Stakeholders unload big list of nursing home deregulation wishes as CMS deadline hits
Long-term care stakeholders resembled children with plentiful Santa time at Christmas when the Centers for Medicare & Medicaid Services recently asked to hear what rules they would like to see taken away.
Respondents created a flurry of activity up to Tuesday’s submission deadline, sparking suspense over what items federal regulators may eventually eliminate.
Many saw the unusual offer from CMS as a chance to ask for greater efficiencies or modernize processes — and, of course, to request the withdrawal or elimination of the nursing home staffing mandate.
The government billed its request for information “Unleashing Prosperity Through Deregulation of the Medicare Program.”
Provider association LeadingAge unleashed recommendations in 34 topic areas. The association included desired revisions of federal requirements for enhanced barrier precautions and infection control guidance for respiratory illnesses.
“Both create a significant burden on providers, impose on the homelike environment and dignity of residents, and seem to be outdated or ill-advised,” LeadingAge wrote. It noted that the Centers for Disease Control and Prevention’s Healthcare Infection Control Practices Advisory Committee was reviewing the latter request before the committee was dissolved in early May in one of the new administration’s federal worker purges.
LeadingAge also criticized the automatic levying of a 1-star rating for staffing if Payroll-Based Journal workforce information isn’t submitted in a timely enough manner. It reflects a “growing tendency” for the consumer-facing Care Compare website and Five Star Quality Rating System to be used for enforcement purposes, which they weren’t designed for, the association said.
“This arbitrary penalty gives an inaccurate picture of the staffing provided by the nursing home, which might actually be staffing at a 5-star level but simply experienced a technical error preventing timely submission of data,” LeadingAge wrote.
Other key wishes it expressed: more widely implementing the risk-based survey, revising / waiving the ownership / management / additional disclosable parties reporting via the form CMS-855A, and ideas to assist with workforce issues such as modifying the guidance to allow telehealth visits and better delegation of physician services to non-physician practitioners such as physician assistants, nurse practitioners, and clinical nurse specialists.
Stakeholder comments may prove particularly helpful to regulators, who through an executive order have been charged with eliminating 10 rules for every new one introduced.
Not to be outdone by LeadingAge’s 23-page wish list, was the American Health Care Association, which weighed in with a whopping 54 pages of desires. Many reflected the addition of steps or definitions, rather than strictly stripping away regulations.
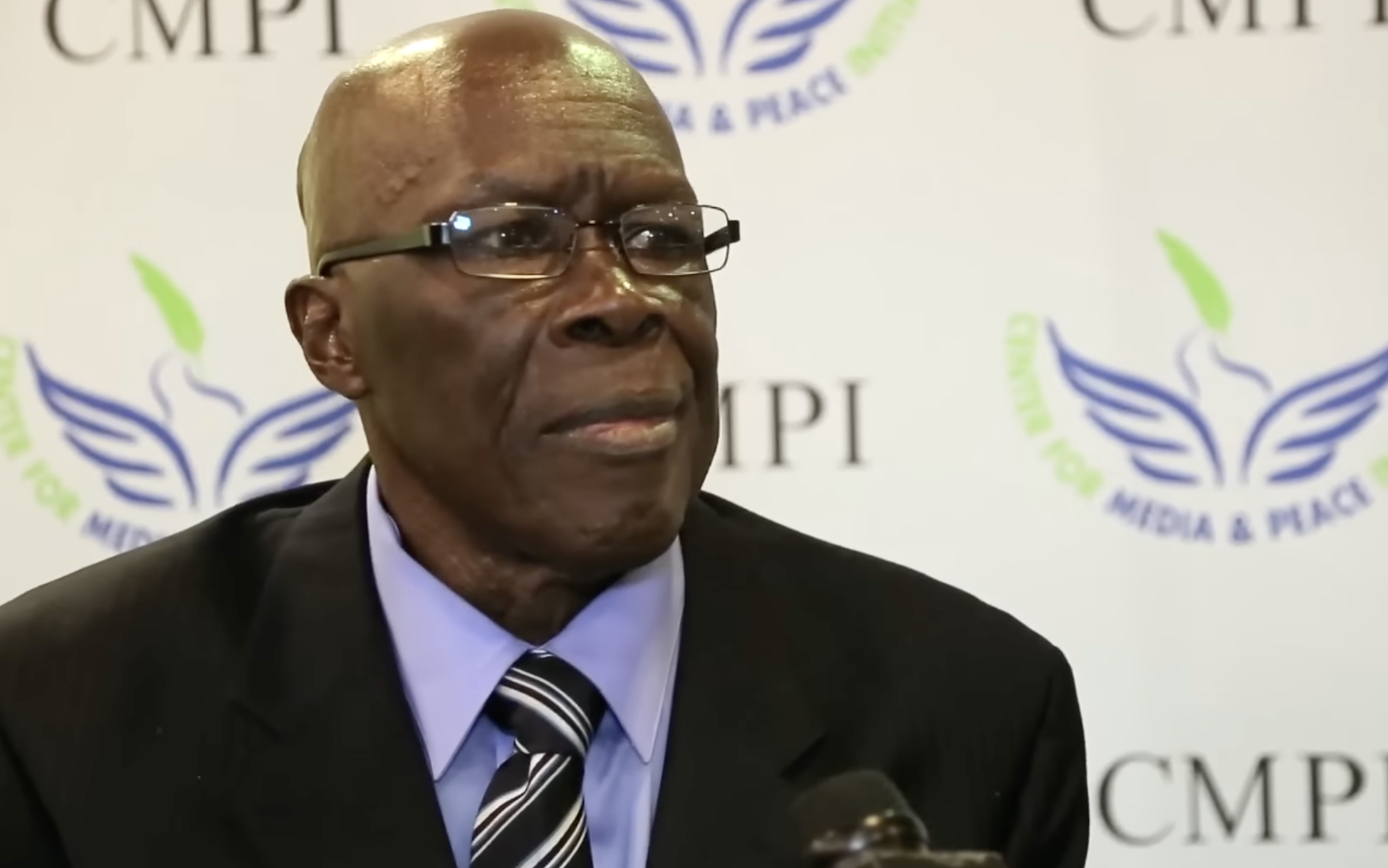
“We have an inconsistent and ineffective oversight system that does not drive quality improvement among nursing homes or enhance the quality of life for residents,” wrote AHCA President and CEO Clif Porter to preface his group’s submission to Health and Human Services Secretary Robert F. Kennedy Jr. “What it does drive is highly qualified and dedicated caregivers out of or away from the long-term care profession, contributing to our sector’s ongoing workforce challenges.”
One of its first requests called for nursing homes to be surveyed not less than every 36 months instead of the current roughly annual cycle, in order to “be consistent with other healthcare settings.” In addition, CMS should expand the risk-based survey process to go nationwide (or at least for the top 20% of performing nursing homes).
The group also recommends that non-physician practitioners be allowed to conduct initial and routine visits and that such work time be recognized in Payroll-Based Journal accounting.
It also wants Appendix PP guidance changes for surveyors that went into effect April 28 of this year to be withdrawn because they are slowing down the survey process and creating unnecessary paperwork.
Among the 10 Five-Star Rating System changes it would like are shifting to 20% allotment at each star rating (currently only 10% are allowed to be 5-star); stopping forced rating downgrades to 1-star as a Payroll-Based Journal audit penalty; and moving to a two-survey cycle, instead of three.
AHCA also seeks numerous revisions to Immediate Jeopardy tagging, including adding “serious” before harm and impairment whenever referring to the definition of Immediate Jeopardy, replacing “reasonable expectation” with “high probability,” and adding a statement to clearly define Immediate Jeopardy.
Another target would be the easing of restrictions on SNFs that have been punished for certain deficiencies to resume certified nursing assistant training programs.
At one point, it also argues for the elimination of measures that report on staff COVID-19 and flu vaccination rates.
Calls for streamlining MDS reporting, standardizing patient data elements and liability standards are also among the dozens of regulatory areas touched on.
The long-term care medical directors group PALTmed made revision of the current three-day rule its first mention. It recommended dropping that hospital-stay requirement to gain SNF Medicare coverage to the two-midnight inpatient admission benchmark for Medicare beneficiaries or the removal of the three-day criteria altogether.
It also called for reinstatement of the requirement that a registered nurse must be included for any complaint or revisit surveys.
Another recommendation is to implement a standardized CMS-endorsed resident and family experience survey similar to one used in hospitals or for Medicare Advantage plans. Results could contribute to a facility’s survey risk score and high-performing facilities could qualify for reduced survey frequency, the physicians suggested.
PALTmed also would like to exempt hospice patients in nursing facilities from CMS regulations in order to reduce redundant steps and administrative tasks.
In addition, the physicians called for simplified Merit-Based Incentive Payment system provisions, partly to help smaller, independent and rural facilities.
Enabling more telemedicine use, providing training to staff and physicians on digital health tools and fostering more pilot programs in rural health facilities also were goals mentioned in PALTmed’s submission.
Massive products and services supplier Direct Supply emphasized bold, technology-enabled changes that “reduce administrative burden and return valuable time back to resident care.”
It recommended CMS focus on embracing digital transformation by:
“SNFs are overburdened by duplicative systems and outdated documentation processes,” said Angela Eslinger, Direct Supply’s vice president of operations and supply chain. “We see this RFI as a chance to modernize healthcare infrastructure and stand with our customers in building a smarter, more sustainable future.”