Tenzing Assisted Delivery of Aspiration (TADA) technique for thrombectomy of medium vessel occlusions using the Freeclimb 54 catheter: multicenter experience
Tenzing Assisted Delivery of Aspiration (TADA) technique for thrombectomy of medium vessel occlusions using the Freeclimb 54 catheter: multicenter experience
- 7 Neuroradiology, OhioHealth, Columbus, Ohio, USA
- 8 Dotter Interventional Institute, Oregon Health and Science University, Portland, Oregon, USA
- 9 Neurosurgery, Cooper University Health Care, Camden, New Jersey, USA
- 10 Neurosurgery and Radiology, Emory University School of Medicine, Atlanta, Georgia, USA
- Correspondence to Dr Fabio Settecase; fsettecase{at}gmail.com
Medium vessel occlusions (MeVOs) account for 25–40% of acute ischemic stroke. The Tenzing 5 (Route 92 Medical, San Mateo, California, USA) and FreeClimb 54 (Route 92 Medical, San Mateo, California, USA) catheter is a novel delivery–aspiration catheter combination designed to facilitate aspiration thrombectomy (AT) of MeVOs. We report our clinical experience using the Tenzing assisted delivery of aspiration (TADA) technique with FreeClimb 54 for first-line AT of MeVO.
We retrospectively reviewed consecutive patients who underwent MeVO first-line AT using TADA with FreeClimb 54 at nine institutions in the USA and one in New Zealand.
94 MeVOs (65 primary, 29 secondary) were treated in 92 patients: median age 71 (IQR 58–81) years; 49/92 (53%) women. FreeClimb 54 was successfully delivered by Tenzing 5 to all 94/94 MeVOs: 26 proximal M2; 44 distal M2; 5 M3; 6 A2; 4 A3; and 8 P2. Median target vessel diameter on DSA was 1.7 (IQR 1.4–1.8) mm. A leading microwire was used to advance Tenzing in 84% of cases. A stent retriever was used for additional thrombectomy passes in 6/94 (6%) patients. For a primary MeVO, final modified expanded Thrombolysis in Cerebral Infarction (meTICI) 2B–3 reperfusion was achieved in 63/65 (97%) patients, after a median of 1 (IQR 1–2) pass, with a first pass effect (FPE, meTICI 2C–3) in 43/65 (66%). Secondary MeVO FPE (eTICI 2C–3) was achieved in 20/29 (69%) patients. Tenzing 5–FreeClimb 54 related complications occurred in 2/94 (2%) patients: one perforation with asymptomatic subarachnoid hemorrhage and one embolus to new territory.
MeVO first-line AT using the TADA technique with Tenzing 5 and FreeClimb 54 had a high FPE with a low complication rate.
Anonymized data that support the findings of this study are available from the corresponding author upon reasonable request.
http://creativecommons.org/licenses/by-nc/4.0/
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Mechanical thrombectomy (MT) has become the gold standard treatment for large vessel occlusion (LVO) stroke,1 with both stent retrievers2 3 and aspiration direct first pass technique (ADAPT)4 showing comparable efficacy and safety.5 6 Primary medium vessel occlusions (MeVOs) of the M2/3 segment of the middle cerebral artery (MCA), A2/3 segment of the anterior cerebral artery (ACA), and P1/2 segment of the posterior cerebral artery (PCA) account for 25–40% of acute ischemic strokes.7 Secondary MeVOs can also occur after initial thrombectomy of an LVO. There is evidence of benefit of mechanical thrombectomy of primary proximal M2 occlusions from LVO trials,1 and meta-analysis of 29 previously published studies suggests a benefit to primary and secondary MeVO thrombectomy.8
In aspiration thrombectomy, the suction force is dependent on inner diameter (ID) for effective clot retrieval.9 Consistent navigation of aspiration catheters to an occlusion, however, remains challenging due to friction through arterial turns, as well as the significant ledge between the catheter and traditional inner microcatheter and/or wire. This is an issue when treating LVOs, and is exacerbated in MeVO thrombectomy by the presence of increased tortuousity and branching at arterial bifurcations, and the smaller caliber medium and distal cerebral arteries, which increase the risk of catheterization failure, dissection, and vessel perforation.10
Building on the recent clinical success of the larger Tenzing 7 and 8 (both tapered tip, ledge reducing catheters) for delivery of large (0.070 inch) and super large (0.088 inch) bore aspiration catheters,11–15 respectively, a novel smaller delivery catheter, the Tenzing 5 (Route 92 Medical, San Mateo, California, USA) was developed. This device is paired with a FreeClimb 54 aspiration catheter (Route 92 Medical, San Mateo, California, USA) with a distal ID of 0.054 inch and a distal outer diameter (OD) of 1.7 mm (table 1). Tenzing 5 and FreeClimb 54 are designed to work in combination to facilitate navigation to MeVO occlusions. In this study, we report our international multicenter experience using the Tenzing assisted delivery of aspiration (TADA) technique for delivering FreeClimb 54 catheters using Tenzing 5. The primary aims were to to evaluate the effectiveness and safety of this device technique in first-line aspiration thrombectomy of primary and secondary MeVOs.
Table 1
Dimensions of the Tenzing 5 delivery catheter and FreeClimb 54 aspiration catheter
The databases of endovascular interventions for acute ischemic stroke at ten high volume stroke centers (nine in the US and one in New Zealand) were retrospectively searched. Patients with secondary MeVOs were treated according to current LVO thrombectomy guidelines. The decision to treat a secondary MeVO in these patients was at the operator's discretion and based on determination that further thrombectomy pass(es) would target secondary MeVOs that supply eloquent brain tissue and were likely to result in improved final reperfusion score. In contrast, endovascular treatment guidelines for primary MeVOs are not established. Patients with primary MeVOs (detected by CT angiography) were treated if the substantial area at risk of infarction but not yet infarcted was evident on CT/CT angiography/CT perfusion, National Institutes of Health Stroke Scale (NIHSS) score at presentation was ≥3, with at least one disabling deficit (extremity weakness, aphasia, or homonymous hemianopsia), regardless of whether they received intravenous thrombolysis. All patients were treated within 24 hours of stroke onset/last known well.
Because the study was observational with retrospective collection of anonymized data and no patient contact, research study consent was not required by participating centers. Data collection and analysis were performed under an institutional review board approved protocol at the corresponding author’s institution (protocol 2.16.17). During the study period, FreeClimb 54 was FDA approved as an intracranial access catheter, not for mechanical thrombectomy; therefore, cases included in this study involve off-label use.
MeVO locations were defined using the same criteria as the EndovaSCular TreAtment to imProve outcomEs for Medium Vessel Occlusions (ESCAPE-MeVO) trial16: M2 segments were defined as vessels beyond the first bifurcation (or trifurcation) of the insular segment of M1. Of note, the proximal M2 segment of the MCA was defined as up to 1 cm distal to the M1 MCA bifurcation/trifurcation, and the distal M2 segment was defined as ≥ 1 cm distal to the M1 MCA bifurcation/trifurcation to the circular sulcus of the insula. A branch off of an M2 segment MCA arising proximal to the circular sulcus of the insula was considered an M3. We categorized MeVO as primary (without proximal LVO), or secondary (proximal LVO with a subsequent remnant distal occlusion or distal embolization present after LVO recanalization). Assessment of whether the target artery would accommodate the OD FreeClimb 54 was left to the individual operator, and involved either operator estimation of artery caliber and/or measurement of the occluded artery on pre-procedure CT angiography, and/or real time caliper measurement using intial DSA. Therefore, we included all patients aged ≥18 years with primary or secondary MeVOs consecutively treated with Tenzing 5 and FreeClimb 54 catheters (table 2) by aspiration thrombectomy as a first line approach.
Table 2
Summary of baseline characteristics, procedural details, and outcomes of patients
Typically, the Tenzing 5 is loaded with a preshaped 0.014 inch microwire and inserted into the FreeClimb 54. After guide catheter placement (0.070 inch ID or larger), the Tenzing 5–FreeClimb 54 catheter combination is advanced as a single unit, leading with the distal tapering tip of the Tenzing 5 (figures 1 and 2, and online supplemental figure 1 and video 1). The microwire can be advanced out of the Tenzing 5, if necessary, to assist with selection of the desired branch artery before Tenzing advancement into more distal anatomy. After the Tenzing enters the desired branch, if the wire had been used for vessel selection, the microwire may be pulled back into the Tenzing, as crossing the clot with the microwire is typically not necessary. Once the distal tip marker of the Tenzing 5 reaches the angiographic limit of contrast (ALOC) of the MeVO, the Tenzing 5 is then pinned, and the Freeclimb 54 catheter advanced over the Tenzing 5 to the ALOC on the roadmap. During this maneuver, we concurrently observe the Tenzing 5 tip movement to ensure that the angiographic limit of contrast is not crossed by the proximal marker of the Tenzing 5. In some cases, subtle back and forth movements of the Tenzing 5 during FreeClimb advancement can assist in reducing the static friction between catheters and vessel wall, and assisting in FreeClimb delivery. Once the FreeClimb 54 catheter reaches the ALOC, Tenzing 5 is removed while allowing the Freeclimb 54 catheter to advance passively into the occluded artery, as the vacuum created by Tenzing 5 removal may assist with clot ingestion.12 Vacuum aspiration is then applied for 2–3 min. The Freeclimb 54 is then slowly withdrawn with care not to dislodge ingested/corked thrombus.
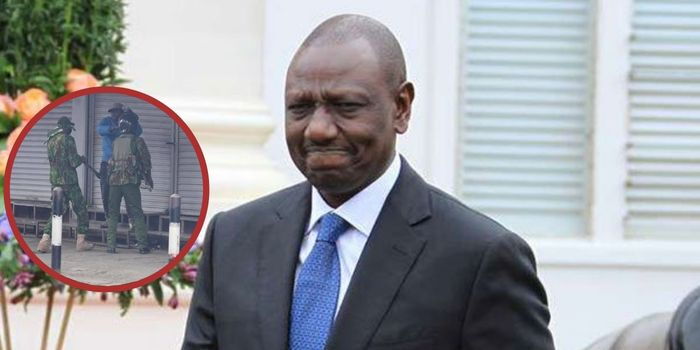
Figure 1
Schematic illustration of Tenzing assisted delivery of aspiration (TADA) technique. (A) Primary medium vessel occlusion (MeVO) in a distal M2 segment. (B) Stagnant blood resulting in thrombus formation at the upstream end of the embolus. (C) Tenzing 5–FreeClimb 54 catheter combination is advanced as a single unit, leading with distal tapering tip of the Tenzing 5. (D) The microwire can be advanced out of the Tenzing 5, if necessary, to assist with selection of the target branch artery before Tenzing advancement into more distal anatomy. (E) After the Tenzing enters the desired arterial branch, if the wire had been used for vessel selection, the microwire may be pulled back into the Tenzing, as crossing the clot with the microwire is typically not necessary. Once the distal tip marker of the Tenzing 5 reaches the angiographic limit of contrast (ALOC) at the site of the MeVO (arrow), the Tenzing 5 is then pinned, and the Freeclimb 54 catheter advanced (arrow) over the Tenzing 5 to the ALOC on the roadmap (F). During this maneuver, we concurrently observe the Tenzing 5 tip movement to ensure that the ALOC is not crossed by the proximal marker of the Tenzing 5. In some cases, subtle back and forth movements of the Tenzing 5 during FreeClimb advancement can assist in reducing the static friction between catheters and vessel wall, assisting in FreeClimb delivery to target. Once the FreeClimb 54 catheter reaches the ALOC, the Tenzing 5 delivery catheter is removed (G) (arrow in FreeClimb catheter) while allowing the Freeclimb 54 catheter to advance passively into the occluded artery, as the vacuum created by Tenzing 5 removal may assist with clot ingestion.12 Vacuum aspiration is then applied to FreeClimb 54 for 2–3 min. The Freeclimb 54 is then slowly withdrawn (H) until either free blood return is observed in the aspiration tubing or if no free blood flow is seen in the tubing during FreeClimb withdrawal (arrow), the catheter is completely removed from the patient.
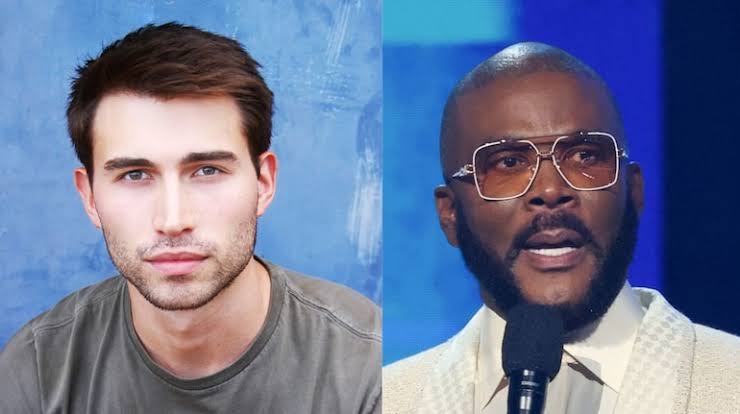
Figure 2
An octogenarian with atrial fibrillation presented with a National Institutes of Health Stroke Scale (NIHSS) score of 8 due to acute right distal M2 occlusion (A) Left Anterior Oblique (LAO) and (B) Schuller’s views showing occlusion of the dominant distal right M2 (red arrows). Tenzing 5 is prepared with a preshaped 0.014 inch microwire, which remains inside the Tenzing 5. The Tenzing 5 is inserted into the FreeClimb 54 (C, D). LAO (E), and Schuller’s (F) fluoro saves of FreeClimb 54 delivered using a Tenzing 5 into the dominant left distal M2 occlusion (online supplemental video 1), with the final position of the FreeClimb 54 after Tenzing 5 removal (G, H). After 2 min of vacuum aspiration, single pass successful recanalization was achieved with final LAO (I) and Schuller’s (J) views showing final modified expanded Thrombolysis in Cerebral Infarction (meTICI) 3 reperfusion. Photo of the removed embolus (K).
Variables extracted were age, sex, comorbidities, NIHSS score, Alberta Stroke Program Early CT Score (ASPECTS) and posterior ASPECTS, procedural details (access site, number of passes, other devices used), complications, and angiographic and clinical outcomes. For cases with secondary MeVOs, angiographic outcomes were based on the extended Thrombolysis in Cerebral Infarction (eTICI) scale.17 For primary MeVOs, angiographic outcomes were based on the recently described modified eTICI (meTICI) scale.18 Angiographic results were locally self-adjudicated with instructions on the use of eTICI and meTICI scales provided to the authors before collecting local data. The modified Rankin Scale (mRS) was used to assess prestroke functional status. Functional independence was defined as mRS ≤2. First pass effect (FPE) and modified FPE (mFPE) were defined as single pass with FreeClimb 54 delivered by Tenzing 5 to the MeVO achieving meTICI ≥2C and meTICI ≥2B for primary MeVOs, respectively. For secondary MeVOs, FPE was defined as a single pass with FreeClimb 54 delivered by Tenzing 5 to the secondary MeVO achieving eTICI ≥2C. Clinical outcome was assessed as the change in NIHSS score from hospital presentation to discharge. Procedural reports, images, and electronic medical records were reviewed for potential complications. Postprocedural hemorrhages were evaluated based on the Heidelberg classification, with symptomatic intracranial hemorrhage (sICH) defined as parenchymal hematoma type 2 with an increase of ≥4 points in NIHSS score.19 Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for reporting observational/cross sectional study were used.20
Ninety-eight patients were identified. Six were excluded due to non-MeVO locations, giving a final cohort of 92 patients, in which a total of 94 MeVOs were treated. Median age was 71 (IQR 58–81) years and 49/92 patients (53%) were women. Comorbidities were hypertension in 66 patients (72%), diabetes in 20 (22%), hyperlipidemia in 52 (56%), and cigarette smoking in 28 (30%). Nineteen (21%) patients were taking anticoagulation medication and 19 (21%) were taking antiplatelet medication(s). Eighty-two patients (89%) had a prestroke mRS score of ≤2 (table 2). Median NIHSS score at admission was 12 (IQR 7–20) and median ASPECTS was 9 (IQR 8–10). Intravenous thrombolytic was administered to 34 (37%) patients.
Access was transfemoral in 89/92 patients (97%) and transradial in 3 patients (3%). There were 65 primary and 29 secondary MeVOs (94 MeVOs total). Freeclimb 54 was successfully delivered over Tenzing 5 to the target MeVO in all 94/94 (100%) patients. The occlusion locations of the primary MeVOs are listed in table 3. The initial proximal occlusion location in secondary MeVOs cases was the ICA in 15/29 patients (52%), M1 in 13/29 patients (45%), and the A1 segment of the ACA in 1/29 (3%). Median target vessel diameter for FreeClimb 54, measured on DSA before thrombectomy, was 1.7 mm (IQR 1.4–1.8). No stent retrievers (SRs) were used for FreeClimb 54 delivery. Intracranial atherosclerotic disease was present in 10/94 cases (11%). A leading microwire was used to direct the Tenzing 5 to the target vessel in 79/94 MeVO cases (84%). The leading microwire was placed beyond the angiographic limit of contrast (ALOC) on roadmap in 52/94 (55%) patients. To better understand operator technique, operators were asked to track the final position of the Tenzing 5 distal and proximal markers relative to the ALOC on roadmap during FreeClimb 54 delivery to the target. Most commonly, the Tenzing 5 was advanced such that the ALOC was in between the proximal and distal markers of Tenzing 5 in 49/94 (52%) (figures 1 and 2, and online supplemental figure 1 and video 1), followed by placement of the distal T5 marker at the ALOC in 23/94 (24%) patients. The distal Tenzing 5 marker stayed proximal to the ALOC during FreeClimb 54 delivery in 2/94 (2%) patients. The proximal marker on T5 was advanced past the ALOC in 10/94 (11%) patients. No response/unknown was recorded for 10 cases (11%). After FreeClimb 54 delivery to the ALOC, on Tenzing removal, the FreeClimb 54 was observed to passively advance in 37/94 (39%) cases.
Table 3
Primary and secondary medium vessel occlusions: comparison of baseline characteristics, procedure details, and outcomes
For primary MeVOs, final meTICI 2B/2C/318 reperfusion and final meTICI 2C/3 reperfusion was achieved in 63/65 (97%) and 80% of patients, respectively, after a median of 1 (IQR 1–2) pass; FPE (meTICI 2C/3) was observed in 43/65 (66%), and a modified FPE (meTICI 2B/2C/3) in 51/65 (78%). Median time from groin puncture to reperfusion for 65 primary MeVO cases was 26 (23–38) min. For secondary MeVOs, after initial LVO thrombectomy passes and before initial FreeClimb 54 pass, all 29/29 secondary MeVOs started with an eTICI score of ≤2B. For secondary MeVOs, FreeClimb 54 FPE (eTICI 2C/3) was achieved in 20/29 (69%) patients and final eTICI 2C/3 was achieved in 25/29 (86%) patients .
A different thrombectomy device was used for subsequent thrombectomy passes in 9/94 MeVO cases (10%) to recanalize the MeVO after one or more unsuccessful Freeclimb 54 passes, including: two cases in which a Trevo (Stryker, Fremont, California, USA) 3×32 mm was used; one case where a RED43 (Penumbra, Alameda, California, USA) was used for thrombectomy in a separate M3 branch occlusion; one case where a RED 62 (Penumbra) delivered by Tenzing 5 also did not result in reperfusion and subsequently a Solitaire 3×20 mm (Medtronic, Minneapolis, Minnesota, USA) was successful; one case of combined Trevo 3×32 mm with a Sofia 5F (Microvention, Tustin, California, USA) for local aspiration; two cases where RED 43 was used with an Aristotle 24 (Scientia, West Valley City, Utah, USA) wire; one case of Trevo 4×20 mm with FreeClimb 70 (Route 92 Medical) for local aspiration; and one case of Trevo 4×41 mm with FreeClimb 70 for local aspiration. A Walrus balloon guide catheter (Q’Apel, Fremont, California, USA) was inflated in 25/94 (27%) cases.
Tenzing 5 and/or FreeClimb 54 device related complications were observed in 2/94 cases (2%): one arterial perforation resulting in transient and asymptomatic subarachnoid hemorrhage (SAH); and one embolus to new territory (after a posterior M2 division MeVO thrombectomy pass, a small clot fragment was noted in an anterior division distal M3). Neither of these two patients underwent additional intervention. Other procedure related complications (3/94, 3%) included a one transient (self-limited) carotid–cavernous fistula related to microwire use before Tenzing advancement; a common femoral artery pseudoaneurysm in one patient; and one non-flow limiting internal carotid artery dissection related to guide catheter use.
Postprocedure, ICH of any type was observed in 23/92 patients (25%) (table 2). Symptomatic ICH occurred in 3/92 patients (3%). Median NIHSS improvement from initial presentation to discharge was 6 (IQR 3–11). Eight patients (9%) died during hospitalization.
Primary and secondary MeVOs were not significantly different regarding age, diabetes, hypetension, prestoke functional independence, intravenous thrombolytic administration, access site, number of MeVO FreeClimb 54 passes, MeVO FPE, any ICH, sICH, or hospital mortality (table 3). Number of women (P=0.01) and balloon guide catheter use (P=0.03) was higher in the primary MeVO cohort. Primary MeVO patients had higher baseline median CT ASPECTS (10 vs 8, P<0.0001) and a lower rate of hyperlipidemia (P=0.04). Mean NIHSS score at presentation was significantly higher in secondary than in primary MeVOs (18 vs 12, P=0.0002). The primary MeVO group had a shorter average groin to reperfusion time (32 vs 51 min, P<0.0001). The secondary MeVO group had a significantly higher number of ACA (21% vs 6%, P=0.03) and lower number of PCA (0% vs 14%, P<0.001) occlusions compared with the primary MeVO group. There was no significant difference in the number of proximal M2 (26% vs 31%) occlusions, distal M2 occlusions (48% vs 45%), or M3 occlusions (6% vs 3%) between the primary and secondary MeVO groups. Balloon guide catheter inflation was higher in the primary MeVO group compared with the secondary MeVO group (35% vs 7%, P=0.03). NIHSS improvement at discharge was significantly higher in the secondary MeVO group than in the primary MeVO group (−10.6 vs −6.8, P<0.0001) (table 3).
Devices used in the intial thrombectomy passes to treat an LVO (in patients with secondary MeVOs) included HiPoint 88/Tenzing 8 (Route 92 Medical) (17/29, 59%), FreeClimb 70/Tenzing 7 (Route 92 Medical) (8/29, 28%), HiPoint 70/Tenzing 7 (Route 92 Medical) (3/29, 10%), FreeClimb 88/Tenzing 8 (Route 92 Medical) (2/29, 7%), Hippo/Cheetah (Q’Apel) (1/29, 3%), Zoom 71 (Imperative Care, Campbell, California, USA) and Trevo (Stryker) (1/29, 3%), and Apro 70 (Medtronic)/Sofia 6 (Terumo Neuro, Tustin, CA)/Vecta 46 (Stryker) (1/29, 3%).
We have reported an international multicenter experience of AT using the novel Tenzing 5 delivery catheter and FreeClimb 54 catheter for 92 patients with both primary and secondary MeVOs. The TADA technique using this catheter combination was highly effective for access to the MeVO in 100% of cases, and for achieving reperfusion with a 66% FPE (meTICI 2C/3) for primary MeVOs, with a low complication rate. Thrombectomy of MeVOs resulted in significant improvement in NIHSS at discharge, with primary MeVOs presenting with lower severity and achieving better discharge NIHSS scores than secondary MeVOs. This study is the first series of patients treated with the novel Tenzing 5 and FreeClimb 54 catheters using the TADA technique.
Since suction force in AT depends in part on the cross sectional area in contact with the clot surface, higher suction forces are expected with larger bore catheters. Smaller catheters are needed, however, to access the smaller caliber ACA, PCA, and M2-M3 segment MCA. A growing body of literature highlights the importance of size matching the aspiration catheter OD to the target vessel ID, which not only maximizes the catheter area in contact with the thrombus but also reduces blood inflow, and potentially reverses blood flow within the target vessel, leading to increased AT pass success rate.21–23 In this study, the median diameter of the target MeVO measured 1.7 (IQR 1.4–1.8) mm, which closely approximates to the FreeClimb 54 OD (1.7 mm). A technical challenge and safety consideration when attempting to closely size match the catheter OD to the target vessel ID in AT is the ability to deliver a relatively large aspiration catheter to the clot interface successfully without vessel injury. This is true for LVOs as well as MeVOs.
The increased tortuousity, number of bifurcations crossed, and the smaller and more fragile nature of the medium sized M2–3/A2–3/P1–P2 arteries compared with M1/ICA/basilar arteries compound the challenge further. A unique solution to this problem is the use of a ledge reducing, self-centering delivery catheter, such as the Tenzing. Several LVO thrombectomy clinical reports have described the efficacy and high delivery rates with both 0.070 inch large bore and 0.088 inch super large bore aspiration catheters using the TADA technique with Tenzing 7 and Tenzing 8, respectively.11 12 14 15 This is the first study of the TADA technique with the novel Tenzing 5, specifically designed to deliver the FreeClimb 54 in MeVO anatomy, showing delivery of FreeClimb 54 in all cases in both anterior and posterior circulation MeVO anatomy.
For LVOs, the efficacy and safety of first line AT has been demonstrated to be non-inferior to SR thrombectomy.5 6 24 Moreover, the first line AT approach may be more cost effective.25 For MeVOs, however, there are fewer studies comparing first line AT versus SRs. Bilgin et al 26 performed a meta-analysis of 1719 procedures (520 AT, 844 SRs, and 355 SR+AT). Final eTICI 2B–3 recanalization and mFPE 2B–3 rates were 83.7% and 54.9% for SR+AT, respectively, 75.6% and 46.0% for SRs, while AT alone had 74.2% and 52.4% rates. The AT group had a functional independence rate of 46.9%, while functional independence rates of the SR and SR+ASP groups were 51.5% and 61.7%, respectively. Another meta-analysis by Barchetti et al of 494 patients with an MeVO (defined as A2–A3, M2–M3, P1–P2) compared AT versus 0.017 inch ID microcatheter compatible SR.27 They found comparable recanalization rates, and ICH and SAH rates, although there was higher functional independence and a lower mortality rate in the AT group.27 In the same study, the final mTICI 2B–3 reperfusion was achieved in 80% distal occlusions using 5MAX, 4MAX, 3MAX, SOFIA 5, and CAT 5 aspiration catheters without dedicated delivery catheters.27 Another study by Vargas et al reported AT of distal occusions using 5MAX, 4MAX, and 3MAX (Penumbra), with eTICI 2b–3 reperfusion of 77.1% without further adjunctive techniques.28 In our study, meTICI 2B–3 reperfusion was achieved in 93.8% of primary MeVO cases solely with Tenzing 5/FreeClimb 54 pass(es) before the use of adjunctive techniques or devices, and 97% overall, and with FPE meTICI 2C–3 of 66%, significantly higher than previously reported MeVO thrombectomy studies. Crossover from first line AT technique to SR+/-AT technique can also be used as a surrogate for thrombectomy efficacy. In this study, crossover to SR thrombectomy after unsuccessful AT with FreeClimb 54 was only 6%, compared with 30% crossover from AT to SR in the ASTER and COMPASS trials for LVO,5 6 and the 31–41% crossover to SR in studies reporting first line AT of MeVO with the 3MAX catheter.29 30
In addition to improved catheter delivery, a unique physical phenomenon occurring with the TADA technique plays an important part in increasing thrombectomy efficacy. The Tenzing delivery catheter is almost completely space occupying within the FreeClimb catheter lumen. When Tenzing is removed from the catheter, a vacuum is created within the FreeClimb catheter deadspace, including at the catheter tip. This vacuum created by Tenzing removal typically causes thrombus and blood downstream of the catheter to become ingested. This ingestion of the thrombus, therefore, can occur before vacuum aspiration is applied at the catheter hub (eg, with a pump or syringe). On close inspection of online supplemental video 1, there is a small amount of contrast in stasis at the site of occlusion (or ALOC) during the navigation of Tenzing and the delivery of the FreeClimb. In the same video, with FreeClimb arrival at the ALOC and with Tenzing removal, the contrast can be seen entering the distal aspect of the catheter shaft. This likely represents ingestion of material immediately downstream of the FreeClimb 54 tip into the catheter. We postulate that this mechanism is an additional advantage of the TADA technique, and may contribute to the high FPE seen in this study. Furthermore, as the thrombus material is ingested into the FreeClimb catheter, the FreeClimb tip often passively advances forward and takes over the space that was formerly occupied by the thrombus within the artery. Passive FreeClimb catheter advancement on Tenzing removal was commonly observed on fluoro in this study. This did not result in significant vasospasm or dissection. Therefore, we advise that operators should not pull the FreeClimb catheter back during Tenzing removal when this phenomenon is observed.
Regarding safety, Bilgin et al 26 reported that SAH rates were lowest for the AT group (1.8%) compared with the SR (9.3%) and SR+AT (11.9%) groups; Barchetti et al reported vessel perforation and SAH in 1.7% of patients after MT, without differences between the AT versus SR technique. In our study, we observed only one case (1%) of perforation with transient SAH, and rates of sICH were similar to previous studies.26 29 The low device related complication rate is worth highlighting, and may not only be due to both the TADA technique and Tenzing 5/FreeClimb 54, but also related to increased FPE and the low number of passes. The inhospital mortality rate in our study (9%) was similar to previous studies in patients who underwent thromboaspiration for LVOs and MeVOs.26 31 None of the deaths were deemed procedure related, occurring in patients with either large core infarcts or with pre-existing co-morbidities.
The efficacy and safety profile of AT using Tenzing 5/FreeClimb 54 was similar for both primary and secondary MeVOs. Secondary MeVOs may occur due to spontaneous clot fragmentation, thrombolytic drug induced fragmentation (eg, post-intravenous alteplase administration), or thrombectomy induced fragmentation.32 As expected, in our study, secondary MeVO patients had greater presenting stroke severity, larger baseline infarct core (lower ASPECTS), longer time to final reperfusion, and higher discharge NIHSS. The absolute change in NIHSS from presentation to discharge was also, as expected, more pronounced in the secondary MeVO group as they started with a higher NIHSS score. We observed similar rates for any ICH and sICH. Despite the high rate of balloon guide catheter use in the primary MeVO group, the MeVO FPE 2C–3 was not significantly different between groups (66% vs 69%, P=0.79).
This study contributes to the expanding literature investigating the use of new thrombectomy devices and techniques for MeVOs.33 34 As we await the results of randomized control trials comparing thrombectomy to medical therapy for primary MeVOs, and future randomized control trials comparing the efficacy of first line MT strategies in MeVO, the applicability of our findings to MeVOs may become more clear in the near future. In the meantime, however, careful consideration is required, as the smaller volume of brain tissue supplied by MeVOs and the potential therapeutic benefit of thrombectomy must be weighed against the risks associated with distal catheterization of these thinner, smaller calibre, more tortuous vessels.10
Our study had several limitations, including the retrospective observational study design with a limited study population and lack of a control group. Another limitation was the absence of long term functional outcomes (90 day mRS) although, in both primary and secondary MeVO groups, we observed improved early clinical outcomes as reflected by their NIHSS shifts. Different management protocols may have been followed across the nine different institutions. Furthermore, patients were treated by highly experienced operators at all centers, thereby potentially reducing the generalizability of study findings. Angiographic and clinical outcomes were self-adjudicated, which may have introduced bias. Although there is evidence highlighting the potential benefit of balloon guide catheters in LVO thrombectomy, only 35% of primary MeVO thrombectomies in this study were performed using a balloon guide catheter. Some caution is advised, therefore, when applying the results of this study to clinical practice.
Aspiration thrombectomy of MeVOs with the novel Tenzing 5 paired with the FreeClimb 54 catheter using the TADA technique resulted in rapid access to MeVOs, high rates of successful recanalization, mFPE and FPE, low complication rates, and high rates of NIHSS improvement at hospital discharge. The 1.7 mm outer diameter of Freeclimb 54 approximated the diameter of the MeVO target vessels, with the ledge reducing effect of the Tenzing 5 facilitating delivery of the FreeClimb 54 catheter in all cases.
Anonymized data that support the findings of this study are available from the corresponding author upon reasonable request.
Not applicable.
This study involves human participants and was approved by the local institutional review boards (IRBs) of the participating centers, with Sutter Health as a coordinating site (IRB approved protocol CPMC021617). Local IRB approvals: UMass-H:00001860; Oregon Health Sciences University-STUDY00026591; Emory-STUDY00000332; Cooper University-22-096; and Northern B Health and Disability Ethics Committee of New Zealand-19/NTB/122. The local IRBs waived the need for patient consent due to the retrospective nature study of patients receiving routine clinical care.
Portions of the data contained in this study were presented at the 21st Annual Meeting and Fellows Course of the Society of Neurointerventional Surgery, July 22-26, 2024, in Colorado Springs, Colorado, USA, as well as at the 16th Congress of the European Society of Minimally Invasive Neurological Therapy, 4-6 September 2024, Marseille, France.