Journal of Neuroinflammation volume 22, Article number: 149 (2025) Cite this article
Inflammatory bowel disease (IBD), which includes ulcerative colitis (UC) and Crohn’s disease (CD), is characterized by complex aetiological factors and extensive extraintestinal manifestations. Anxiety and depression, which are common mental disorders, have shown increasing incidence rates in recent years. Compared with the general population, IBD patients are more susceptible to anxiety and depression, which consequently exacerbate the disease burden and increases the risk of adverse clinical outcomes. Emerging evidence reveals shared pathophysiological mechanisms between IBD and anxiety and depression. This review rigorously focuses on anxiety and depression in IBD, distinguishing these conditions from primary anxiety or depressive disorders, as well as from mood disturbances secondary to other chronic illnesses, and summarizes the latest research literature highlighting their unique comorbid characteristics. Firstly, we integrate recent epidemiological evidence to establish their bidirectional relationship. Subsequently, we summarize the comorbid mechanisms as follows: genetic predisposition, impaired hippocampal neurogenesis, specific brain region alterations, gut microbiota dysbiosis, hypothalamic‒pituitary‒adrenal (HPA) axis dysregulation and neuroimmune interactions mediated by inflammatory cytokines and neurotransmitters. Finally, we explore novel therapeutic approaches derived from these mechanistic insights, aiming to enhance clinical recognition of this bidirectional comorbidity and optimize the management of such comorbid conditions.
Inflammatory bowel disease (IBD) is a chronic immune-mediated intestinal inflammatory condition categorized into ulcerative colitis (UC) and Crohn’s disease (CD) [1]. The clinical manifestations of IBD include intestinal and extraintestinal features. The intestinal symptoms predominantly include diarrhoea, abdominal pain, and haematochezia. Extraintestinal manifestations most frequently involve the musculoskeletal system, skin, hepatobiliary tract, and eyes [2]. Anxiety disorders account for the most prevalent or frequently diagnosed mental health conditions [3], and depression has emerged as a leading contributor to disability and loss of productive life-years [4]. Epidemiological studies have indicated that IBD patients are more susceptible to psychiatric disorders than are those in the general population [5], and anxiety and depression are among the most common comorbidities [6]. These comorbidities exacerbate the disease burden through increased health care utilization, increased hospitalization risk, emergency department visits, and readmissions [7, 8]. Research suggests elevated risks of depression and anxiety both before and after IBD diagnosis, although the temporal sequence remains unclear due to the limited number of studies [9].
The bidirectional relationship between IBD and anxiety/depression is supported by shared pathophysiological mechanisms (Fig. 1). Genetic susceptibility plays a critical role, as genome-wide association studies (GWASs) have revealed significant genetic correlations between IBD and anxiety/depression traits [10]. Impaired hippocampal neurogenesis has emerged as another core mechanism. Abnormal hippocampal neurogenesis has been observed in animal models of colitis, showing distinct neurogenic changes between acute and chronic colitis models, while conflicting results persisting across various investigations [11, 12]. Furthermore, hyperactivation of the hypothalamic‒pituitary‒adrenal (HPA) axis may induce symptoms of anxiety and depression in individuals with IBD through hormonal and inflammatory signalling pathways. Numerous studies have investigated the influence of the gut microbiota on psychiatric comorbidities in those with intestinal diseases, predominantly attributing this association to gut‒brain axis dysregulation [13, 14]. Studies have shown that microbiota–gut–brain axis dysfunction directly modulates central emotional circuits through reduced short-chain fatty acids (SCFAs) levels, aberrant vagal signalling, and downregulated neuropeptide Y (NPY) expression [15,16,17]. Furthermore, the concept of the gut‒immune‒brain axis involves a stepwise cascade initiated by chronic intestinal inflammation breaching the gut epithelial and vascular barriers, subsequently inducing systemic inflammation and propagating inflammatory signals to the central nervous system [18]. We posit that various inflammatory mediator, neurotransmitters, and structural‒functional alterations in brain regions during neuroinflammation participate in this inflammatory transmission. Given the underdiagnosis of anxiety and depression in many IBD patients, systematic screening and management of these comorbidities remain crucial [19]. This review synthesizes current epidemiological evidence and therapeutic approaches with the aim of providing guidance for predicting and treating neuropsychiatric comorbidities in IBD patients.
Underlying mechanisms of IBD and anxiety/depression comorbidity. This schematic outlines the numerous changes observed in IBD patients with anxiety/depression and in IBD animal models. ↑ indicates an increase in the related process compared to the healthy control group, ↓ indicates the opposite, and -- indicates no significant difference. The figure was created using Figdraw (ID: PSPYUb4000)
Anxiety and depression are common comorbidities in IBD. A recent meta-analysis reported a pooled prevalence of 33.8% for anxiety symptoms and 22.8% for depression symptoms in IBD [20]. Previous studies have found that the prevalence and risk of anxiety and depression in patients with IBD are significantly higher than those in patients without IBD [21] and patients with other chronic conditions [22]. Numerous clinical studies conducted in various countries have yielded similar results [23,24,25,26,, 24, 26, 27]. Meanwhile, several meta-analyses have further confirmed the reliability of this result [28,29,30,31]. Furthermore, a growing body of research suggests that the relationship between IBD and anxiety/depression is likely to be bidirectional. This implies that not only do IBD patients have a higher risk of developing anxiety and depression, but those with anxiety and depression may also be more susceptible to IBD [25, 31]. A number of studies have investigated the bidirectional link between IBD and anxiety/depression, as summarised in Table 1.
Notably, distinct gender differences exist in the prevalence of anxiety and depression among IBD patients, with some studies indicating that female patients exhibit significantly higher susceptibility compared to males [22, 26]. It remains unclear whether the observed gender differences in susceptibility to anxiety and depression arise from IBD-specific mechanisms or inherent sex-related vulnerability, given that females generally have higher baseline susceptibility to these conditions independent of IBD [32, 33]. Additionally, IBD is marked by chronic abdominal pain, which is often linked to anxiety and depression [34,35,36]. Both cross-sectional and prospective studies have shown that pain in IBD patients is significantly associated with increased anxiety and depression [37,38,39]. Pain catastrophizing, a psychological maladaptive coping mechanism associated with exaggerated pain perception, is defined by three core domains: helplessness, rumination, and magnification [40]. Feldman et al. proposed that pain catastrophizing specifically mediates the relationship between abdominal pain and anxiety symptoms [41].
Current clinical research has established a bidirectional association between IBD and comorbid anxiety and depression. Nevertheless, the nature of this association whether it is direct or indirect—the predominant causal direction, and the specific molecular mechanisms involved, remain incompletely understood. Further investigations are needed to thoroughly explore these issues. This will enhance our understanding of the interactions between IBD and anxiety/depression and inform the development of more effective therapeutic strategies.
Research shows that the risk of developing CD and UC is significantly increased in the first-degree relatives (FDRs) of patients with these conditions [42]. Similarly, anxiety disorders tend to cluster in families, with individuals having four to six times higher odds of developing anxiety disorders if they have FDRs with any anxiety disorder [43]. The genetic causal relationship of IBD comorbid with anxiety and depression disorders is even more complex. A study that analysed over 2.19 million Swedish children who were born between 1991 and 2011 and their parents revealed that children of parents with anxiety or stress-related disorders presented a slightly elevated risk of IBD (HR = 1.10, 95% CI = 1.01–1.21) [44]. Undoubtedly, employing clinical cohort studies to elucidate the genetic correlation of the comorbidity between IBD and anxiety/depression is of paramount importance. Nevertheless, as observational studies, clinical cohort studies cannot completely eliminate the interference of confounding factors, and thus, establishing causality difficult. The development of modern sequencing technologies and genomics has provided a strong foundation for exploring genetic associations.
Genetic
The comorbidity of IBD with anxiety and depression has been well documented in both animal models and human patients. However, investigations on the underlying molecular mechanisms remain in nascent stages. Fortunately, the rapid development of sequencing technologies has provided us powerful tools to elucidate this complex relationship at the genetic level.
In animal models, one study used mouse model of DSS-induced colitis and extracted forebrain samples for RNA sequencing. Pathway analysis revealed several enriched terms related to inflammation, including genes associated with the IL-17 signalling pathway, regulation of the inflammatory response, and antimicrobial peptide pathways. Genes such as prostaglandin-endoperoxide synthase 2 (Ptgs2), S100 calcium-binding proteins S100A8/A9, and lipocalin 2 (Lcn2), which are associated with neuroinflammation, were upregulated in the DSS group [45]. Another study performed RNA-sequencing analysis and revealed that Lcn2 was upregulated in the paraventricular thalamic nucleus (PVT) of mice exhibiting DSS-induced depressive behaviours. Moreover, silencing of Lcn2 in the PVT ameliorated DSS-induced depressive-like behaviours [46].
In a clinical study, transcriptomic data from 630 IBD samples retrieved from the Gene Expression Omnibus database were analysed to identify differentially expressed genes (DEGs) that were significantly dysregulated in IBD patients compared with healthy controls, and by cross-referencing these DEGs with 153 depression-associated genes, 33 hub genes with functions that potentially underlie the comorbidity of depression in IBD were identified [47]. Moreover, a clinical study revealed that IBD patients with depressive symptoms exhibited decreased levels of the circadian locomotor output cycles kaput (CLOCK) and nuclear receptor subfamily 1 group D member 1 (NR1D1) genes in their peripheral blood compared with those without mood disturbances [48]. Similarly, several studies have sought to identify molecular markers that are shared by IBD and major depressive disorder through integrative analysis of DEGs, aiming to elucidate the underlying mechanisms contributing to their comorbidity [49, 50]. Nonetheless, these studies can only suggest that these genes might be related to the comorbidity of IBD and anxiety/depression, and much work remains to be done to understand the pathogenic mechanisms underlying this comorbidity.
Genomic
GWASs are a crucial method in genomics research for uncovering genetic correlations, as they can identify associations between sequence variations and phenotypes across the entire genome. Shaw et al. leveraged GWASs to demonstrate robust genetic correlations between IBD and psychiatric-related traits associated with anxiety and depression [10]. Similar study has also revealed a significant positive global genetic correlation between major depressive disorder (MDD) and IBD (P = 1.824 × 10⁻⁵), and bidirectional Mendelian randomization (MR) analyses have shown a unidirectional causal relationship: while genetic susceptibility to IBD does not causally increase the risk of MDD (p = 0.069), reverse causality is significant (p = 0.026) [51]. Another study corroborated these findings, demonstrating that genetically predicted depression was significantly associated with an elevated risk of IBD (OR = 1.20, 95% CI 1.05–1.36), whereas genetic predisposition to IBD or its subtypes showed no causal relationship with the risk of depression in reverse MR analyses [52]. The current synthesis of evidence demonstrates that clinical cohort studies and genetic analyses collectively provide stronger support for the causal influence of depression on risk of IBD, whereas genetic evidence supporting causal pathways from IBD to depression remains comparatively limited. The details of some genetic and genomic studies are summarized in Table 2.
In 1965, Altman and Das first reported on neurogenesis in the adult mammalian brain, a phenomenon now termed adult neurogenesis [53]. Although initially controversial, adult neurogenesis has been robustly validated through extensive investigations [54, 55]. Adult neurogenesis primarily occurs in two regions: the subgranular zone of the dentate gyrus in the hippocampus and the subventricular zone along the lateral ventricles [56]. Adult hippocampal neurogenesis is a multistage process involving the generation of new neurons from radial glia-like stem cells (type 1 RGLs) in the subgranular zone of the dentate gyrus, which develop into intermediate progenitor cells (type 2 cells) and neuroblasts (type 3 cells) before they mature into neurons that integrate into the existing network [57, 58].
Hippocampal neurogenesis and psychiatric disorders
In recent years, significant progress has been made in research on neurogenesis and its relationship with psychiatric disorders such as anxiety and depression [59,60,61]. In rodent studies, research by Hill et al. demonstrated that increasing adult hippocampal neurogenesis is sufficient to reduce anxiety- and depression-related behaviours in a mouse model of stress induced by chronic corticosterone treatment through a mechanism independent of the HPA axis [62]. Further studies have shown that suppressing the excitability of newborn neurons without affecting neurogenesis abolishes the antidepressant effects of fluoxetine. Remarkably, activating these neurons is sufficient to alleviate anxiety- and depression-like behaviour and reverse the adverse effects of unpredictable chronic mild stress. Thus, current research suggests that both neurogenesis and the activity of newborn neurons may be critical factors influencing anxiety- and depression-like behaviours [61]. In nonhuman primates, research by Perera et al. revealed that repeated separation stress in adult female bonnet macaques induces depression-like behaviours (anhedonia and subordinance), which are associated with a reduction in hippocampal neurogenesis, and that treatment with the antidepressant fluoxetine stimulates neurogenesis and prevents the emergence of these depression-like behaviours [63]. Furthermore, neuropathological studies of human brain tissue from patients with MDD have revealed reduced numbers of Nestin+ (a marker of neural stem/progenitor cells) and NeuN+ (a marker of mature neurons) cells, as well as a decreased dentate gyrus (DG) volume [58].
Hippocampal neurogenesis and acute colitis
Previous studies have also reported abnormalities in hippocampal neurogenesis in animal models of IBD. Eloisa Salvo et al. induced acute colitis in mice by administering 2% DSS for 5 days from weaning (P21). Despite acute disease resolution by adulthood (P56), DSS-treated mice exhibited persistent cognitive deficits and anxiety-like behaviours. Immunostaining revealed a reduction in the number of hippocampal DCX + cells (a marker of neuroblasts/immature neurons) in DSS-treated mice, suggesting that impaired neurogenesis may underlie these behavioural deficits [64]. Another recent study reported that DSS-treated mice exhibited reduced hippocampal neurogenesis, manifested by a decrease in DCX + cells and significantly fewer BrdU+/DCX + cells (a marker of newborn immature neurons) in the dentate gyrus [12]. Nonetheless, another similar study showed different results, that acute DSS-induced colitis activated quiescent neural stem cells (Glial Fibrillary Acidic Protein +/Ki67+), increased rapidly proliferating progenitor cells (Sox2+) and neuroblasts (DCX+), thus promoting neurogenesis in the hippocampus [11].
Hippocampal neurogenesis and chronic colitis
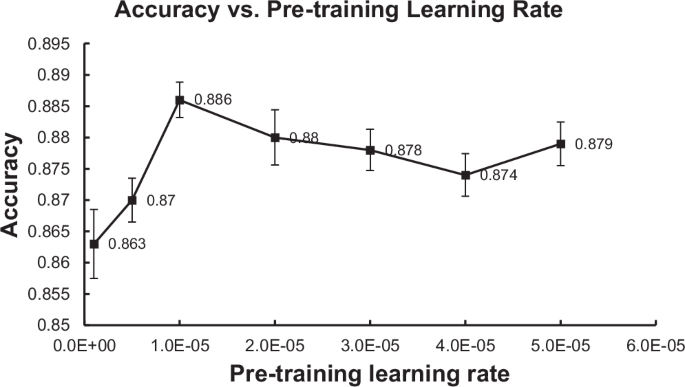
Research on hippocampal neurogenesis in chronic IBD models has also been explored. Research has revealed reduced hippocampal neurogenesis in chronic IBD models, characterized by significantly decreased expression of the neurogenic markers DCX and NeuN. This reduction was accompanied by a weakened positive correlation between colonic ZO-1 tight junction protein levels and hippocampal NeuN expression [65]. Another study indicated that, during chronic colitis, the decline in neurogenesis was mild compared with that in acute colitis, as only the cell compartment labelled with Ki67 was significantly decreased, whereas alterations in the stem/progenitor cell compartment were resolved [57]. In chronic DSS-induced colitis, normal levels of neurogenesis are maintained, but the migration and integration of newborn neurons into the functional circuitry of the dentate gyrus are impaired [11]. The key points of hippocampal neurogenesis research are summarized in Fig. 2.
Hippocampal neurogenesis associated with anxiety and depression in IBD. This figure illustrates recent advances in hippocampal neurogenesis across psychiatric disorders (anxiety and depression) and anxiety/depression combined with IBD, highlighting alterations in neurogenesis and their effects on anxiety- and depression-like behaviours. The left side (orange) primarily showcases research on hippocampal neurogenesis in psychiatric disorders, such as anxiety and depression, across various species. The right side (green) focuses on key findings from hippocampal neurogenesis in IBD animal models, both acute (top right) and chronic (bottom right) colitis. It analyzes the abnormalities in hippocampal neurogenesis and their impact on behavior associated with anxiety and depression in IBD, synthesizing both consistent and conflicting results across studies. ↑ indicates promotion; ↓ indicates inhibition; → indicates the resulting effect. For the abbreviations, refer to the list of Abbreviations
Neurogenesis is a dynamic, multistage process that cannot be fully captured by single-marker analyses. While multiplex immunofluorescence enables simultaneous detection of multiple biomarkers, this approach increases the risks of nonspecific binding and experimental variability. Furthermore, quantitative analysis of immunofluorescence signals requires subjective interpretation during threshold setting and cell counting. These methodological challenges collectively contribute to the observed discrepancies across neurogenesis studies. Unfortunately, owing to the challenges in obtaining brain tissue samples from patients with IBD, there is currently a lack of direct evidence to establish a link between impaired neurogenesis and anxiety and depressive symptoms. Future research should address this gap by developing noninvasive approaches, such as advanced imaging techniques or biomarker analysis, to investigate neurogenesis in living patients.
Prefrontal cortex
Some studies on IBD have shown changes in key brain regions related to psychiatric symptoms. The prefrontal cortex (PFC), a key brain region, regulates cognition and emotion. Research has shown that DSS-induced colitis causes a reduction in the immunoreactivity of Iba-1 and CD68, which are markers of microglia, in the medial prefrontal cortex (mPFC); microglia are the immune cells of the brain and are considered to be associated with a variety of mental disorders [66]. In contrast, mice with 2,4,6-trinitrobenzene sulfonic acid (TNBS)-induced IBD presented visceral pain and depression associated with increased P2Y12 expression in the mPFC. However, the number of cells positive for Iba-1, and the percent area positive for CD68, were significantly increased [67]. Different modelling methods or disease stages may account for the observed discrepancies in microglial changes. However, regardless of these differences, the mPFC does indeed undergo certain changes during the course of IBD, and these changes may be closely related to the pathogenesis of anxiety and depression in IBD. Additionally, abnormal myelination in the PFC is closely associated with IBD-related anxiety and depressive symptoms. DSS-treated mice presented reduced expression of myelin and nodal proteins, as well as impaired formation of the nodes of Ranvier in the PFC. The administration of brexpiprazole, a serotonin modulator, prevented both the DSS-induced depressive-like behaviour and the demyelination in the PFC [68]. Currently, clinical research is focused primarily on functional imaging analysis to reveal the role of functional changes in the mPFC in comorbid anxiety and depression-like behaviours in individuals with IBD. In a study of resting-state functional magnetic resonance imaging (fMRI) data from 222 participants, dynamic functional connectome analysis revealed enhanced cortical stability in the mPFC in the UC group, which correlated with severe depression and anxiety-related measures [69]. Another study used magnetic resonance spectroscopy (MRS) with the MEGA-PRESS sequence with a 3-T scanner to quantify neurotransmitter levels in the mPFC. Compared with healthy controls, IBD patients presented significantly lower concentrations of GABA + and Glx in the mPFC, both of which were negatively correlated with the Hamilton Depression Scale (HAMD) score (GABA+: r=-0.497, p = 0.002; Glx: r=-0.496, p = 0.002) [70].
Insula
The insula is a complex brain region that also plays an important role in emotion regulation [71]. A study analysed the structural magnetic resonance imaging (MRI) results of 57 patients with UC and 40 healthy controls and revealed that UC patients had a reduced grey matter volume in the insula, thalamus, pregenual anterior cingulate cortex, hippocampus/parahippocampus, and other regions [72]. Another study compared high-resolution brain MRI of patients with CD with those of healthy controls and reported that transitivity—a measure of global network segregation—was significantly reduced in CD patients (P = 0.003). Additionally, CD patients exhibited decreased nodal betweenness centrality in the right insula, an alteration that may be associated with anxiety, depression, and other emotional disorders in patients with IBD [73]. One study used glutamate chemical exchange saturation transfer (GluCEST) magnetic resonance imaging to compare glutamate levels in insular subregions between IBD patients and healthy controls. The results showed that the IBD patients had lower GluCEST indices in the left dorsal dysgranular subregion of the insula (p < 0.001, corrected p < 0.05). In IBD patients in remission, these indices were positively correlated with depression scores (FDR-corrected q < 0.05). This finding suggests that GluCEST changes in insular subregions are a brain metabolic feature of IBD and are linked to depression [74]. In addition to the PFC and insula, several other brain regions, such as the cingulate gyrus, precentral gyrus, and supplementary motor area, have been shown to be associated with comorbid anxiety and depression in individuals with IBD [72, 75]. These structural and functional alterations in brain regions collectively contribute to the neurobiological basis of comorbid anxiety and depression in individuals with IBD.
A growing number of studies have demonstrated that there is a complex bidirectional relationship between the gut and the brain, in which the gut microbiota may play an important mediating role [76]. The composition of the gut microbiota in patients with IBD significantly differs from that in healthy individuals. For example, compared with healthy controls, IBD patients present a significantly increased prevalence of proinflammatory bacteria, such as adherent-invasive Escherichia coli, Proteus mirabilis, Klebsiella pneumoniae, and toxigenic Bacteroides fragilis [77], whereas the abundance of beneficial SCFAs-producing bacteria, including Faecalibacterium prausnitzii, Roseburia inulinivorans, and Ruminococcus torques, is notably reduced [78, 79]. Current research has even shown promise in achieving noninvasive and efficient early diagnosis of IBD through detection of the gut microbiota [80]. Similar changes in the gut microbiota, such as an increased abundance of proinflammatory bacterial species, have also been observed in patients with depression [81]. When IBD is complicated by anxiety and depression, what changes occur in the gut microbiota? Studies have shown that, compared with UC patients without depression or anxiety, those with UC and comorbid depression or anxiety exhibit reduced faecal microbial community richness and diversity. They have relatively high levels of Lactobacillales, Sellimonas, Streptococcus, and Enterococcus but relatively low levels of Prevotella_9 and Lachnospira [82].The gut microbiota may mediate the interplay between IBD and anxiety/depression through multiple pathways, including bacterial metabolites, vagus nerve signalling, neuropeptides, and pathogen associated molecular patterns (PAMPs)-pattern recognition receptors (PRRs) interactions.
Bacterial metabolites
SCFAs, which are the key metabolites generated by the gut microbiota from insoluble dietary fibre, mainly include acetate, propionate, butyrate, and valerate, among others [83]. It has been reported that in patients with active IBD, a reduction in SCFAs-producing genera and pathways is associated with depression [84]. In a chronic ethanol exposure study, researchers reported that mice exposed to ethanol presented decreased SCFAs levels and anxiety- and depression-like behaviours. Recipient mice undergoing faecal microbiota transplantation (FMT) from ethanol-exposed donors presented impaired intestinal structure and function, low SCFAs levels, intestinal inflammation, alterations in the GABA system, and anxiety- and depression-like behaviours. Notably, these negative effects were significantly alleviated through SCFAs supplementation [15]. Research suggests that the gut microbiota may modulate depressive-like behaviours induced by chronic ethanol exposure through short-chain fatty acids [15]. Similarly, in another study on methamphetamine-induced depressive- and anxiety-like behaviours, SCFAs supplementation was shown to optimize methamphetamine-induced gut microbiota dysbiosis, improve colonic inflammation, and suppress anxiety- and depression-like behaviours [85]. Additionally, it was discovered that gut microbiota-derived SCFAs could optimize gut homeostasis and ameliorate methamphetamine-induced anxiety- and depression-like behaviours in a manner dependent on the Sigma-1 receptor (SIGMAR1)/BDNF/TRKB pathway [85]. Studies have shown that in animal models of IBD induced by DSS, treatments such as lycopene, rattan pepper polysaccharide, and Lactiplantibacillus plantarum DMDL 9010 (LP9010) can upregulate the levels of SCFAs, improving microbial dysbiosis, intestinal inflammation, and anxiety- and depression-like behaviours [86,87,88]. However, the causal relationships and specific molecular mechanisms involved in the effects of the gut microbiota and SCFAs in IBD combined with anxiety and depression still require further investigation. Other microbial metabolites, such as tryptophan and glycine, have been reported to be closely associated with comorbid anxiety and depression in individuals with IBD, but the underlying mechanisms require further exploration [89,90,91,92].
Vagus nerve
Emerging evidence suggests that vagus nerve signalling may contribute to gut microbiota-mediated mechanisms underlying anxiety and depressive behaviours in individuals with IBD. A study showed that chronic treatment with L. rhamnosus induced region-dependent alterations in GABA mRNA in the brain and reduced stress-induced corticosterone and anxiety- and depression-related behaviours. Interestingly, these neurochemical and behavioural effects were not observed in vagotomized mice, suggesting that the vagus nerve is a major modulatory communication pathway between gut bacteria and the brain [93]. A study revealed that Cholinergic Receptor Nicotinic Alpha 7 (Chrna7) knockout (KO) mice presented depression-like phenotypes. Transplantation of their faecal microbiota into antibiotic-treated mice recapitulated the depression-like phenotypes of the recipient mice. However, subdiaphragmatic vagotomy (SDV) effectively blocked the development of these depression-like phenotypes [94]. According to reports, a small-scale clinical study revealed that chronic vagus nerve stimulation exerts a regulatory effect on anxiety and depressive symptoms associated with Crohn’s disease via afferent vagal fibres [16].
Neuropeptides
In addition to bacterial metabolites and vagal pathways, gut-derived peptides serve as signalling molecules that contribute to the gut microbiota’s ability to regulate anxiety and depression, with particular significance attributed to the NPY family [95]. A previous study demonstrated that Enterococcus mundtii (E. mundtii) is a key microbe that can induce colitis-like symptoms and anxiety/depression-like behaviours in mice, with reduced NPY expression in the colon, plasma, and hippocampus; notably, intraperitoneal NPY administration can alleviate these E. mundtii -induced anxiety/depression-like phenotypes [17]. These studies provide valuable insights into the role of neuropeptides, particularly the NPY family, in the mechanisms underlying how microbiota mediate the interplay between IBD and anxiety/depression. However, further investigation into a broader range of neuropeptides is essential to fully elucidate these complex interactions.
PAMPs-PRRs
PAMPs are conserved structures in pathogens that are recognized by PRRs, such as Toll-like receptors (TLRs) and NOD-like receptors (NLRs), to activate immune responses [96, 97]. Elevated TLR4 expression has been consistently observed in both the brain and colon across murine models of IBD [98, 99]. In the chronic mild stress rat model, intestinal barrier disruption facilitates bacterial translocation, enabling LPS to engage TLR4 and subsequently activate NF-κB and MAPK signaling cascades. Specifically, the p38 MAPK pathway exacerbates neuroinflammation and oxidative/nitrosative stress, ultimately contributing to depression-like phenotypes [100]. Gut microbiota-derived trimethylamine N-oxide (TMAO) may induce depressive behaviours by triggering neuroinflammation via the TLR4/MyD88/NF-κB pathway, as demonstrated in recent studies of methamphetamine-exposed mice [101]. As a pivotal NLR family member, NLRP3 inflammasome activation is observed in the brain of DSS-induced colitis mice, while NLRP3 depletion mitigates DSS-induced neuroinflammation and neurological damage [102]. Furthermore, study has demonstrated Gut microbiota contribute to NLRP3-mediated neuroinflammation and depressive-like behaviours in chronic ethanol exposure models [103]. Collectively, these studies suggest that PAMPs-PRRs pathways represent conserved mechanisms for neuroinflammation and behavioural disturbances, although direct validation of this axis in IBD models with anxiety/depressive-like behaviours remains to be fully elucidated. Future studies specifically interrogating PAMPs-PRRs crosstalk in the neuropsychiatric comorbidity of IBD are warranted to establish causal relationships.
Preclinical evidence
Microglia, derived from early erythroid myeloid progenitors in the yolk sac during embryonic development, are resident macrophages in the brain. Together with astrocytes, which are the most abundant glial cells in the central nervous system, they play a pivotal role in the development of neuroinflammation [104, 105].
In acute IBD animal models induced by DSS, increased Iba-1 protein expression in the CA3 and DG regions of the hippocampus, as well as increased levels of interleukin-1β (IL-1β) and tumour necrosis factor-α (TNF-α) in the serum. Interestingly, correlation analysis indicated that the increase in anxiety- and depression-like behaviours was positively correlated with the elevated levels of serum inflammatory cytokines [106]. Similarly, in mice with DSS-induced acute IBD, significantly elevated levels of pro-inflammatory cytokines (IL-6, IL-1β, and TNF-α) were also found in the anterior cingulate cortex (ACC) and remained high into the remission phase [107]. In a study of chronic IBD mice, the expression levels of inflammatory cytokines such as IL-6 and TNF-α were significantly elevated in colonic tissues, serum, and brain tissues [108]. Spirulina platensis and rhein both possess anti-inflammatory properties [109, 110]. One study developed an oral therapeutic strategy using a Spirulina platensis and rhein hydrogel (SP@Rh-gel), which reduced pro-inflammatory markers and increased anti-inflammatory markers in the hippocampi of mice with chronic colitis, and alleviating anxiety- and depression-like behaviours [111]. A comparison of mice with acute and chronic DSS-induced colitis revealed that both exhibited increased levels of inflammatory cytokines in the hippocampus, but whereas the number of microglia in the hippocampus was significantly increased in mice with acute colitis, the number of astrocytes was significantly increased in mice with chronic colitis [57]. Although these data indicate that the nervous system exhibits different patterns of inflammatory responses in mice with acute and chronic colitis, the presence of neuroinflammation is relatively clear. Multiple studies have suggested that circulating inflammatory cytokines may compromise blood‒brain barrier (BBB) integrity by downregulating tight junction proteins (e.g., claudin-5, ZO-1, and occludin) in cerebral endothelial cells. This increased BBB permeability facilitates the translocation of systemic inflammatory mediators into the brain parenchyma, ultimately triggering neuroinflammation [112,113,114]. However, the more specific mechanisms underlying these processes still need to be further investigated and refined.
Clinical evidence
A small clinical study found that IBD patients with severe intestinal symptoms had higher depression and anxiety scores and elevated inflammatory markers in both intestinal tissues and blood, indicating that active IBD is associated with systemic inflammation and an increased risk of depression and anxiety [115]. Another recent study followed 84 IBD patients (75% with UC and 25% with CD) and reported that baseline C-reactive protein (CRP) significantly predicted follow-up Hospital Anxiety and Depression Scale Depression subscale (HADS-D) scores among individuals with a previous mood disorder diagnosis (β = 0.843, p < 0.001), suggesting that inflammation may be an aetiological trigger for depressive symptoms [116]. TNF-α is an important proinflammatory cytokine. One study revealed that in IBD patients treated with anti-TNF agents, depression scores significantly decreased from baseline (50.1) to week 6 (48.1, p = 0.02) and week 14 (49.4, p = 0.058), although changes in anxiety scores did not reach statistical significance during the same periods [117]. Another study also revealed that anti-TNF treatment improved depressive symptoms in CD patients [118]. Moreover, another relatively large prospective study included 570 IBD patients revealed that anti-TNF treatment significantly improved both anxiety and depressive symptoms within the first 2.5 years and thereafter [119].
While substantial evidence highlights elevated inflammatory cytokine levels as a common feature in comorbid IBD and anxiety/depression, this phenomenon may stem primarily from the inherent inflammatory nature of IBD itself. Whether inflammation and anxiety/depression share a causal relationship remains debatable. For example, a meta-analysis revealed that not all patients with generalized anxiety disorder present elevated inflammatory cytokine levels [120]. A recent randomized controlled trial involving 599 IBD patients demonstrated no association between faecal calprotectin (FCP, an inflammatory marker) and depression, regardless of whether patients were in biochemical remission or a flare [121]. Similarly, a prior prospective study revealed no correlation between FCP/CRP levels and anxiety/depression scores in IBD cohorts [122]. Thus, further research is needed to determine whether inflammatory responses are directly linked to anxiety and depression in individuals with IBD. At the same time, it is necessary to clarify whether anti-inflammatory treatments improve depressive symptoms by alleviating IBD symptoms, which in turn reduces anxiety and depression, or whether the treatments exert a dual protective effect on both IBD and psychological symptoms simultaneously. Therefore, investigating the specific mechanisms by which inflammatory responses lead to anxiety and depression in individuals with IBD is essential. This can help identify more direct therapeutic targets, thereby more effectively alleviating psychological symptoms.
The HPA axis is a complex neuroendocrine system. The hypothalamus releases corticotropin-releasing hormone (CRH), which stimulates the pituitary gland to secrete adrenocorticotropic hormone (ACTH). Once ACTH enters the bloodstream, it prompts the adrenal cortex to produce and release cortisol (CORT). Under normal conditions, the HPA axis maintains cortisol balance through a negative feedback mechanism, where cortisol inhibits the activity of the hypothalamus and pituitary gland, reducing ACTH secretion and thereby regulating its own synthesis and release. This balance helps the body adapt to various internal and external environmental changes, ensuring physiological stability.
In DSS-induced colitis mice, researchers observed that the HPA axis was activated and that α-melanocyte-stimulating hormone (α-MSH) expression was increased. This process promoted the proliferation and differentiation of haematopoietic stem cells into neutrophils, thereby enhancing the clearance of pathogenic microorganisms during the acute phase of colitis while inducing sustained inflammatory responses during the remission phase [123]. The HPA axis plays a significant role in the pathogenesis of depression. Studies have shown that in the unpredictable chronic mild stress (UCMS) model of depression in male rats, UCMS caused a significant increase in corticosterone levels compared with those in the control group (p < 0.001). Treatment with Detarium microcarpum (DM) extract significantly reduced anxiety- and depression-like behaviours, and corticosterone levels decreased in a dose-dependent manner [124]. In some MDD patients, stress-induced hyperactivity of the HPA axis results in long-term elevated glucocorticoid levels, which in turn cause synaptic structural changes and remodelling and disrupt the negative-feedback balance of the HPA axis, both of which are associated with depression [125, 126]. Moreover, anxiety and stress can activate the HPA axis and worsen colitis. Studies have shown that, compared with mice that did not undergo wrap restraint stress (WRS) pretreatment, mice subjected to 7 days of WRS pretreatment developed more severe colitis after receiving a 1% oxazolone enema. Subsequently, the mice were injected with dexamethasone (DEX) to mimic the secretion of CORT induced by HPA axis activation. These mice then received a 1% oxazolone enema and exhibited more significant weight loss and shorter colons. Further investigations revealed that DEX treatment led to increased expression of IL-6 and TNF-α, as well as marked downregulation of the tight junction proteins occludin and ZO-1. Additionally, DEX stimulated group 2 innate lymphoid cells (ILC2s) to secrete more type II cytokines, thereby exacerbating oxazolone-induced colitis. Blocking the IL-13/STAT6 signalling pathway alleviated colitis in mice subjected to WRS and DEX injection [127]. In a TNBS-induced colitis rat model, researchers reported that the concentrations of CRH in the hypothalamus and CRH, ACTH, and CORT in the serum were significantly greater in the TNBS group than in the control group. However, electroacupuncture (EA) treatment significantly improved anxiety- and depression-like behaviours in rats and simultaneously dramatically attenuated hyperactivity of the HPA axis [128]. Studies have shown that in the DSS-induced colitis model, ERβ gene KO mice exhibited exacerbated colitis and anxiety-like behaviours. Further research revealed that ERβ deletion led to increased HPA responsiveness following DSS treatment, suggesting that HPA axis hyperactivity and ERβ may play critical roles in the anxiety-like behaviours observed in IBD [129].
In conclusion, the HPA axis has complex and close interactions with anxiety, depression, and inflammatory bowel disease. However, research on the role of the HPA axis in IBD combined with anxiety and depression, as well as its specific mechanisms, remains limited and is worthy of further investigation.
It is well known that serotonin (5-HT) plays a significant role in the pathogenesis of anxiety and depression [125, 130]. A study revealed that the serum level of 5-HT in IBD patients is significantly greater than that in healthy controls [131]. Moreover, in the UC group, disease flare-ups were not associated with the 5-HT concentration, whereas in the CD group, the 5-HT level was elevated in patients with active CD compared with those in remission. This finding is consistent with previous findings indicating an association between CD severity and the serum 5-HT level [132]. Another animal study demonstrated that DSS-treated mice presented decreased 5-HT levels in the PFC and serotonergic system dysfunction. Brx, a serotonin modulator with partial agonism at dopamine D2 and 5-HT1A receptors and antagonism at 5-HT2A receptors, reversed these changes and prevented DSS-induced depressive-like behaviour in mice. However, Brx did not alleviate colitis-related manifestations. These findings suggest that the improvement in DSS-induced depressive-like behaviour by Brx may be achieved through direct modulation of the serotonergic system and related signalling pathways in the brain rather than indirectly through alleviation of intestinal inflammation. The potential mechanism involves the activation of 5-HT1A receptors, enhancing the ERK1/2-CREB-BDNF-TrkB pathway and regulating myelination in the PFC [68].
By exploring the specific mechanism by which EA relieves anxiety-like behaviours in mice with IBD, researchers have shown that EA could reduce the protein level of cannabinoid type 1 receptor (CB1R) in the ventral hippocampus (vHPC) of mice with IBD treated with TNBS and decrease the percentage of neurons colabelled with CB1R and GABA but that EA had no effect on CB1R expression in glutamatergic neurons. Knocking out CB1R in GABAergic neurons alleviated anxiety in TNBS-treated mice and mimicked the anxiolytic effect of EA [133]. Combined with previous findings that stimulating CB1Rs in GABAergic neurons in the vHPC may reduce GABAergic transmission and lead to anxiety [134], it can be concluded that knocking out CB1Rs in GABAergic neurons can relieve anxiety by regulating neurotransmitter release. In addition, knocking out CB1Rs in glutamatergic neurons led to severe anxiety in wild-type mice, and when EA was given, its anxiolytic effect was inhibited. These findings indicate that CB1Rs in glutamatergic neurons are involved in the anxiolytic effect of EA. EA may exert an anxiolytic effect by activating CB1Rs in glutamatergic neurons, reducing the release of glutamate, and inhibiting the activation of anxiety-related neuronal circuits. In summary, EA may inhibit the activation of anxiety-related neuronal circuits and alleviate the anxiety-like behaviours associated with IBD by downregulating CB1R expression in GABAergic neurons to increase the release of GABA and simultaneously activating CB1R expression in glutamatergic neurons to reduce the release of glutamate [133].
Another study found that in DSS-treated rats, depressive-like behaviours persisted even after the remission of intestinal symptoms, indicating that the depressive-like behaviours were not directly caused by IBD-like symptoms. Additionally, impaired glutamatergic neurotransmission in the ventrolateral periaqueductal grey (vlPAG) was observed, and this impairment was closely associated with sustained depressive-like behaviours in rats. Pharmacological interventions that altered the state of glutamatergic neurotransmission in the vlPAG (either inhibition or enhancement) correspondingly modulated the depressive-like behaviours. These findings suggest that glutamatergic neurotransmission in the vlPAG mediates the relationship between IBD and depression, suggesting that IBD influences glutamatergic neurotransmission in the vlPAG, thereby leading to the emergence of depressive-like behaviours [135].
The comorbidity of IBD with anxiety and depression has attracted increasing attention, and there have been numerous studies on the treatment of IBD comorbid with anxiety and depression. Pharmacotherapy, psychotherapy, and gut microbiota-targeted therapies represent the primary treatment modalities. Additionally, less-studied approaches such as diet and exercise have also shown promise in treating IBD-related anxiety and depression. Several studies have examined the treatment for anxiety/depression in patients with IBD, as outlined in Table 3.
Currently mainstream third-wave psychological approaches, which have evolved from cognitive behavioural therapy (CBT), emphasize improving mental health through strategies such as mindfulness, acceptance, and metacognition [136]. These primarily include acceptance and commitment therapy (ACT), mindfulness-based intervention (MBI), and others [136,137,138,139]. Numerous studies have shown that these therapies have positive effects on anxiety and depressive symptoms in patients with IBD, but their efficacy in improving the disease itself remains controversial.
Among studies on CBT, a meta-analysis demonstrated that CBT significantly reduced anxiety and depression scores and improved quality of life in patients with IBD [140]. A randomized controlled trial revealed that group CBT not only alleviated psychological symptoms but also reduced the Crohn’s Disease Activity Index (CDAI) and CRP levels [141]. A two-armed, parallel-group randomized controlled trial (RCT) revealed that, compared with the standard charity support (SCS) group, the COMPASS intervention group (a cognitive behavioural program for chronic conditions) significantly reduced the psychological distress score by 6.82 points at 12 weeks (p < 0.001). Since the sample included patients with IBD, this finding suggests that this therapy may improve anxiety and depressive symptoms in IBD patients. However, this therapy lacks a specific design targeting IBD [142]. Nevertheless, some researchers argue that CBT has limited efficacy in improving anxiety or stress in patients in remission and can only provide short-term improvement in depression scores [143].
In contrast, the effects of ACT are more pronounced. A randomized controlled trial comparing ACT with CBT reported that ACT significantly improved both anxiety and depression, whereas CBT was only effective for depression [144]. Another study comparing ACT with psychoeducation as a control revealed that the Depression Anxiety and Stress Scale (DASS-21) score significantly decreased in the ACT group [145]. However, findings on the impact of ACT on anxiety and depressive symptoms in IBD patients are inconsistent. A randomized controlled trial involving 122 patients with quiescent or mildly active IBD showed that, compared with the usual treatment group, the ACT group demonstrated significant improvement in depressive symptoms (P = 0.010) but no significant change in anxiety symptoms (P = 0.388) [146]. In contrast, another study involving a one-day ACT intervention designed for IBD patients reported that 79% of participants experienced a reduction in anxiety scores from a baseline of 6.9 to 4.3 at the 3-month follow-up (P < 0.01), whereas depression scores showed only a downwards trend (P = 0.08) that did not reach statistical significance [147]. This discrepancy may stem from differences in intervention duration, disease activity status, or assessment tools, suggesting that the efficacy of ACT in improving anxiety and depression may be influenced by study design and population characteristics.
Recent studies on MBI are relatively limited. A meta-analysis indicated that MBI can reduce CRP levels in IBD patients in the short term but that the improvement in anxiety and depression is not significant [148]. In contrast, a small-sample study revealed that virtual mindfulness-based stress reduction (v-MBSR) therapy could reduce patients’ scores on the Patient Health Questionnaire–Somatic, Anxiety, and Depressive Symptoms Scale (PHQ-SADS) from 11.2 to 6.4 and improve their quality of life scores. Nonetheless, the small sample size (n = 16) and high dropout rate (only 7 people completed the program) limit the reliability of the conclusions [149]. Another meta-analysis revealed that mindfulness interventions have sustained benefits for depression and quality of life but have no significant effects on anxiety or physical disease outcomes [150].
Research conclusions concerning whether psychological therapies can improve IBD conditions are inconsistent. Indicators of IBD conditions include self-reported disease activity indices and objective inflammatory markers. A meta-analysis including 28 RCTs revealed that psychological therapies can reduce the levels of inflammatory markers (such as CRP and faecal calprotectin) (SMD = − 0.455) [151]. However, another meta-analysis including 25 RCTs indicated that psychological therapies had no effect on disease activity indices in patients with quiescent disease (SMD = − 0.01) and did not reduce the risk of disease activity relapse [152]. This discrepancy might arise because the former explicitly stated the exclusion of studies using self-reported clinical indicators, whereas the latter did not clearly specify whether the clinical disease activity measures included self-reported components. Notably, a cohort study of 760 individuals with a follow-up period of up to 6.5 years suggested that IBD patients with active disease and psychological symptoms have a greater risk of disease deterioration [153]. If psychological therapy can only improve anxiety and depressive symptoms but does not contribute to the improvement of IBD itself, then the treatment of comorbidities may require other approaches, such as pharmacological interventions.
The use and applications of antidepressants in IBD have been extensively discussed in multiple papers [154,155,156]. At the level of animal research, paroxetine is acknowledged as a selective serotonin reuptake inhibitor (SSRI). One study revealed that paroxetine can regulate GPCR signalling to affect macrophage polarization, thereby alleviating the symptoms of DSS-induced colitis in mice [157]. Moreover, a recent study revealed that metal-polyphenol, which has antidepressant effects, also has significant efficacy in improving anxiety- and depression-like behaviours in colitis model mice [158].
Additionally, in a prospective, randomized, double-blind, placebo-controlled clinical trial, participants who were diagnosed with IBD and experienced symptoms of anxiety or depression were randomly assigned to receive either venlafaxine (a serotonin-norepinephrine reuptake inhibitor [SNRI] antidepressant) or an equivalent placebo and were followed for 6 months. The study revealed that venlafaxine not only significantly reduced HADS scores (anxiety: p < 0.001, depression: p < 0.001) but also had positive effects on IBD activity and serum inflammatory factor levels after 6 months [159]. A meta-analysis including 13 studies with 884 individuals also revealed that antidepressants not only were superior in reducing depression scores [95% confidence interval (CI): -1.009 -0.572; p < 0.001] and anxiety scores (95% CI: -1.203-0.552; p < 0.001) but also improved disease activity scores (95% CI: -0.500 -0.145; p < 0.001) [160]. In a large epidemiological study of 403,665 patients, patients with a history of depression were found to have an increased risk of IBD; Notably, this increased risk seemed to be mitigated by the use of antidepressants in the treatment of depression [25].
Do usual treatments such as immunosuppressive and biological agents, without any antipsychotic intervention, improve anxiety and depressive symptoms in patients with IBD? Ustekinumab is a monoclonal antibody that targets IL-12 and IL-23 and is used for treating IBD. Two randomized controlled trials have shown that ustekinumab can improve anxiety and depressive symptoms and relieve IBD-related indicators in patients with moderate-to-severe active CD [161, 162]. Similarly, studies have found that both vedolizumab and anti-TNF biologic therapies (infliximab or adalimumab) can also improve the symptoms of anxiety and depression in patients with CD and UC [117, 163]. One recent meta-analysis revealed that depressive symptom scores were significantly lower after IBD treatment without any antipsychotic intervention (SMD = 0.500; 95% CI: 0.207–0.793; P = 0.001), whereas the improvement in anxiety was not 95% CI significant (SMD = 0.083; 95% CI: -0.120, 0.285; P = 0.425) [164]. Overall, anti-IBD treatments have demonstrated certain positive effects in alleviating emotional disorders related to IBD. Nevertheless, there are subtle differences among studies in terms of the extent to which anxiety or depressive symptoms are improved. These differences may be related to multiple factors, including sample size, specific treatment regimens, and the underlying pathogenesis of anxiety or depression itself.
The concept of probiotics, which has a long history, has recently garnered increased attention for its potential therapeutic effects on anxiety and depression, particularly in the context of the gut–brain axis [165, 166]. As defined by the International Scientific Association of Probiotics and Prebiotics (ISAPP), probiotics are “live microorganisms that, when administered in adequate amounts, confer a health benefit on the host”; prebiotics are “a substrate that is selectively utilized by host microorganisms, conferring a health benefit”; and synbiotics are “a mixture comprising live microorganisms and substrates selectively utilized by host microorganisms, which confers a health benefit on the host” [167,168,169]. Numerous animal studies have demonstrated that probiotics mitigate colitis and anxiety/depression-like behaviours in various murine models of colitis [170,171,172,173], but there have been relatively few related human studies. A review by Hassan et al. summarized clinical trials on probiotics for IBD up to 2022, indicating that probiotics can reduce IBD-related depression and improve overall mental health [174]. Another recent study revealed that the probiotic BBG9-1 can improve anxiety scores in patients with quiescent CD [175]. Although prebiotics and synbiotics have shown potential in treating anxiety and depression [166, 176], their direct effects on IBD-comorbid anxiety and depression remain unclear. Interestingly, some bacteria that are considered probiotics, such as Enterococcus faecium and Pediococcus acidilactici, may worsen anxiety and depression in IBD patients when they overgrow in an imbalanced manner [177].
More large-scale RCTs are needed in IBD patients with anxiety and depression. Comparisons can be made between probiotics alone and in combination with other drugs. In addition, details such as the optimal dosage and duration need to be determined. Notably, probiotic engineering represents an innovative strategy. For example, a study loaded a carbon monoxide/hydrogen sulphide-releasing copolymer with the probiotic Escherichia coli Nissle 1917, which reduced neuroinflammation and IBD symptoms and alleviated anxiety- and depression-like behaviours in IBD mice [178].
Compared with probiotics and prebiotics, FMT represents a more aggressive intervention due to the holistic transplantation of the entire gut microbiota rather than specific bacterial strains. A study revealed that faecal microbiota transplants from patients with inflammatory bowel disease and depression induced anxiety and depression-like behaviours in mice. Notably, when these mice underwent FMT from healthy volunteers, the depression-like behaviours were significantly reduced [179]. A prospective clinical study involving 272 UC patients demonstrated that, compared with a placebo, FMT significantly reduced anxiety and depression scores. The participants underwent three FMT sessions via gastroscopy at 3-week intervals using microbiota from sex-matched, healthy adolescent donors. FMT not only improved gastrointestinal symptoms (e.g., diarrhoea, abdominal pain) but also decreased self-rating anxiety scale and self-rating depression scale scores, suggesting that FMT may mitigate anxiety/depression in IBD patients [180]. Another small-scale clinical study has shown that FMT also provides similar benefits in improving depressive symptoms in IBD patients [181]. Although clinical data remain limited and large-scale RCTs are lacking, these recent findings highlight an interesting research direction for the role of the microbiota in patients with IBD and comorbid anxiety and depression.
Several complementary therapies can complement the primary interventions discussed above. For example, DuBois et al. reported that an anti-inflammatory diet and increased physical activity (PA) are associated with decreased anxiety and depressive symptoms in UC patients [182], highlighting the therapeutic potential of diet and PA for IBD-comorbid psychological disorders. These interventions exhibit therapeutic potential for patient with IBD as well as anxiety and depression.
With respect to PA, Sciberras et al. reported that IBD patients with higher anxiety/depression scores were more likely to be sedentary (p < 0.05) [183]. A Chinese cross-sectional study indicated that sedentary behaviour might lead to depression (p = 0.006) in CD patients, whereas moderate-intensity recreational PA could improve anxiety and depression (p < 0.05) [184]. In a US study, 430 adult IBD patients were divided into low, moderate, and high clusters based on their PA. The cross-sectional analysis revealed that those in the low-activity cluster had the worst depression scores (P = 0.004). Longitudinal analysis further revealed that transitions between activity clusters correlated with changes in disease activity scores. For CD patients moving from moderate to high activity, the Short Crohn’s Disease Activity Index decreased by 25.3 on average (P = 0.04), suggesting that increased PA may benefit psychological well-being, including anxiety and depression, in individuals with IBD [185].
In terms of diet, Di Giorgio et al. proposed that the high prevalence of anxiety and depression in individuals with IBD may lead to orthorexia—an evolution from healthy eating beliefs into an obsessive and harmful pursuit of “pure” food [186]. A UK study of 1,576 IBD patients reported strong associations between anxiety/depression and food-related quality of life (FR-QoL) (Pearson’s r = − 0.52, p < 0.001), with poorer FR-QoL linked to lower fibre intake [187]. A recent study reported a negative correlation between anxiety/depression scores and daily fibre intake in patients with IBD [188]. Animal studies have demonstrated that fibre can mitigate gut inflammation in IBD models [189, 190]. Research in humans has revealed that increased fibre intake is associated with decreased odds of depression [191] and is negatively correlated with anxiety and depression outcomes [192]. However, the efficacy of fibre intake for anxiety and depression in patients with IBD remains unconfirmed in human studies. Given that animal studies have indicated that sex [189] and dosage factors might affect fibre effectiveness or even exacerbate anxiety [193], future research should explore dose‒responses and sex-based differences in human trials to optimize therapeutic outcomes.
Other approaches, such as sleep improvement and noninvasive brain stimulation, show promise for treating anxiety and depression [194,195,196,197], yet evidence in IBD populations is lacking. Notably, one study reported no associations among diet, PA, sleep duration, or anxiety/depression in IBD patients during the COVID-19 pandemic (all p > 0.05), possibly due to the pandemic’s unique context [198]. Overall, these complementary therapies may assist in managing comorbid IBD and anxiety/depression, and further large-scale, well-designed RCTs are needed.
The bidirectional relationship between IBD and anxiety/depression stems from a complex network involving genetic predisposition, dysregulation of the microbiota‒gut‒brain axis, and neuroimmune interactions. Preclinical models have shown that neuroimmune dysregulation and gut microbiota disturbances are core mechanisms behind these comorbidities. However, the existing evidence is largely confined to animal studies. There is an urgent need for large-scale, randomized, controlled clinical trials to validate their translational relevance in humans. Many observed associations and mechanisms are mutually causal. For example, gut microbiota dysbiosis can induce anxiety and depression, which in turn further alter the composition of the gut microbiota. Intestinal inflammation can cross the blood‒brain barrier to induce neuroinflammation, which then exacerbates peripheral inflammation through glial cells and proinflammatory factors. Future research should prioritize the use of multiomic technologies to elucidate the temporal sequence of causality and employ organoid models or gene-editing tools to precisely intervene in potential key targets. Clinically, integrating psychological screening into routine IBD management can reduce the underdiagnosis of psychiatric symptoms, particularly in high-risk subgroups. By combining mechanistic exploration with therapeutic innovation, we have the potential to disentangle the suffering caused by both intestinal inflammation and anxiety/depression in patients with IBD, ultimately improving their overall prognosis.
No datasets were generated or analysed during the current study.
- IBD:
-
Inflammatory bowel disease
- UC:
-
Ulcerative colitis
- CD:
-
Crohn’s disease
- HPA:
-
Hypothalamic-pituitary-adrenal
- GWASs:
-
Genome-wide association studies
- MR:
-
Mendelian randomization
- DG:
-
Dentate gyrus
- RGLs:
-
Radial glia-like stem cells
- Sox2:
-
SRY-box 2
- DCX:
-
Doublecortin
- GABA:
-
Gamma-aminobutyric acid
- NeuN:
-
Neuronal nuclei antigen
- CORT:
-
Corticosterone
- DSS:
-
Dextran sodium sulfate
- P:
-
Postnatal day
- ACC:
-
Anterior cingulate cortex
- BBB:
-
Blood-brain barrier
- ZO-1:
-
Zonula occludens-1
- CRP:
-
C-reactive protein
- SP@Rh-gel:
-
Spirulina platensis and rhein hydrogels
- LPS:
-
Lipopolysaccharide
- IL-1β:
-
Interleukin-1β
- TNF-α:
-
Tumor necrosis factor-α
- HADS-D:
-
Hospital Anxiety and Depression Scale-Depression
- CRH:
-
Corticotropin-releasing hormone
- ACTH:
-
Adrenocorticotropic hormone
- DEX:
-
Dexamethasone
- ILC2:
-
Group 2 innate lymphoid cells
- STAT6:
-
Signal transducer and activator of transcription 6
- TNBS:
-
2,4,6-trinitrobenzene sulfonic acid
- EA:
-
Electroacupuncture
- ERβ:
-
Estrogen receptor beta
- 5-HT:
-
Serotonin
- Brx:
-
Brexpiprazole
- CB1R:
-
Cannabinoid type 1 receptors
- vHPC:
-
Ventral hippocampus
- vlPAG:
-
Ventrolateral periaqueductal gray
- CBT:
-
Cognitive behavioral therapy
- ACT:
-
Acceptance and commitment therapy
- DBT:
-
Dialectical behavioural therapy
- MBI:
-
Mindfulness-based intervention
- CDAI:
-
Crohn’s Disease Activity Index
- SCS:
-
Standard Charity Support
- COMPASS:
-
Cognitive behavioral program for chronic conditions
- DASS-21:
-
Depression Anxiety and Stress Scales-21
- v-MBSR:
-
Virtual Mindfulness-Based Stress Reduction
- PHQ-SADS:
-
Patient-Health Questionnaire–Somatic, Anxiety, and Depressive Symptoms Scale
- SNRI:
-
Serotonin-Norepinephrine Reuptake Inhibitor
- AAV:
-
Adeno-associated virus
- CLOCK:
-
Circadian locomotor output cycles kaput
- NR1D1:
-
Nuclear receptor subfamily 1 group D member 1
- BDI:
-
Beck Depression Inventory
- CRGs:
-
Cuproptosis-related genes
- DLD:
-
Dihydro lipoamide dehydrogenase
- DLAT:
-
Dihydrolipoyl transacetylase
- DLST:
-
Dihydrolipoamide succinyl transferase
- PDHB:
-
Pyruvate dehydrogenase E1 subunitβ
- DBT:
-
Dihydrolipoamide branched chain transacylase E2
- LIAS:
-
Lipoic Acid SLC31A1, Synthetase; solute carrier family 31 member 1
- SCO2:
-
Synthesis of cytochrome C oxidase 2
- CDKN2A:
-
Cyclin-dependent kinase inhibitor 2 A
- WGCNA:
-
Weighted gene co-expression network analysis
- PPI:
-
Protein-protein interaction
- HGF:
-
Hepatocyte growth factor
- SPARC:
-
Secreted protein acidic and rich in cysteine
- ADAM12:
-
Protein 12 with integrin and metalloproteinase domains
- MMP8:
-
Matrix metalloproteinase 8
- GWAS:
-
Genome-wide association study
- RCT:
-
Randomized controlled trial
We thank Figdraw (www.figdraw.com) for the assistance in creating figures.
This work was supported by project grants from the National Natural Science Foundation of China(Code: 82301644)and the Wuhan University Zhongnan Hospital Science and Technology Innovation Cultivation Fund(Code: CXPY2023021).
Not applicable.
Not applicable.
The authors declare no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Luo, K., Zhang, M., Tu, Q. et al. From gut inflammation to psychiatric comorbidity: mechanisms and therapies for anxiety and depression in inflammatory bowel disease. J Neuroinflammation 22, 149 (2025). https://doi.org/10.1186/s12974-025-03476-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12974-025-03476-6