation of idioms reduced the rate of disengagement from psychotherapy, nor did it improve subjects’ satisfaction, recommendation, or reuse of treatment.
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Not applicable.
There was no financial support for these studies.
All procedures in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee. This study was approved by the Ethics Committee of Nanjing Brain Hospital(No.2023-KY043-01). The participants will be informed about the aims and characteristics of the study. The researchers will clarify any doubts, ensure that the participants have read and understand the information about the study. All recruited participants need to sign the written informed consent after a written and verbal explanation of the study. All participants will be free to withdraw from the research at any time.
Not applicable.
The authors declare no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Lin, C., Hu, M., Xu, J. et al. The role of idioms in reducing depression in university students: a study on group cognitive behavioral therapy. BMC Psychol 13, 618 (2025). https://doi.org/10.1186/s40359-025-02924-5