BMC Complementary Medicine and Therapies volume 25, Article number: 199 (2025) Cite this article
Traditional Chinese medicine (TCM) is widely used by pregnant and breastfeeding women in China, yet predictors of its use intention remain understudied in mainland China. This study applied an extended Theory of Planned Behavior (TPB) framework to identify factors influencing TCM use intention in this population.
A cross-sectional survey was conducted among 264 pregnant and breastfeeding women from diverse regions in mainland China between July and October 2023. Data were collected through an online questionnaire that included demographic information, TPB-based measures (attitudes, subjective norms, perceived behavioral control, intention), and past TCM use experiences. Structural Equation Modeling (SEM) was used to test hypothesized relationships.
The results showed that 37.5% of participants reported using TCM during pregnancy or lactation. The extended TPB model explained 84.5% of variance in intention, with subjective norms having the strongest impact (β = 0.435; p < 0.001), followed by attitudes (β = 0.304; p < 0.001) and perceived behavioral control(β = 0.294; p < 0.001). Past experience with TCM also significantly influenced both attitudes and intentions. The model demonstrated excellent fit (χ²/df = 1.53; CFI = 0.99; RMSEA = 0.04).
This study demonstrates that TCM use during pregnancy and lactation is common in China, and that subjective norms, attitudes, perceived behavioral control, and prior experience are key predictors of intention to use TCM. These findings underscore the importance of integrating cultural and social considerations into healthcare practices. Healthcare providers should be aware of the significant role of family in decision-making and incorporate culturally sensitive counseling into maternal care. Policymakers should strengthen regulatory oversight of TCM to ensure its safe and effective use during pregnancy.
Traditional medicine (TM) represents a critical component of global healthcare, particularly in the prevention and management of chronic conditions and in addressing the health demands of ageing populations [1]. Due to its perceived low cost, alignment with sociocultural, religious and spiritual values, holistic approach to health and well-being, and dissatisfaction with conventional healthcare, interest in TM has resurged [2]. Approximately 80% of the global population is estimated to use TM [3], with usage rates particularly high in low- and middle-income countries [4].
Traditional Chinese medicine (TCM) —which includes herbal medicine, acupuncture, moxibustion, and massage — has been practiced in China for over 2000 years and remains a cornerstone of the national healthcare system. TCM is widely applied in the prevention, treatment, and rehabilitation of conditions such as musculoskeletal injuries, pediatric disorders, gynecological issues, cerebrovascular diseases, and cancers [5]. According to the National Administration of Traditional Chinese Medicine, TCM constitutes approximately 16.8% of China’s healthcare services [6], and has been introduced to 196 countries and regions, reflecting its growing international acceptance.
Women are more likely than men to use traditional medicine [7], and the use of TM during pregnancy is a widespread global phenomenon [8]. Surveys indicate that between 40% and 90% of pregnant women in China use TCM [9], with notable TM usage also reported in Japan [10], Nepal [11], and various regions of Africa [12]. Pregnancy involves profound physiological changes that may lead to maternal or fetal complications [13]. Many pregnant women, particularly in developing countries, often turn to TM due to its accessibility, affordability, limited healthcare access, cultural acceptance, and a perception of enhanced safety compared to conventional treatments [14, 15].
TCM has a long-standing role in pregnancy care among Chinese communities [9, 16], with increasing clinical evidence suggesting its benefits for conditions such as recurrent pregnancy loss [17], infertility [18], and threatened miscarriage [19]. Common TCM practices during pregnancy include herbal remedies (e.g., for morning sickness or back pain), acupuncture for pain relief, moxibustion for breech presentation, and therapeutic massage and cupping. However, TM use during pregnancy has also been associated with adverse obstetric outcomes [20, 21], and many traditional remedies remain insufficiently untested, raising concerns about safety [22, 23]. Given the rising popularity of TCM alongside its potential risks, there is an urgent need for a deeper understanding of the factors influencing pregnant women’s decision-making to ensure its safe and informed use.
Studies have examined the relationship between demographic or obstetric characteristics and TCM use among pregnant or breastfeeding women in Taiwan, Macau, and Hong Kong. For example, Wen et al. [24] found that demographics and pre-existing health conditions predicted Chinese herbal medicine use among pregnant women in Taiwan. Zheng et al. [25] found that 62.6% of lactating women in Macau used traditional or complementary medicine, particularly in response to breastfeeding-related health concerns. However, due to historical reasons, some cultural perspectives vary between Hong Kong, Macau, and mainland China, making it difficult to directly apply findings from these regions. To our knowledge, no study has systematically investigated the predictors of intention to use TCM among pregnant and breastfeeding women in mainland China. This study seeks to fill this gap by exploring these predictive factors.
The theory of planned behavior (TPB) is a widely verified framework for examining health-related behaviors [26, 27]). According to TPB, an individual’s behavioral intention—a key determinant of actual behavior—is influenced by three core constructs: attitude (the individual’s evaluation of the behavior), subjective norms (one’s perceived social pressures to perform or avoid the behavior), and perceived behavioral control (perceived ease or difficulty of performing the behavior). The TPB can be extended by incorporating additional variables such as self-identity, anticipated affect, and past behavior, thereby enhancing its predictive validity. TPB has been effectively applied to maternal health behaviors, including breastfeeding, prenatal screening, healthy eating, and smoking cessation [28,29,30,31]. For instance, studies show that positive attitudes, strong perceived behavioral control, and supportive subjective norms significantly increase women’s intentions to engage in these health behaviors. The framework has also been applied to predict TCM use intention [32]. In a study of TCM users in Hong Kong, Ng et al. [33] applied an extended TPB model and found that attitudes, satisfaction, perceived control, and subjective norms significantly predicted TCM use intention.
Moreover, past behavior has consistently emerged as a critical predictor of intention in maternal health contexts, such as smoking cessation, exclusively breastfeeding, and complementary medicine use during, as it has been shown to predict TCM use [34,35,36,37,38]. For example, Barnes et al. found that women with positive prior experiences of complementary medicine were more likely to continue during pregnancy and lactation. Similarly, Xia et al.’s survey of 10,824 participants revealed that prior TCM use was a significant predictor of future intention (P < 0.001). These findings underscore TPB’s adaptability and relevance across diverse maternal health domains.
This study adopts an extended TPB framework (Fig. 1, adapted from Ajzen [39]) to investigate predictors of intention to use TCM among pregnant and breastfeeding women in mainland China. We hypothesize that positive attitudes, supportive subjective norms, and stronger perceived control over TCM use will be associated with greater intention to use TCM, and that past experiences with TCM will shape both attitudes and subjective norms. By testing these assumptions empirically, the study seeks to validate the extended TPB framework and offer actionable insights for integrating TCM into evidence-based maternal healthcare policy and practice in China.
This was a cross-sectional quantitative study conducted using an online questionnaire administered by obstetrics and gynecology practitioners between July and October 2023. Ethics approval was obtained from the Ethics Committee of Peking Union Medical College Hospital (No.I-24PJ1428, approved on 2023-06-28). All participants provided online informed consent prior to participation.
A convenience sampling approach was adopted to recruit eligible participants. Inclusion criteria were: (1) literate in Chinese and able to understand the questionnaire; (2) provision of informed consent prior to survey commencement; (3) currently pregnant or breastfeeding and aged between 15 and 49 years; (4) could access the internet via smartphones or computer; (5) had used TCM or not before; and (6) residence in mainland China a prolonged period. A sample size of 190 was determined based on the target sample size being 10 times the maximum number of measuring items in the PLS path model [40].
Members of the Maternal and Children Health Management Committee of the Chinese Medicine Education Association, comprising obstetricians and gynecologists from various regions across China, were invited to disseminate the survey to eligible women attending routine clinical appointments. These healthcare providers were located in both urban and rural settings across eastern, central, western, and northeastern China. A total of 20 obstetricians and gynecologists from clinics in eight provinces (Fujian, Beijing, Guangdong, Sichuan, Zhejiang, Shandong, Guizhou, and Jilin) participated in the survey distribution. All participating clinicians were trained via online sessions prior to the launch of the survey. The online questionnaire was hosted on wjx.cn, a widely used survey platform in China [41]. Participants were provided with information about the purpose of the study, the voluntary nature of participation, and assurances of anonymity. They were informed that non-participation would not affect their access to healthcare services. To avoid duplicate entries, only one response per device was permitted. No financial compensation were offered.
The questionnaire was adapted from validated TPB-based instruments and supplemented with new items specific to TCM use. It contained 28 items divided into three sections and required approximately 10 min to complete. Section 1 collected demographic information and background information, including the participant’s maternity stage, TCM usage history (before and during pregnancy/breastfeeding), and a standardized definition of TCM (including herbal medicine, acupuncture, moxibustion, and massage). Section 2 included 19 items measuring TPB constructs (four items each for attitude, subjective norm, perceived behavioral control, and behavioral intention) and three items assessing past experience with TCM. All items were scored on a 7-point Likert scale (1 = ‘strongly disagree’/‘never’ to 7 = ‘strongly agree’/‘always’). Section 3 collected demographic data, including age, gender, education level, economic status, employment status, geographic location and self-reported health status. The complete questionnaire is available in Supplementary File 1.
To ensure content validity, the questionnaire was reviewed by a panel of three experts: an obstetrician, a TCM practitioner, and a health information behavior researcher. Feedback on item clarity, relevance, and cultural appropriateness was also obtained from seven obstetricians and seven pregnant women. A pilot test involving 30 pregnant women at the outpatient department of Peking Union Medical College Hospital was conducted, yielding an average Cronbach’s alpha of 0.9, indicating excellent internal consistency.
Data were analysed using SPSS 22.0 (IBM) for descriptive statistics and reliability assessments, and AMOS 26.0 [42] for structural equation modelling (SEM). Frequencies, percentages, means, and standard deviations were computed to describe participants’ sociodemographic and obstetric characteristics as well as the TPB construct scores. The internal consistency of the measurement instruments was assessed using Cronbach’s alpha, with values ≥ 0.6 considered acceptable and ≥ 0.8 regarded as good [43].
To examine the construct validity in line with TPB theoretical assumptions, Principal Component Analysis (PCA) with varimax rotation was conducted. Factors with eigenvalues greater than 1 were retained and items with loadings above 0.50 were considered significant. Subsequently, Confirmatory Factor Analysis (CFA) was performed to verify the measurement model. Model fit was evaluated using multiple indices: a χ2 /df ratio between 1 and 5, goodness-of-fit index (GFI) and comparative fit index (CFI)>0.90, and a root-mean-square error of approximation (RMSEA)<0.05 [44, 45]. Convergent validity was assessed by calculating the Average Variance Extracted (AVE > 0.50) and Composite Reliability (CR > 0.70) for each construct [46]. Finally, Structural Equation Modelling (SEM) was employed to evaluate the fit of the hypothetical model with the data [47], assessing the relationships between TPB constructs and intention to use TCM. The same fit indices were used to evaluate the overall model fit and path coefficients between variables.
A total of 264 valid responses were included in the final analysis. The majority of participants were from Fujian, Beijing, Guangdong and Sichuan Provinces (84.9%), while the remaining 40 participants (15.1%) were distributed across Zhejiang, Shandong, Guizhou, and Jilin provinces. The demographic characteristics of the survey participants are presented in Table 1.
Most participants (70.8%) were aged between 25 and 35 (with a mean age of 31.0 years), were employed (69.0%), had completed tertiary education (76.9%), reported good health status (60.9%), had no adverse obstetric history (76.9%), reported TCM history before pregnancy (56.1%), and reported no TCM use during pregnancy/lactation (62.5%). There was a relatively even distribution in maternity stage and family monthly income.
Principal component analysis(PCA) was conducted to assess the factor structure of the questionnaire and the contribution of each latent variable to the intention to use TCM. Table 2 shows the reliability and validity results for each construct. The results revealed that all items had outer loadings greater than 0.7. All items exhibited outer loadings above 0.7, and Cronbach’s alpha values exceeded 0.8, indicating strong internal consistency. The AVE for each construct was greater than 0.5, supporting good convergent validity.
Mean scores indicated generally favorable perceptions among participants: attitudes (M = 5.5, SD = 1.1), behavioral intentions (M = 5.0, SD = 1.0), subjective norms (M = 5.0, SD = 1.1), perceived behavioral control (M = 5.2, SD = 1.1), and past experience (M = 4.9, SD = 1.3). These findings suggest that the respondents had relatively positive attitudes, moderate-to-high perceived behavioral control, and satisfaction with prior TCM experiences.
The confirmatory factor analyses show good fit indices for the model, with the values of χ2/df, GFI, CFI, and RMSEA equal to 1.53, 0.96, 0.99, and 0.04, respectively. These values confirm that the measurement model adequately represents the latent constructs.
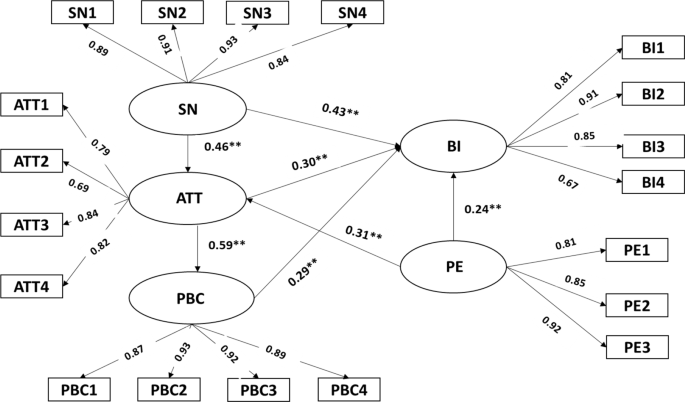
SEM was used to test the relationships among the constructs of the hypothesized model. All path coefficients were statistically significant (p < 0.001), supporting the proposed theoretical model. As shown in Table 3, subjective norms had the strongest direct association with behavioral intention (β = 0.435), followed by attitude (β = 0.304), perceived behavioral control (β = 0.294), and past experience (β = 0.240). In addition, subjective norms (β = 0.459), perceived behavioral control (β = 0.591), and past experience (β = 0.306) were significantly associated with attitudes toward TCM use.
Figure 2. illustrates the results of structural model. All hypothesized paths were supported, suggesting that pregnant and breastfeeding women with more favorable attitudes, stronger subjective norms, and higher perceived control were more likely to express intentions to use TCM. Moreover, past experiences with TCM influence both attitudes toward and intentions, reinforcing its importance as an additional predictive factor in the extended TPB framework.
Structural equation model of the TPB factors and past experience covariate on the intention to use TCM during pregnancy or breastfeeding. Note: ATT Attitude, SN Subjective norms, PBC Perceived behavioural control, BI Behavioural intention, PE past experience
TCM has become increasingly popular among pregnant women in the Chinese population. In our cohort of 264 respondents, the prevalence of TCM use during pregnancy or lactation was 37.5% (n = 99). This rate is higher than reported in Taiwan (11.2-20.9%) and Guangdong (11.2%), but lower than in Hong Kong (55.8%) [48] and Macau (62.6%). These regional differences may reflect variations in cultural practices, healthcare infrastructure, and study methodologies. To address these regional differences, future studies could expand the sample size and include a more representative cohort from additional regions.
Consistent with previous research, we found that demographic variables such as older age, higher educational attainment, and greater family income were positively associated with TCM use intention. Unexpectedly, no significant association was observed between self-rated health status and intention to use TCM, which contrasts with prior studies suggesting that perceived health status influences TCM use during pregnancy and the postpartum period [49]. This discrepancy may be attributed to the fact that most participants in our sample (60.9%) reported good health, thereby reducing variation in this variable. Future studies could include a more diverse sample with varying health statuses to better capture the potential influence of self-rated health on TCM use intention during pregnancy and the postpartum period.
This study contributes novel evidence to the literature by evaluating the utility of the TPB in explaining TCM use intentions among pregnant and breastfeeding women in mainland China. Our extended TPB model accounted for approximately 84.5% of the variance in behavioral intention, indicating strong explanatory power. Among the predictors, subjective norms exerted the most substantial influence, followed by attitudes, perceived behavioral control, and past experience. Furthermore, attitudes toward TCM were shaped by subjective norms, perceived behavioral control, and prior TCM use experience.
Our research revealed that subjective norms -the opinions of important others- was the primary determinants of the intention to use TCM for pregnant or lactating Chinese women. This finding aligns with prior studies in diverse cultural settings. For example, in Iran, subjective norms significantly predicted self-medication with herbal remedies during pregnancy [50]. Similarly, in a focus group study in Norwich, Holst et al. [51] found that asking family and friends was a common way to gain experience with the use of herbal preparations during pregnancy. In Macau, Zheng et al. [26] reported that nearly half 49.8% of breastfeeding women cited recommendation of friends or family as key influences on their TCM use. In collectivist societies such as China, subjective norms are deeply embedded and may be a stronger behavioral drivers than individual attitudes [52]. Pregnancy is often viewed as period of heightened vulnerability, during which women are highly influenced by their social environment. Family members—especially elder women—frequently serve as trusted advisors and decision-makers [53, 54]. In contrast, individualistic cultures tend to emphasize autonomy, wherein healthcare decisions are based more on personal beliefs or professional consultation rather than social conformity. These cross-cultural differences underscore the need for culturally sensitive interventions and interpretations when addressing TCM use in pregnancy.
Health professionals should be aware of cultural differences in decision-making and provide advice that aligns with individual and cultural needs. In China, health professionals, particularly obstetricians, must recognize the strong influence of family and social networks and involve these stakeholders to support informed TCM practices. Moreover, collaboration between Western-trained healthcare providers and TCM practitioners is essential to provide integrated, evidence-based maternal care. Healthcare professionals should be knowledgeable about both conventional medical practices and TCM to guide women effectively. To support clinical decision-making, standardized guidelines should be developed to help professionals balance cultural preferences with maternal and fetal well-being. In addition, educational initiatives should also be introduced to raise pregnant women’s awareness of evidence-based TCM practices, while discouraging unsupervised or unregulated practices. By incorporating these strategies, healthcare providers can play a pivotal role in ensuring that TCM use during pregnancy and lactation is both culturally appropriate and scientifically sound.
Although a meta-analysis identified attitudes as the strongest predictor of health behavior intentions overall [55], our study found that subjective norms exerted a greater influence than attitudes within the Chinese population. Nonetheless, attitudes and perceived behavioral control also significantly contributed to TCM use intention, aligning with both the TPB framework and findings from Hong Kong by Ng et al. [33]. Furthermore, the mean scores for attitudes and perceived behavioral control indicate that this sample of women had relatively positive attitudes toward TCM and a strong sense of empowerment regarding future TCM use.
The role of prior TCM experience was also evident: women with prepregnancy exposure to TCM were more likely to report positive attitudes and stronger intention to use it during pregnancy or lactation. This supports findings from Wen et al. [24] in Taiwan, where prepregnancy Chinese herbal medicine use was associated with use during pregnancy. Favorable past experiences may enhance perceived effectiveness and trust in TCM, reinforcing future use. However, the influence of negative prior experiences remains underexplored. While this study did not specifically measure negative experiences, it is possible that that adverse outcomes or dissatisfaction with past TCM use could reduce intention. Future research should adopt a more nuanced approach by examining how both positive and negative past experiences shape women’s beliefs, attitudes, and intentions. Healthcare providers should consider past TCM experiences when counseling pregnant or breastfeeding women and provide personalized recommendations accordingly. A comprehensive understanding of women’s histories and beliefs will enable more tailored, empathetic, and effective health communication.
To the best of our knowledge, this is the first study to explore the predictors of pregnant and lactating women’s intention to use TCM in mainland China using a TPB framework. This study offers valuable insights for perinatal healthcare professionals, enabling them to better understand the key factors influencing women’s decisions to use TCM. Another notable strength is the broad geographical representation, with participants recruited from various regions across northern, southern, eastern, and southwestern China, ensuring a diverse sample reflective of China’s population.
However, there are several limitations to consider. First, the convenience sampling method used in this study may limit the generalizability of the findings to broader populations of pregnant and breastfeeding women. Future research should employ more rigorous sampling strategies, such as population-based, randomized, or stratified sampling, to enhance representativeness across key demographic and geographic characteristics and validate the current results. Another limitation is the reliance on self-reported questionnaires, which might introduce measurement bias. To mitigate this issue, future research should adopt a mixed-methods approach, combining qualitative interviews with quantitative data to gain deeper insights into the factors influencing pregnant and breastfeeding women’s intention to use TCM. Additionally, longitudinal studies are needed to assess whether the intentions use TCM identified in this study translate into actual behavior and to explore the long-term outcomes, including both positive and adverse effects. Finally, future research should investigate the efficacy of specific TCM practices during pregnancy and breastfeeding to address existing knowledge gaps regarding their risks and benefits.
This study demonstrates that a substantial proportion of pregnant and breastfeeding women in China use TCM and exhibit strong intentions to continue its use. The intention to use TCM was found to be influenced by a combination of personal, obstetric, sociocultural, and experiential factors. Importantly, the TPB proved to be a robust framework for understanding the factors influencing women’ intention to use TCM during pregnancy or lactation in the Chinese population. Among the TPB constructs, subjective norms exerted the strongest influence on behavioral intention, followed by attitudes and perceived behavioral control. These findings emphasize the central role of social and cultural influences—particularly family and community—in shaping health-related decisions among Chinese women.
This research has important implications for maternal and child health practitioners. Healthcare providers should recognize the widespread use of TCM modalities—such as herbal medicine, acupuncture, moxibustion, and massage—during pregnancy and lactation, and be aware of the critical influence of family and social networks in women’s decision-making processes. Integrating culturally sensitive counseling strategies that acknowledge these influences will enhance the effectiveness and acceptability of clinical care. Policymakers should also consider strengthening the regulatory oversight of TCM practices to ensure quality and efficacy, especially for use during pregnancy and breastfeeding, where clinical evidence may be less established. Developing clear, evidence-based guidelines can support healthcare professionals in making informed recommendations and in guiding women toward safe and effective use of TCM. Finally, this study highlights the importance of further research to better understand the specific benefits and potential risks of TCM therapies in maternal populations, as well as their long-term effects on maternal and infant health. Such efforts will be essential for advancing integrative, evidence-informed, and culturally responsive maternity care in China and beyond.
The datasets used and analysed during the current study are available from the corresponding author upon reasonable request.
- TM:
-
Traditional medicine
- TCM:
-
Traditional Chinese medicine
- TPB:
-
Theory of planned behavior
- ATT:
-
Attitude
- SN:
-
Subjective norms
- PBC:
-
Perceived behavioral control
- BI:
-
Behavioural intention
- PE:
-
Past experience
We are thankful for the enduring support and assistance from Professor Zhengbiao Han and PhD candidate Jinglin Qi from the College of Information Management, Nanjing Agricultural University, Nanjing, China.
This study was supported by the Chinese Medicine Education Association (2022KTM029), Science and Technology Project of Beijing (Z231100004623010), the Chinese Academy of Medical Sciences (CAMS) Innovation Fund for Medical Sciences (2021-I2M-1-056), and the Key Laboratory of Medical Information Intelligence Technology.
This study was approved by the Ethics Committee of Peking Union Medical College Hospital(No.I-24PJ1428,2023-06-28). Online informed consent was obtained from all participants prior to their participation in the study. All methods were performed in accordance with the Declaration of Helsinki.
Not applicable.
The authors declare no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Li, Z., Li, J., Lan, Y. et al. Predictors of pregnant and breastfeeding women’s intention to use traditional Chinese medicine: a cross-sectional study from China. BMC Complement Med Ther 25, 199 (2025). https://doi.org/10.1186/s12906-025-04952-5